PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
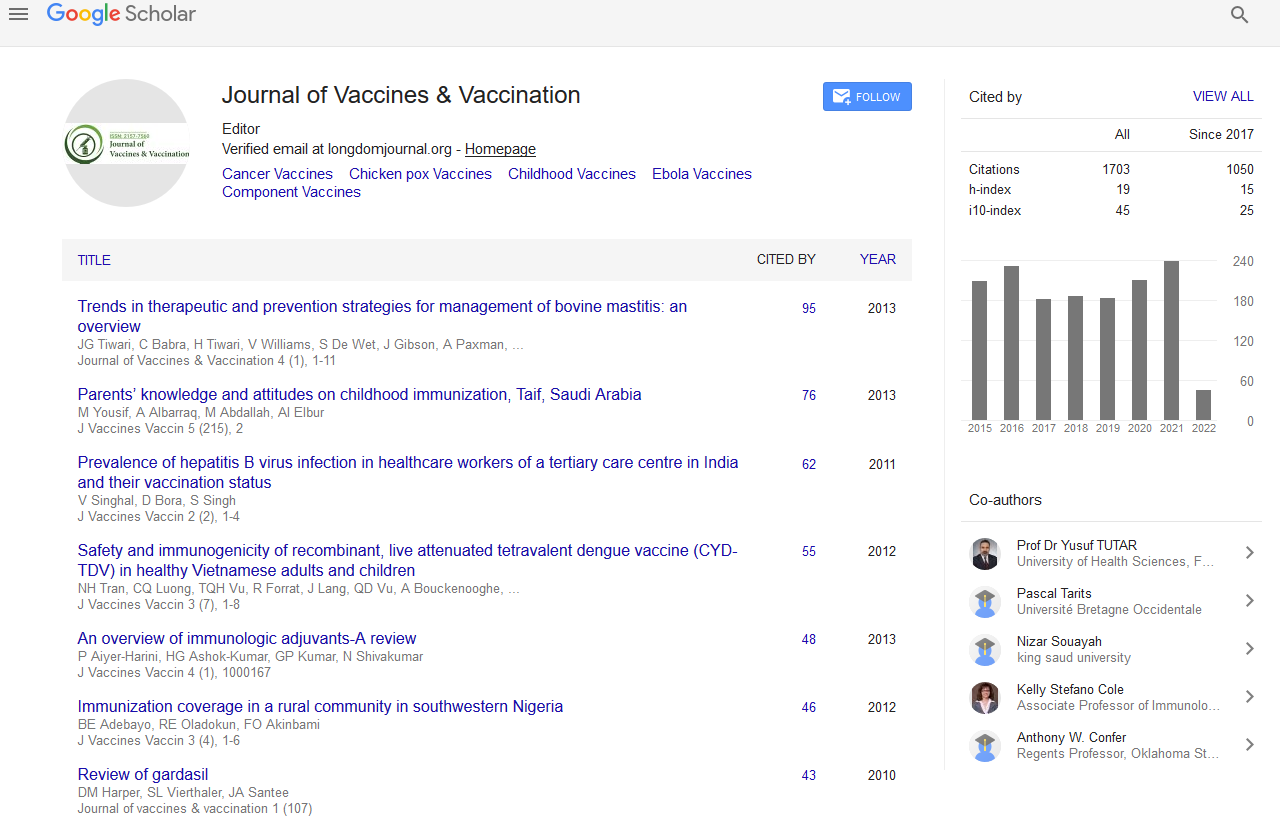
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2020) Volume 0, Issue 0
Personalizing Vaccination for Infectious Disease in the 21st Century
Reginald M Gorczynski*Received: 16-Oct-2020 Published: 05-Nov-2020, DOI: 10.35248/2157-7560.20.S5:005
Abstract
Current approaches to vaccination have several underlying assumptions, namely that following immunization most individuals are at similar risk of the disease considered; will react immunologically in the same way (with protective antibodies and/or cell-mediated reactivity) with equivalent and minimal side effects; and that vaccination dosing and frequency of administration does not vary in the population at large. As a result, a widespread delivery of vaccines has been achieved for a number of infectious diseases, with effective control for many of those. It is clear that a weakness of this approach, made manifest with our increasing knowledge of the genomic and proteomic approach to medicine which has come to the fore in the last decade or so, is that it discounts the growing evidence for individual variability in risk; in immune responsiveness; and in response to different doses of vaccine. While this evidence grew from a focus on tailoring individual approaches to cancer therapy, and has revolutionized our thoughts on drug therapy, drug pharmacogenomics and toxicity and the importance of understanding at the individual, not population level, unique responses to treatment, application of the same approach to vaccines for infectious disease has not had a similar attention. Indeed, not only does consideration of individual specific factors challenge a traditional public-health level paradigm of infectious disease vaccinology, and confront newer approaches based on genetically encoded individuality in response to pathogen challenge, but the cost-benefit of such an approach has, to the author’s knowledge, not been considered at all. The review below will consider these issues in greater detail, with a final focus on how this might dictate our global responses to emerging infections.
Keywords
Personalized medicine; Vaccine development; Immunology of host resistance; Innate immunity; acquired immunity; COVID19
Introduction
