Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
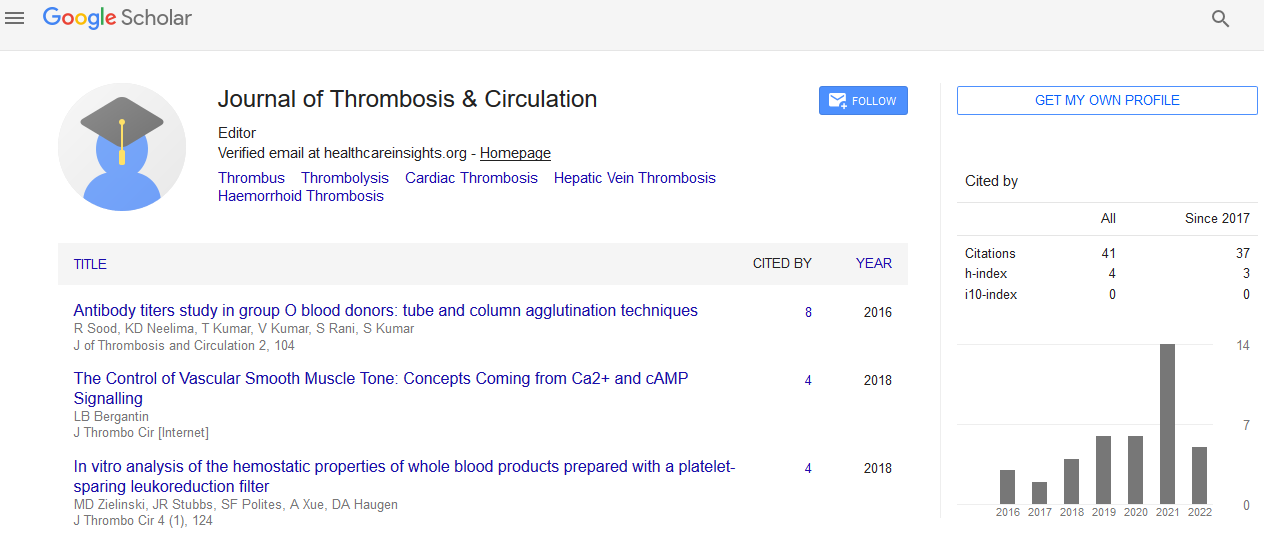
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Opinion - (2021) Volume 7, Issue 5
Prescient Variables of Venous Recanalization in Furthest Point Vein Apoplexy of Shallow Thrombophlebitis, Superficial Vein Thrombosis
Nitesh Singh*Received: 07-Sep-2021 Published: 28-Sep-2021, DOI: 10.35248/2572-9462.21.7.168
Abstract
Shallow thrombophlebitis or shallow vein apoplexy (SVT) results from clots development in a shallow vein with related irritation of the vessel divider. SVT is frequently seen in the lower limits with more noteworthy saphenous vein (GSV) inclusion in 60-80% of influenced people. SVT is 6-crease more normal than venous thromboembolism (VTE) with a yearly rate pace of 0.64%. Furthest point venous apoplexy (UEVT) addresses about 10% of venous thromboembolic illness. This is principally clarified by the expanding utilization of focal venous line, for oncologic or healthful consideration. The variables related with venous recanalization are not known.
Introduction
Furthest point venous apoplexy (UEVT) is an undeniably venous thromboembolic infection (VTED). Today, UEVT address 10% of all venous apoplexy, though it addressed 1 to 4% during the 2000s. This is predominantly clarified by the expanding utilization of incidentally embedded focal catheter - line (PICC-LINE) and of focal venous catheter (CVC). The major UEVT-related infections and conditions are: venous catheter, a strong neoplasia, a hematological threat, a thoracic outlet disorder (TOS), an estrogenic hormonal impregnation, inherited or gained organic thrombophilia (APLS), intense kidney disappointment or kidney disappointment requiring dialysis or different circumstances, for example, flares of provocative infections [1].
Diagnosis
The analysis of SVT is, by and large, made clinically, in view of the presence of trademark signs and manifestations including erythema, warmth and delicacy along a substantial string. Pressure ultrasound (CUS) can affirm the presence of SVT and portray the length of the blood clot and vicinity to the saphenofemoral intersection (SFJ), where the GSV joins the profound veins. Insights about these boundaries ought to be looked for from the radiologist when excluded from the ultrasound report. Execution of CUS ought to be considered in patients with clinically analyzed SVT, especially those with side effects over the knee or found near the popliteal fossa, in those with manifestations reminiscent of DVT and in patients with VTE hazard factors. Patients with underneath the knee SVT limited to a varicose vein without extra VTE hazard variables may not need CUS appraisal.
