PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
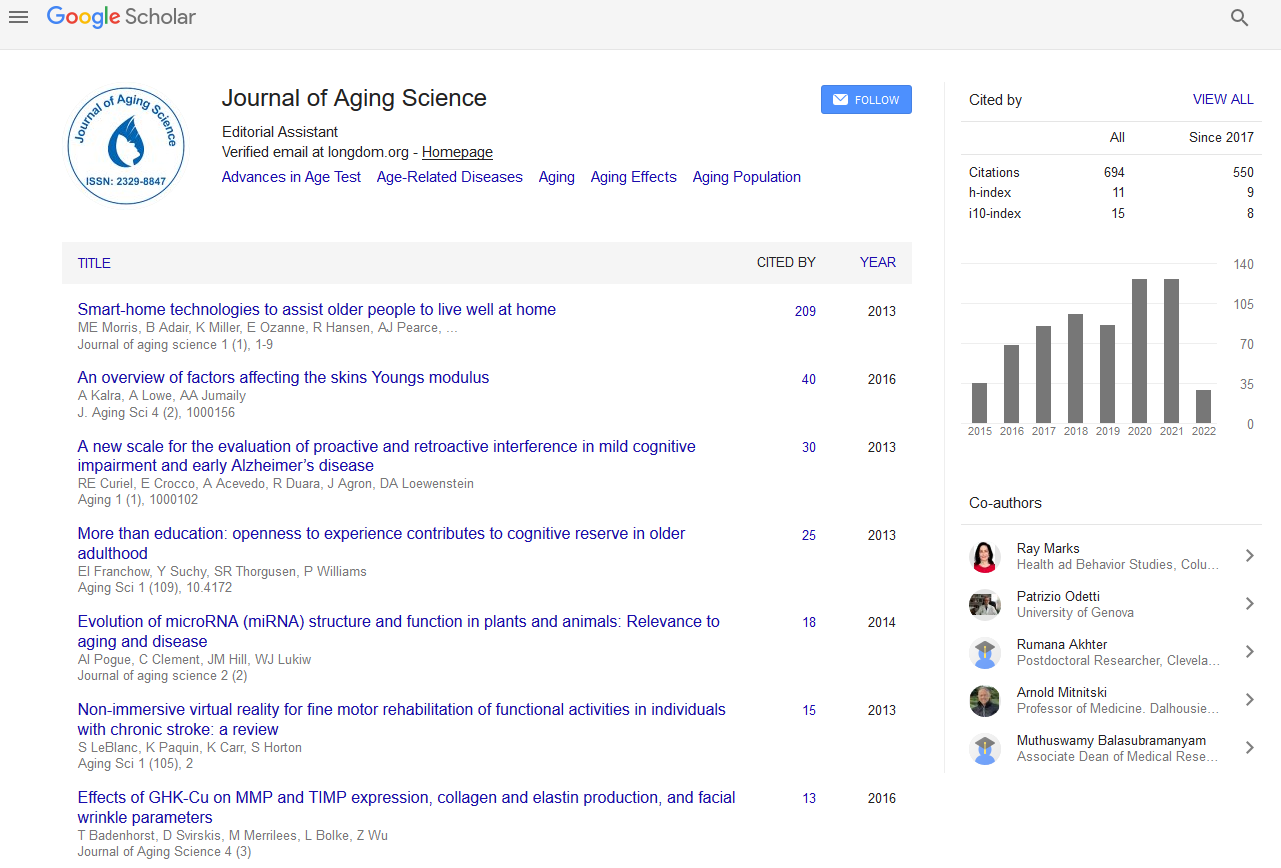
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2019) Volume 7, Issue 3
Prevalence of Frailty among Older Surgical Patients
Roberto Accardi1*, Silvia Ronchi1, Matteo Cesari2, Emanuela Racaniello1, Elena De Rosa1 and Dario Laquintana12Department of Clinical Sciences and Community Health, Milan, Italy
Received: 09-Dec-2019 Published: 30-Dec-2019
Abstract
The increase of hospital admissions for surgical interventions in subjects aged 65 years and older has raised interest among surgeons about the concept of frailty. The aim of this study is to estimate the prevalence of frailty in a sample of older patients admitted to the surgical departments.
Frailty was defined using the model proposed by Robinson and colleagues that reflects the number of deficits an individual has accrued across different domains like gait speed and muscular strength, chronic anemia, comorbidity, cognitive impairments, ability to perform activity of daily living, malnutrition, geriatric syndrome of falls. Results show a high prevalence of frailty (19%) and pre-frailty (34%) in the studied population. Physical impairment (54%), comorbidity burden (29%), cognitive dysfunction (32%) and dependence in Activities of Daily Living (28%) largely characterized the frailty phenotype of our sample. Given its complexity and heterogeneity, a multidisciplinary and integrated care approach is necessary for designing a personalized plan of intervention. This will avoid wasting the benefits brought by the surgical intervention because of a poor supporting network.