It goes without saying that the development of the field of personalized medicine was fostered by the completion of the Human Genome Project and the international HapMap, with further advances then dependent upon new molecular assay tools allowing for high-throughput detection of gene variations, particularly Single Nucleotide Polymorphism (SNP) and linkage disequilibrium maps. This applies even to high-throughput tools needed for the genotyping of SNPs known to be related to drug and xenobiotic metabolism [1-3].
Application of standardized therapies in a number of cancers has shown great individual-to-individual variation in response to treatment. With the advent of immunotherapies, that variability became even more pronounced, reflecting presumably polymorphisms in key immune response genes which in turn lead to heterogeneity in immune responses to biologic manipulation, as well as genetic variability in the expression of target molecules on individual tumors to which immunotherapy was directed [4- 8]. Fundamental advances in knowledge of the mechanism(s) responsible for tumor cure were essential before any rationale could be applied in this field [9-13]. More recently however there has been attention paid to other demographics in the population, particularly age and age-associated immune changes (e.g. in natural killer cells; naïve T cells), in altering individual responses to cancer therapy [14]. A more challenging variable, in terms of understanding and incorporation into therapeutic predictions, is the growing evidence that the gut microbiome can also influence overall immunity and may affect immunotherapy of cancer [15].
This notion that a new focus on personalized medicine might represent a paradigm shift in many chronic diseases led to rapid “spill-over” into other fields, including as an example, allergy and autoimmune diseases [16,17]. Systemic Lupus Erythematosus (SLE), a disease with wide ranging clinical symptoms, has an equally heterogeneous biological diversity, and newer investigations on peripheral blood immunophenotyping using flow cytometry and mass cytometry to identify cell subsets and markers associated with that disease heterogeneity, along with transcriptome analysis to highlight molecular networks responsible for disease activity and disease subtype/response to therapy, are contributing to newer approaches [17,18]. Understanding the correlation between risk alleles and the nature of both underlying immune abnormalities and varied drug responses (pharmacogenomics) across populations, as already noted in the approach to cancer therapy, is key to any rationale intervention in autoimmunity and inflammatory disease. [19-21].