Treatment of Supraventricular Tachycardia (SVT)
General measures
As roughly 4% of patients with SVT will have an associative PE, all patients ought to be evaluated for a background marked by PE indications (e.g., dyspnea, pleuritic chest torment, hemoptysis) and examined appropriately. Patients with furthest point SVT related with vein cannulation or IV catheters ought to be surveyed for indications of disease (fever, purulent release at inclusion site) [2].
General measures
As roughly 4% of patients with SVT will have an associative PE, all patients ought to be evaluated for a background marked by PE indications (e.g., dyspnea, pleuritic chest torment, hemoptysis) and examined appropriately. Patients with furthest point SVT related with vein cannulation or IV catheters ought to be surveyed for indications of disease (fever, purulent release at inclusion site) [2].
Approach to treatment
When SVT is analyzed, treatment will rely upon whether an attendant DVT is distinguished and on the degree and most proximal area of the SVT. Anti-infection treatment is by and large not demonstrated except if there are indications of contamination. Patients in whom a corresponding DVT is recognized ought to be made do with remedial anticoagulation. Isolated SVT which reaches out to inside 3 cm of the SFJ is related with a high danger of movement into the profound venous framework. These patients ought to likewise get remedial dosages of anticoagulation for 90 days. Isolated SVT ≥5 cm long found >3 cm from the SFJ ought to get prophylactic portions of fondaparinux (2.5 mg subcutaneously each day), rivaroxaban 10 mg po every day or prophylactic/middle dosages of LMWH for 45 days. Patients can likewise get skin Nonsteroidal Anti-Inflammatory Drugs and additionally pressure Isolated SVT <5 cm long found >3 cm from the SFJ can be treated with oral or effective NSAIDs and packs (warm or cool) for indicative alleviation. In patients with confined SVT <5 cm long found >3 cm from the SFJ with extreme side effects or hazard factors for augmentation (earlier history of DVT/PE or SVT, malignant growth, pregnancy, hormonal treatment, late medical procedure or injury) therapy with prophylactic dosages of fondaparinux (2.5 mg subcutaneously each day), prophylactic portions of rivaroxaban (10 mg po day by day) or prophylactic/moderate portions of LMWH for as long as 45 days can be thought of. SVT related with IV cannulation isn't for the most part treated with anticoagulation. Steady measures, for example, warm packs and effective NSAIDs can be considered for indication help [3].
Special Populations
Pregnancy
No randomized investigations have evaluated the administration of SVT during pregnancy. Rule suggestions contrast and incorporate prophylactic or moderate portions of LMWH for a proper period (1 to about a month and a half) or all through pregnancy and the post pregnancy time frame in pregnant ladies with SVT that is reciprocal, indicative, ≤5 cm from the profound venous framework or ≥5 cm long. On the off chance that no treatment is controlled, clinical development and rehash CUS is prescribed inside 7 to 10 days. Warfarin and DOACs are contraindicated in pregnancy as these drugs can cross the placenta.
Pediatrics
Information with respect to the administration of SVT in this populace are exceptionally restricted. In the event that conceivable, pediatric hematologists with experience in thromboembolism ought to oversee kids with or in danger for SVT. At the point when this is preposterous, a blend of a neonatologist/pediatrician and a grown-up hematologist, upheld by meeting with an accomplished pediatric hematologist [3].
Conclusion
This is the main examination researching venous recanalization of UEVT in an enormous companion of 494 UEVT. This examination showed that clinical setting, the sort and geography of the apoplexy and the presence of focal catheter were related with recanalization after UEVT. The pace of recanalization without sequelae of UEVT was low (38%) with a middle opportunity to recanalization of 43 days. Lower arm shallow VT (cephalic and basilic veins); profound and distal UEVT, VT influencing just a single venous portion and non-occlusive UEVT were factors related with complete recanalization in this examination. These better paces of recanalization without sequelae could be clarified by the lower blood clot volume in these circumstances, permitting quicker and more productive clots lysis [4].
REFERENCES
- Chan WS, Nancy EK, Evelyne R, Thomas C, Michèle D, Paul SG, et al. Venous thromboembolism and antithrombotic therapy in pregnancy. J Obstet Gynecol Can. 2014;36:527-553
- Decousus H, Paolo P, Patrick M, Rupert MB, Zoltán B, Benjamin B, et al. Fondaparinux for the treatment of superficial-vein thrombosis in the legs. N Engl J Med. 2010;363:1222-32.
- Kommareddy A, Zaroukian MH, Hassouna HI. Upper extremity deep venous thrombosis. Semin Thromb Hemost. 2002; 28:89-99.
- Feinberg J, Nielsen EE, Jakobsen JC. Thrombolysis for acute upper extremity deep vein thrombosis. Cochrane Database Syst Rev. 2017 11;12:CD012175.
Citation: Singh N (2021) Prescient Variables of Venous Recanalization in Furthest Point Vein Apoplexy of Shallow Thrombophlebitis, Superficial Vein Thrombosis. J Thromb Circ. 7:168
Copyright: © 2021 Singh N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.