Keywords
Elderly; Frailty; Surgery; Assessment
Introduction
During the last thirty years, the concept of frailty has growingly become object of interest in the scientific community and among public health authorities, largely because of the global aging. In particular, specific research and clinical actions have been developed in geriatric medicine to counteract the biological complexity hidden behind this condition [1]. Frailty is a dynamic state that affects an individual who experiences losses in one or more functional domains (physical, psychic, social), caused by the influence of multiple variables that increase the risk of adverse health outcomes. It is responsible for an increased vulnerability to endogenous and exogenous stressors and exposes the individual at higher risk of negative outcomes. It is an agedependent biological state secondary to the cumulative decline of multiple physiological systems. Frailty is related to multimorbidity, disability, risk of institutionalization, and mortality.
Diseases requiring a surgical approach, but even the surgical procedure per se, represent substantial stressors able to disrupt the individual’s homeostatic balance. The presence of frailty may thus be of special clinical relevance in older patients waiting for surgery [2]. It may, in fact, make the difference between a successful intervention and one characterized by poor outcomes and/or complicated by multiple adverse events. A clear/ definitive estimate of the frailty prevalence in this population is not yet available, with figures ranging between 4.1% and 50.3% [3]. Such variability is largely due to the different characteristics hosting the studies as well as the large heterogeneity of assessment tools used to measure frailty. Furthermore, eligibility criteria applied in the conduction of the different experiences might have biased the final results.
The aim of the present study is to measure the prevalence of frailty in a sample of “ real life ” older persons admitted to different surgery units in major university hospital. The sociodemographic and clinical features of the population are described. Demonstrating the prevalence of frailty within a surgical setting should increase sensitivity to the topic of integrated care.
Materials and Methods
Patients admitted to four surgical units (i.e., Units of Thoracic Surgery, Hepatobiliopancreatic Surgery, Vascular Surgery, Emergency and General Surgery) of the Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico (Milan, Italy) between October 2016 and December 2017 were included in the study. Inclusion criteria were: age ≥ 65 years; pre-surgery assessment in a dedicated short-stay hospitalization.
Frailty was assessed before the surgical intervention according to the model proposed by Robison et al. [4,5]: in this model frailty reflects the number of deficits an individual has accrued across a number of different domains like current illnesses, ability to manage activities of daily living (ADL) and physical signs. This model allows for the calculation of a ‘frailty index’ which can be thought of as ‘a count of an individual’s accumulated deficits’. The tool was chosen as particularly suitable for the settings of interest and minimally impacting on the daily clinical routine. The instrument is based on the measurement of the following criteria:
• Gait speed and muscular strength, assessed using the Timed Up-and-Go test. The test is conducted by asking the participant to stand up from a chair, walk 10 feet, return to the chair, and sit down. The performance is timed. A result equal to or higher than 15 seconds is indicative of poor physical performance.
• Activity of Daily Living (ADL), assessed by the Katz’ scale. The presence of one or more of the six predefined impairments indicates the condition of dependence.
• Cognitive function, assessed with the Mini-Cog test. It uses a paired 3-item recall task and the clock draw test. Abnormal cognition was defined when the Mini-Cog score was lower than or equal to 3.
• Comorbidity burden was measured using the Charlson’s Comorbidity Index, a marker of clinical complexity generated by the multiple conditions affecting the patient. An abnormal chronic disease burden was defined as a score higher than 3.
• Low hematocrit level, defined as lower than 35%.
• Malnutrition, defined by low or excessive body mass index (BMI; BMI<18.5 kg/m2 or BMI>25 kg/m2).
• History of falls, measured by asking the individual how many times he/she had fallen during the past six months.
Patients were grouped into three different groups according to their level of frailty [4,5]:
• Non-frail, in the absence of abnormalities or when only one criterion was present
• Pre-frail, if he had 2 or 3 abnormal characteristics
• Frail, when presenting 4 or more alterations
Statistical analysis
Descriptive statistics were used to present the sample features. Inferential statistics were applied to highlight relations between socio-demographical variables and frailty severity. Statistical analysis was performed using statistical software Stata 11.2 for Windows (StataCorp LP Statistics/Data Analysis StataCorp College Station, Texas 77845 USA).