Understanding the Variables Contributing to Altered Vaccination in Infectious Disease
It has long been acknowledged that polymorphisms in a number of immune response genes results in heterogeneity in immune responses to many biologics including vaccines [22]. However, given the success of a traditional public-health level paradigm of infectious disease vaccinology, resulting in the successful eradication of a number of scourges, including smallpox, and good control of many childhood diseases (measles/mumps/rubella/varicella/polio) with a high cost-benefit ration across global societies, little attention has been paid to the potential value of a more individual specific approach to vaccination against infection. This despite broad evidence that there are important genetic differences (e.g. humans HLA Class II controlling human antibody responses) contributing to different responses to Hepatitis B virus (HBV) and measles virus vaccines [23-25] leading potentially to the documented increased susceptibility to HBV [26,27]. Genetic differences also contribute to sex-related difference in response to vaccines, with women in general mounting an increased antibody response over men [28]; and to more subtle racial/ethnic differences such as the Km/Gm antibody carried by Native Alaskans and Native Americans which had been previously controversially thought to be associated with impaired immune response to polysaccharide vaccine antigens [29, 30]. Indeed, even polymorphisms in response to a common drug which alters transcription of immune response genes has been associated with altered response to (cancer) vaccines [31]. The risk of adverse events following a standard vaccination regime has also been linked with genetic predisposition e.g., vaccinia associated pericarditis, occurring an estimated 1:14,00 individuals, following vaccination vs smallpox [32,33], including the risk of febrile seizures following vaccination with MMR vaccine [34,35].
It should be noted that not only HLA-related polymorphisms, which are likely related to recognition of antigenic epitopes on the infection pathogen, but cytokine gene polymorphisms associated with further development of immune responses have proven relevant in infectious immunity [25,36,37]. Gender differences in response to measles and rubella vaccination have also been reported [38,39]. See also [40] for a review of sex related difference in immunity) Moreover, given that we now know that immune responses change both qualitatively and quantitatively with age, with a marked shrinkage in the immune response (T cell) repertoire in elderly individuals [41], along with an expansion of “exhausted T cells with high PD-1 expression [42], it should be no surprise to find that there are wide variations in response to vaccination with age.
Original antigenic sin (OAS), a term first used by Francis in 1960 [43] refers to the phenomenon that the shape of ongoing immune responses to a persistent/recurrent pathogen (in the case studied, influenza) was “molded” by the initial response made. Thus, the majority of influenza virus antibodies in a population showed cross-reactivity to the original (pioneer) strain for that group [44]. Neonatal immune responses are in general more limited in heterogeneity than the adult counterpart, which may in part explain the poor response to vaccination in the former, when using recombinant antigen (not inactivated viral) vaccines, as compared with immunity generated by live virus infection which presumably offers a broader epitope range for immune challenge. The issue of contraction of the repertoire in the elderly in turn then helps explain their generally poorer response to vaccination by contemporary vaccines. Imprinting, the phenomenon whereby first exposure to pathogen shapes all subsequent exposures [45,46], and interference (which explains how antibody to an original strain of pathogen can interfere with antibody responses to subsequently encountered (different) strains [47]) further compounds these age related altered immune responses to pathogens. The contribution to all of these factors in understanding the contemporary approach to influenza vaccination is discussed below. Consideration will then be given as to how this might guide thoughts to developing useful strategies to novel infections and/or pandemics.
