Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
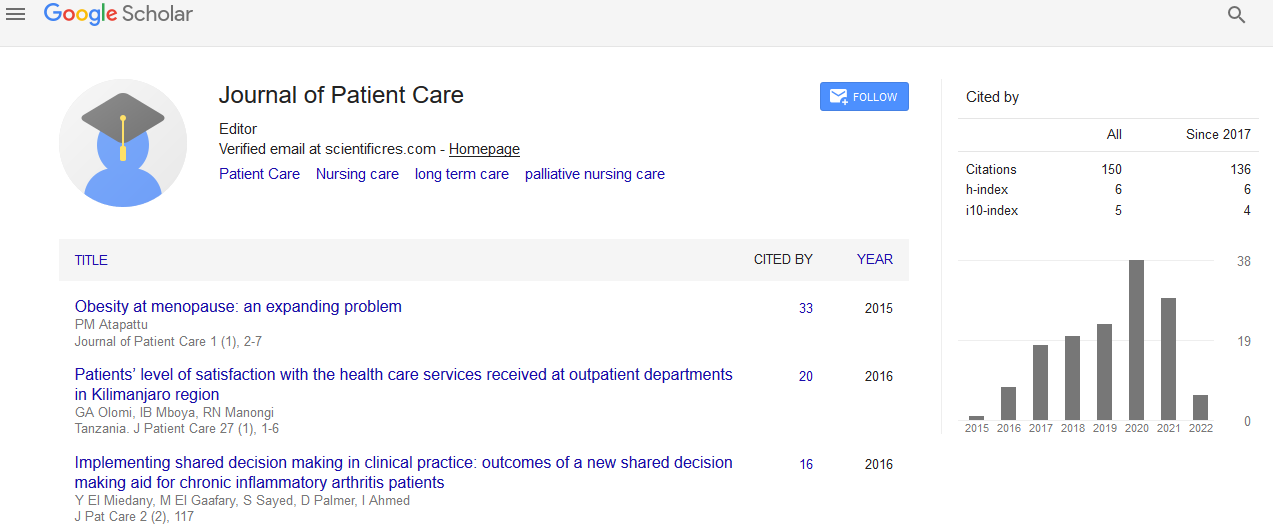
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2021) Volume 7, Issue 3
POTS Buddy Patient Advocate Working Directly on the Medical Team
Robert Wilson MD*Received: 10-May-2021 Published: 26-May-2021, DOI: 10.35248/2573-4598.21.7.160
Abstract
Patients often need medical seek medical guidance outside of their medical provider and direct medical appointment. Patients will utilize social media forums as one of aspect of care. Medical conditions such as Postural Orthostatic Tachycardia Syndrome (POTS) that may present with constitutional and misunderstood as behavioural lead to delayed diagnosis and patients developing further caution of health care systems We have developed a patient who an advocate is called the Pots Buddy. The Pots Buddy is educated and part of the medical team who provides a shared and validated experience for the patient that enhances medical care. We are offering in this commentary the role of a patient advocate concept being incorporated into the medical team as effective patient care model for adherence and challenges in health care systems in delivery of contemporary medicine.
Introduction
Postural Orthostatic Tachycardia Syndrome (POTS) is a disorder afflicting an estimated 500,000 Americans. POTS is diagnosed through tilt table testing with diagnosis confirmed in adults with a heart rate increase to ≥ 120 beats per minute (bpm) or an increase of >30 bpm within 10 minutes from baseline readings. Paediatric criteria are> 40 beats per minute. [1]. POTS patients may experience syncope, near syncope, chest pain, tachycardia, dizziness, and confusion. With the varying symptomology patients may present numerous specialists. More urgent symptoms may prompt ER care and hospital admissions. Arriving at a diagnosis is an exhausting journey for most patients, with long list of relatively common cardiovascular and neurological conditions usually ruled out before POTS is considered. In addition to the confusion and psychological distress that is endured, the chronicity of the illness predisposes patients to an impaired quality of life with limitations on activities of daily living [2,3]. If the medical system fails to arrive at a diagnosis of POTS, these patients are often referred to mental health clinicians only exacerbating the feelings of alienation, hopelessness, leading to a mistrust of health care systems. These patients often come to academic medical centres for the final answers of diagnosis.
Our Autonomic Centre at the Cleveland Clinic has embraced this dismal reality for POTS patients and has formulated access and unique care for this demographic with an expansion of inter professional medical team of physicians, APPs, nurses, and psychologists. The addition of email portals and virtual appointments increased access and the needs of addressing care coordination from a distance, social media questions to be addressed, and limits of in person appointments. The development of Shared Medical Appointments once in person and now with COVID-19 via zoom, patients come together in a group where a physician leads with education, disease management skills, and even specific care points individualized to one’s health needs.
Despite the developments and commitment for access and understanding the journey these patients have been though pre diagnosis and being incorporated into our care there was still a void or missing aspect to the patients’ psychological needs and questions. Even with the increased access and educational opportunities the historic path of the patients through health care systems pre diagnosis and over reliance of social media that does not give an absolute tangible of authenticity if does apply to oneself did not completely help many of the patients with move forward in questions and next steps of care.
The Shared Medical Appointments are invaluable as patients connect and hear similar stories and challenges from their peers. The sharing of resources and problem solving have proved for a grounding experience that help move patients forward to make choices in smart and effective choices of care, eliminating an over reliance on social media. This awareness led to the development of the POTS Patient Liaison Program, also referred to as the “buddy” program.
This initiative aims to address the lack of connectivity and understanding, experienced by POTS sufferers. Family and significant social supports may lack medical literacy, true support, and have high stakes. To reduce the nervous approach of healthcare access, the buddy has been trained by the medical team on disease state and helps the patient define an achievable goal to ward wellness. The buddy will join appointments in clinic, via zoom and the shared medical appointments. The buddy has no access to medical records, but has POTS herself. The uniqueness is the foundation that someone with a shared diagnosis knowledge of the challenges of health care systems who helps the patient works toward achievable goals within the diagnosis. The patients engaged in this program have found validation, clarity, effectiveness, and are resolved.
As humans, we are often moved by stories that are similar and of which we can identify. By giving this reliability of the human experience and teaming up for goals out of the norm of traditional medicine our experience is these patients do better. Those involved are following through with more care, less need of social media, and a reduction in messaging needs.
Similar programs have been used for patients with HIV, autism, alcohol dependency, and those receiving organ transplants, but not to the extent or with the organization of the POTS Liaison program. This model of healthcare shows promise for patient populations who are suffering from similar chronic conditions in alleviating strain on the current medical system and offering a higher standard of care and vastly improved quality of life. Also growing numbers of POTS from post COVID-19 will show more relevance of this additional care support [4].
REFERENCES
- Robertson D. The epidemic of orthostatic tachycardia and orthostatic intolerance. Am J Med Sci. 1999; 317 ;( 2):75-77.
- Benrud-Larson LM , Sandroni JA, Haythornthwaite TA, Rummans PA. Low. Correlates of functional disability in patients with postural tachycardia syndrome: preliminary cross-sectional findings. Health Psychol, 2003;22 :643-648
- Benrud-Larson LM, Dewar MS, Sandroni P, Rummans TA, Haythornthwaite JA. Low. Quality of life in patients with postural tachycardia syndrome. Mayo Clin. Proc. 2002; 77: 531-537
- Goldstein D, Hear Rhythm, December 2019;(12):007
Citation: Wilson R, Silberfeld N (2021) POTS Buddy Patient Advocate Working Directly on the Medical Team. J Pat Care 7:160.
Copyright: © 2021 Wilson R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.