Results
The study included 1,144 subjects with a mean age of 75 (standard deviation, SD 6.7) years. About 56% (n=645) of the sample was composed by men. In 80% (n=920) of the cases, patients had been referred via elective hospitalization. The type of interventions performed consisted of thoracic procedures (n=240; 21%), hepatic and pancreatic surgery (n=124; 11%), general surgery (n=312; 27%), emergency surgery (n=259; 23%), and vascular surgery (n=209; 18%). The average length of postoperative stay was 5 days (SD 7.0; Table 1).
| Variable name | N | F% |
|---|---|---|
| Age (years) (Mean (SD) and Median (IQR)) | 75.0 (6.7) | 74 (70-80) |
| Gender (male) (n and percentage frequencies) | 645 | 56.40% |
| Marital status (married) (n and percentage frequencies) | 821 | 71.80% |
| Emergency admission (n and percentage frequencies) | 224 | 19.60% |
| Surgical subspecialty (n and percentage frequencies) | ||
| Emergency abdominal Surgery | 259 | 22.60% |
| General Surgery | 312 | 27.30% |
| Vascular surgery | 209 | 18.30% |
| Hepatobiliopancreatic surgery | 124 | 10.80% |
| Thoracic surgery | 240 | 21.00% |
| Major surgery (n and percentage frequencies) | 353 | 30.90% |
| Length of stay (days) (Mean (SD) and Median (IQR)) | 5 (7) | 3 (5-7) |
| Frailty domains (impaired) (n and percentage frequencies) | ||
| Dependence in ADL | 313 | 28.00% |
| Bathing | 127 | 11.00% |
| Dressing | 128 | 11.00% |
| Toileting | 182 | 16.00% |
| Transferring | 210 | 18.00% |
| Continence | 164 | 14.00% |
| Feeding | 40 | 3.00% |
| Physical impairment (n and percentage frequencies) | 614 | 54.00% |
| (Mean (SD) and Median (IQR)) | 18” (7.5) | 15” (13-20) |
| Cognitive impairment | 371 | 32.00% |
| clock drawing test | 151 | 13.00% |
| 3-items recall test | 278 | 24.00% |
| History of falls | 117 | 10.00% |
| Chronic anemia (Ht) (n and percentage frequencies) | 161 | 14.00% |
| (Mean (SD) and Median (IQR)) | 38.5% (3.1) | 38.8% (36.2-40.6) |
| Malnutrition (BMI) (n and percentage frequencies) | 309 | 27.00% |
| (Mean (SD) and Median (IQR)) | 23.1 (2.6) | 23.4 (21.9- 24.7) |
| Comorbidity Burden | 332 | 29.00% |
Table 1: Main characteristics of the study sample (n=1,114).
The prevalence of frailty and pre-frailty in our sample were 19% (n=217) and 34% (n=395), respectively. The most prevalent criteria for frailty were physical impairment (54%), comorbidity burden (29%), cognitive dysfunction (32%) and dependence in ADL (28%; Table 1).
Statistically significant differences across levels of frailty were reported for age, type of admission, type of surgery, and surgical subspecialty. Overall, frail patients were more likely to be older (p=0.42; p<0.001), referred for an emergency admission (p=0.32; p<0.001), and undergo emergency abdominal surgical procedures. (R2 = 0.31, p<0.001). Frail patient were more likely to have a longer postoperative stay (p=0.58; p<0.001).
Discussion
Our findings show that frailty represents a highly prevalent issue among older persons undergoing surgical procedures. Roughly, one out of five older patients presents overt frailty and then half of our sample has at least two criteria negatively affecting his/her homeostatic balance.
Our data seem consistent with the prevalence documented by McCarthy and colleagues (i.e., 19.2%) in a similar sample of persons aged 65 years and older undergoing surgery [6]. Differently, the prevalence of frailty we reported in our study is slightly and consistently higher than that obtained in a representative sample of the community-dwelling Italian population [7].
Our study contributes to the growing body of literature in the field of frailty by providing an estimate of frailty retrieved from a large sample of older adults undergoing surgery. To date, the prevalence of frailty in surgical settings has been reported as ranging between 4.1 and 50.3% [3]. Such variability is likely due to the multiple instruments available for the measurement of frailty as well as the possible specificities of the studied populations. Sometimes such heterogeneity has been criticized because seen as affecting the standardized implementation of frailty in clinical and research settings. Not surprisingly, a large body of the literature has been looking for “the tool” able to unify the assessment and identification of frailty. Nevertheless, if frailty has to be considered as a condition to be screened for applying a multidisciplinary and integrated model of care, the choice of the instrument should rather rely on the resources and needs of the service and be function of the intervention(s) that will follow. In this context, the tool we adopted here is perhaps not the most commonly used, but it was found to be 1) Valid, and 2) Suitable for the setting were our clinical team is operating. Our prevalence data are in agreement with what emerges from the literature; therefore, considering the high prevalence of elderly subjects undergoing surgery, it would be necessary and desirable to plan integrated treatment paths with the collaboration of geriatricians and surgeons: these collaborations are already present for the context of orthopedic care, with orthogeriatric operative units that have contributed to the decline in mortality of elderly orthopedic patients in the postoperative period [8].