Influenza as a Model for Population Based Infectious Disease Control
Influenza is a major health problem, with in the order of 3 to 5 million cases of severe illness and 290,000 to 650,000 respiratory deaths per year world-wide [48]. Young children (<24months), pregnant women, immunocompromised subjects, individuals with co-morbidities regardless of age, and the elderly all have a higher risk for influenza-related co-morbidities, many of which will lead to death. In healthy children younger than 24 months of age, the risk of hospitalization is comparable to that of high-risk groups, or even higher. Vaccination is the mainstay of protection against disease. A major challenges to an effective vaccination program follows from the understanding that influenza viruses are constantly changing, leading to antigenic drift that results in escape from earlier immune responses. Thus, monitoring vaccine efficacy is a key issue in the strategy for mass vaccination. As a correlate marker of vaccine efficacy an immune function which can be shown to be responsible for protection, and is easily measured, is used for monitoring (e.g. influenza serum hemagglutination antibody titres, HI), and stringent criteria must be met for licensure of a vaccine. In terms of population responses, a pre-determined increase in titre: e.g. >40 in 18-60 year olds with a 4-fold increase in titre post vaccination and >40% seroconversion in the same group has historically been associated with ~50% reduction in influenza risk [49]. However, it is recognized that in the elderly, where standard vaccine therapy is ineffective [50], strict analysis of HI titres may not be as useful in guidance of vaccination, and monitoring of cell mediated immune responses may be more valid predictors of efficacy [51-55]. This is an important issue, since we know that antibody and cell mediated responses are generally directed to different antigenic epitopes. Thus, in the absence of use of live vaccine, or a live attenuated virus vaccine [56] our choice of recombinant material to include in any vaccine on offer must encompass the antigenic determinants likely to provoke the relevant immune response in the population at risk. Current developments in the influenza vaccine field have addressed these issues and use novel methodology to determine responses other than HI tires which are more applicable in other populations [57-60].
Another correlate of the move away from use of live attenuated or whole cell vaccines, which already contain inbuilt adjuvants promoting auxiliary immune stimulation (ex. bacterial cell wall components; other genetic material including polynucleotides) to the use of purer (recombinant) antigens for safer vaccines, is that there has been an attendant development in the field of novel adjuvants which are now necessarily added to improve efficacy of these newer recombinant vaccines [61,62]. Safety testing of such adjuvants is also needed, and careful choice, given evidence that different adjuvants may promote antibody vs cellular immunity [61,62].
Concerns about an Individual Approach to Vaccination
Despite the evidence that improved vaccine efficacy might arise from personalization of the vaccination strategy used, there are considerable practical issues which make this a very difficult task. Screening for individual factors which contribute to vaccination differently across subgroups will likely add substantial costs to vaccination, although potentially saving other costs (e.g. hospitalization of elderly and other high-risk groups). As already noted, use of personalized vaccines depends on prior knowledge/ characterization of genetic influences on immune response, a field still developing and for which no current routine population testing is offered. Pre-vaccine screening for immune status has been considered, but with the exception of the unvaccinated adult with respect to varicella vaccination, where serologic testing in an adult with a negative history of chicken pox is cheaper than vaccination, vaccination is cheaper than testing.
Most vaccines currently used for infectious disease have high immune response rates, and there is concern over the overall cost of achieving small further advances in vaccination uptake following population genetic screening in order to improve the immune response to vaccine for a minority of the population. Careful consideration of the overall costs to health care should a highly susceptible population contract the disease under consideration clearly will play a major role in this determination. In a similar light, screening for an increased propensity to adverse events in subgroups of individuals may foster a drive for general genetic screening.
There is also the practical difficulty of licensure of personalized vaccines. This is less an issue for treating patients with cancer, where development of individualized cancer vaccines lacks the attendant problems facing manufacturers trying to license materials for mass production and distribution. As of now, regulatory bodies require prelicensure testing in animals and humans for all vaccines and for each dose and schedule. It is against such a background that there is a growing interest in the development of a “one-size-fitsall adjuvanted peptide vaccine cocktail”, which may prove the way forward for e.g. influenza vaccines, in the not-too-distant future. In such a model, different individuals will respond to different agents contained in the cocktail, which are pre-selected and included based on population-level HLA supertype frequencies and age distribution [63].
Personalized Medicine and Response to Novel Infectious Agents, Including COVID-19
In this final section we will consider the value of the information outlined above in determining global responses to new infectious agents, with a particular focus on COVID19. At the time of writing (September, 2020) the world is immersed in focus on a pandemic associated with COVID19 infection. However, even though this is a novel coronavirus infection, our knowledge of past pathogens should be a useful guide to how we approach the problem of developing and using a vaccine. Much of the modeling and thought behind the response to COVID19 has used as background data on recent coronavirus infections (SARS, MERS, [64,65]) and even the global response to the 1918 Flu Pandemic.
Spanish flu, also known as the 1918 flu pandemic, was a particularly deadly influenza pandemic caused by the H1N1 influenza A virus [66]. A second pandemic caused by H1NI was the so-called swine flu pandemic of 2009 [67]. The former lasted about 15 months from spring 1918 (northern hemisphere) to early summer 1919, infected approximately one-third of the world’s population at the time (~500 million people), and had a death toll estimated to have been anywhere from 17 million to 50 million, and possibly as high as 100 million, making it one of the deadliest pandemics in human history [68,69].
While most influenza outbreaks produce their highest mortality in the very young and the very old, with a higher survival rate for those in between, the 1918 pandemic resulted in a higher than expected mortality rate for young adults. Scientists offer several possible explanations for the high mortality rate of the 1918 influenza pandemic. It has been suggested that the virus was particularly deadly because it triggered a cytokine storm, leading to severe pneumonia (much like thoughts regarding COVID19-see below) [70,71]. Alternative, or additional socioeconomic features including those associated with malnourishment, overcrowded medical camps and hospitals, and poor hygiene, all exacerbated by the recent war, which likely contributed to bacterial superinfection were also likely important in 1918 [68,71,72].
As mentioned repeatedly, without understanding the physiology, immunobiology and genetics of the host response to any infection (in this case COVID19), health experts are floundering in the dark. In the early phases on the COVID19 pandemic, effort was focused on PCR testing to assess for evidence of viral infection in symptomatic individuals to obtain some gauge of the prevalence of infection-neglecting the concern that knowledge of infected but non symptomatic individuals may contribute significantly to understanding the disease. Furthermore, the absence, in the early stages, of any serology data recording the numbers infected who developed a measurable immune response, and how that correlated with disease progression, also hindered understanding. An early report from Germany put this, in one locale, at a minimum of ~14%, but again with no corollary data on symptoms [73]. Global media reports cited mortality statistics projections from 1% to upwards of 14%, but without any widespread population data, these numbers were simply nonsensical. As a comparator (see data above regarding influenza virus statistics) the SARS corona virus infection, which struck in 2003 had a global fatality rate of 9.6 per cent (12.4 per cent in Canada) [74], but with a relatively restricted number of infected individuals (predominantly person-to-person spread).
Of major concern in COVID19 is the controversy regarding our understanding of the mechanisms of initiation and spread of the disease. Current dogmatic thinking suggests person-toperson spread, including by aerosols, though there are numerous contradictory data which refute this but are ignored. Not surprisingly then there has been confusion and controversy over the value of using face masks as a method of preventing disease spread, though a recent report in the New England Journal of Medicine indicates it may at least be efficacious in alleviating anxiety [75]. There can be little doubt that fomite spread is an important issue, so advice re hand washing and practice of good hygiene is paramount [76]. A much more radical alternate hypothesis, based on the available epidemiology, the developing spread of infection across Europe, and sequence data from viral isolates, suggests that the inciting event may have originated in a cloud of dust of cosmic origin containing a pure culture of the virus arriving in large quantity first over China, and then dispersed through stratospheric transport processes to be deposited on a global scale following prevailing atmospheric drift [77-81]. This “fall-out” of viruses associated with the current COVID-19 crisis is seen as representing a small perturbation of the billions of viruses per square metre per day that fall through the atmosphere, some of which can be recycled from Earth sources [82], but many of which were predicted and discussed in the past by Hoyle and Wickramasinghe [83].
In an interesting recent submission Qu and Wickramasinghe discussed the advantages of scientific “preparedness” to detect the influence of cosmic ray flux, space weather, and the possible introduction of novel bacteria and viruses from the stratosphere [84]. Such organisms have already been detected at heights up to 42Km [85,86], and indeed on the exterior of the ISS orbiting the earth at over 400Km [87]. Independent measures of the downward flux of viruses in the Sierra Nevada mountains have ranged from 0.25x109 to greater than 7x1010m-2/day [88], numbers which are not easily explained as having originated on the ground [89].