It is noteworthy that, consistently with the literature, frail participants were older, more likely to be admitted from the Emergency Department, and in the need of major surgical intervention. Consistently with previous reports [9,10], a high level of frailty was also associated to a longer postoperative hospital stay. These findings indirectly show the concept of frailty as the substratum for the patient’s clinical complexity. The consequent action to the identification of frailty should be a modification of the traditional care approach. An adapted and integrated care model should be privileged in order to avoid the many adverse outcomes caused by frailty (e.g., longer stay in the intensive care unit, cardiovascular and respiratory dysfunction). This shift of paradigm is in line with the characterization that frailty has been receiving as an emerging public health priority [11]. In this context, a study by Robinson et al. exemplifies how the number of frailty characteristics presented by the individual is associated with increased costs in surgical units. The true cost of an operation on an older adult to society does not stop at the time of hospital discharge. The amount of healthcare adds up to 30% after hospital discharge in the following 6 months.
Frailty assessment has the ability to define before surgery which patients will consume a disproportionate amount of healthcare resources and allows the potential to alter those patients’ care plans, which provide multidisciplinary management of the frail elderly patient [12].
Our study presents some limitations worth to be mentioned. It results from a monocentric experience, potentially limiting the application of the reported findings to a larger scale. Moreover, as mentioned, different results might have been obtained if other instruments were used for the assessment of frailty. However, assessing frailty preoperatively is a complete paradigm shift from traditional preoperative risk assessment, which focuses on single end-organ dysfunction [12] and it could encourage the possibility of creating similar treatment models to orthogeriatrics units.
Conclusion
Our study reports the prevalence of frailty in a large sample of older inpatients referred to surgical departments. Frailty appears to be particularly common in the older adults waiting for surgery. Future research should be focused on the post-operative management of the frail older patient and on methods for preventing the onset of frailty signs/symptoms at old age. It could also be useful the development of complex wards for postoperative care based on novel models promoting integrated and multidisciplinary care for frail people which provides for the systematic collection of biological and functional parameters that influence the outcomes: an increasingly closer collaboration between nurses, geriatricians and surgeons would improve the survival, outcomes and quality of life of the elderly in the postoperative period.
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
REFERENCES
- Ronchi S, Accardi R, Lusignani M. Elderly and surgery: Impact of frailty on surgical outcome. A literature review. Prof Inferm. 2019;72(2): 100-110.
- Kim SW, Han HS, Jung H, Kim KI, Hwang DW, Kang SB, et al. Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA Surg. 2014;149(7): 633-640.
- Partridge JSL, Harari D, Dhesi JK. Frailty in the older surgical patient: A review. Age Ageing. 2012;41(2): 142-147.
- Robinson TN, Wallace JI, Wu DS, Wiktor A, Pointer LF, Pfister SM, et al. Accumulated frailty characteristics predict postoperative discharge institutionalization in the geriatric patient. J Am Coll Surg. 2011;213(1): 42-44.
- Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC, Moss M. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg. 2013;206(4): 544-550.
- McCarthy K, Moug S, Stechman M, Hewitt J. 52 The Prevalence of Frailty in the acute general surgical setting. Age Ageing. 2014;43(suppl 2): ii16-ii16.
- Santos-Eggimann B, Cuenoud P, Spagnoli J, Junod J. Prevalence of frailty in middle-aged and older community-dwelling europeans living in 10 countries. J Gerontol A Biol Sci Med Sci. 2009;64(6): 675-681.
- Frondini C, Lunardelli ML. Ortogeriatria: Un nuovo modello di assistenza ai pazienti anziani con frattura di femore e comorbilità. Ital J Med. 2010;4(2): 105-110.
- Dasgupta M, Rolfson DB, Stolee P, Borrie MJ, Speechley M. Frailty is associated with postoperative complications in older adults with medical problems. Arch Gerontol Geriatr. 2009;48(1): 78-83.
- Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6): 901-908.
- Joseph B, Pandit V, Sadoun M, Zangbar B, Fain MJ, Friese RS, et al. Frailty in surgery: J Trauma Acute Care Surg. 2014;76(4): 1151-1156.
- Robinson TN, Wu DS, Stiegmann GV, Moss M. Frailty predicts increased hospital and six-month healthcare cost following colorectal surgery in older adults. Am J Surg. 2011;202(5): 511-514.
Citation: Accardi R, Ronchil S, Cesari M, Racaniello E, De Rosa E, Laquintana D (2019) Prevalence of Frailty Among Older Surgical Patients. J Aging Sci. 7: 217. Doi:10.35248/2329-8847.19.07.217
Copyright: © 2019 Accardi R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.