As might be anticipated, there has been intense resistance to this view of the new pandemic (particularly as it argues against the weak evidence for person-to-person transmission as a major focus of the initiation of infection) associated with a long standing scientific resistance to accept hypotheses concerning our possible cosmic ancestry and origins (panspermia) which is discussed elsewhere [78, 81,82]. See also [90] for more discussion on the role of solar activity and incidence of viral pathogenesis). Nevertheless, almost all socalled experts have supported governments in the imposition of quite draconian measures restricting people’s lives and movements unheard of in peacetime, across almost all countries (with perhaps the notable exception of Sweden). The attendant short- and, more importantly, long-term costs to the mental, social and economic well-being, as well as the overall health, of those populations has not been well thought through [91]. It has also been argued that attention to this alternative hypothesis (infection as an “infall event” from the stratosphere) allows for testable scientific predictions, most important of which for future potential emerging infections is that it suggests a pro-active rather than a reactive approach to vaccination strategy. If we accept that newly arriving (on earth) infectious material is already accessible in the stratosphere, then sampling this material should provide advance warning (by 1-2 years) of new “emerging” pathogens on earth, providing substantial lead-time to investigate responses to infection in mammals and development of containment/vaccination procedures.
Such lead time may well be crucial. As is evident from over 40 years of research on influenza vaccination, we are still a long way off providing optimal vaccination regimes for the most vulnerable members of our communities (the young; elderly; and those with multiple co-morbidities). We have little knowledge concerning the biology and host resistance factors of many of our more newly documented infectious agents (Zika virus [92]; Candida auris species [93-95]; COVID19 [96]). A preliminary report in ~108 volunteers (ages 18-60) of immunity in humans following administration of 3 different doses of an Ad5 vectored COVID-19 (97) documented production of both T and B cell immunity (peaking by ~14/28d post vaccination respectively) with minimal adverse effects. To date, the correlation of either (or both) of T/B cell immunity with protection following vaccination against COVID-19 remains unknown, and the authors in the study acknowledged that they were unable to predict the protection of the Ad5 vectored COVID-19 vaccine on the basis of the vaccine-elicited immune responses in this study. There are, however, guiding principles available from previous studies of other coronavirus infections in man, investigating SARS and Middle East respiratory syndrome (MERS) respectively. Here the increases in specific antibodies were temporary [98,99], and declined quickly in patients after recovery, whereas it seems that both specific CD4+ and CD8+ T-cell responses played an equally if not more important role in mouse models of immunity [100,101]. A similar rapid decline of the specific antibody amounts in patients with COVID-19 after recovery has also been recorded [102,103], again consistent with the notion that both specific cellular and humoral immunity may be crucial for a successful COVID-19 vaccine. Note that little data is available even in preliminary form for vaccination of patients in particularly vulnerable groups (elderly; those with other co-morbidities [104]), as is any detailed assessment of the usefulness of different adjuvants in enhancement either/both T cell and B cell immunity [105] or even whether unique T and/or B cell recombinant epitopes might prove a safe but effective route of vaccination for protection [106,107]. It is also pertinent to note that given the fact that COVID-19 (and SARSCoV/ MERS-CoV) targets primarily the respiratory tract, designing a vaccine which induces immunity after intranasal delivery might be an optimal strategy for vaccine development.
As regards development of a more specific COVID-19 vaccine, following engagement of the acquired immune response (B and T cell immunity) over the next 12-18 months, one might ask what would the platform for vaccine development look like? RNA vaccines are rapidly produced, but to date none has been licensed for any viral infection. Splicing a relevant gene into an accepted viral vector is an alternative and has been used for a licensed EBOLA vaccine [108]. More likely the licensed product will use a recombinant protein of COVID19, in association with a suitable adjuvant, as this protocol has the best promise of rapid delivery of a licensed vaccine at the volume needed for the global community [109,110]. As discussed above with reference to influenza vaccines, care must be taken to optimize safety and ensure the reagents used do not cause antibody mediated disease enhancement [111- 113]. Merging multiple streams of new data and information are improving the rapidity of development of a COVID 19 vaccine [114,115], but at the time of writing the prevailing thought is that any vaccine for COVID19 is still several months away, with risk assessment of vaccines still pending.
In this interim period, is there any approach that can be used (besides drug therapy) to temporize while we await production of a suitable vaccine? It is known that the immune response in mammals is comprised of both an innate and adaptive arm. The latter (T and B lymphocytes) are responsible for immunologic memory but take some 10-14 days post pathogen exposure to become active. In contrast, protection mediated by the innate immune system, which is the sole immune mechanism for 95% of the species on earth, develops quickly (1-2days), although it has been argued it does not display immune memory. The latter issue has now been challenged by data which has shown quite clearly that “training” does occur in responses, which results in an enhanced protection from reinfection (with the same pathogen) and even enhanced immunity to novel (in this case, non-tubercular) pathogens [116]. The mechanism(s) involved are thought to involve epigenetic changes (altered DNA methylation; Histone deacetylase activity) which results in more rapid gene activation of genes implicated in pathogen responses, as well as an altered cell metabolism. As an example, monocytes obtained from individuals vaccinated with BCG vaccine have been shown to exhibit enhanced cytokines responses (IL-1β IL-6; TNFα production) on exposure to other (yellow fever) viral pathogens [117]. This same phenomenon may in part at least be responsible for the observations made some time ago that infant mortality, and even adult mortality, is less in BCG vaccinated cohorts than in non-vaccinated cohorts from the same population [118]. Since the effects of BCG in human experimental subjects have been seen at long times (>12 months), beyond the time expected for an effect mediated by epigenetic changes on mature monocytes, it has been thought that re-programming of myeloid development from bone marrow precursors must also occur, as documented now by Kaufman et al [119]. The implications then of using such BCG-mediated training of innate immunity in vaccine development has in turn been discussed elsewhere by Covian [120], and provides the underlying principle behind the ACTIVATE trial in elderly volunteers to assess the contribution of BCG vaccine in decreasing susceptibility to bacterial disease [121]. More recently a BCG-CORONA trial [122] has also been initiated to assess the value of BCG vaccination in reducing health care worker’s infection and disease severity during the epidemic phase of SARS-CoV- 2 (COVID -19) see also [123]).
It has also been suggested that ongoing development of human monoclonal anti-COVID19 antibodies be developed also as treatment regimens, given their now known proven efficacy in HIV infection [124,125]. This has been reviewed elsewhere by Sharun [126,127].
Conclusion
It should be apparent that there are good parallels, drawn primarily from the emerging field of personalized care in cancer therapy, to argue that such an approach will have a major impact in the future treatment of infectious disease. The arguments raised above show that this cannot take place in a vacuum, however, and depend heavily upon improved knowledge of the epidemiology and natural resistance mechanisms in any infectious disease outbreak. Using the contemporary global response to COVID19 infection, it is clear that attention to such variables have not characterized what has often been a response dictated more by political expediency, and scientific dogma, than by a rationale attention to the emerging facts. Indeed, a recent summary of data in exposed but asymptomatic individuals concluded that “SARS-CoV-2-specific memory T cells were detected in exposed seronegative healthy individuals (relatives of confirmed cases), indicative of asymptomatic infection. Remarkably, "93% of ‘exposed asymptomatic individuals mounted detectable T cell responses to SARS-CoV-2 despite only 60% of cases being seropositive. This suggests that asymptomatic infections may be more common than current data suggest and that immunosurveillance through antibody testing alone may underestimate infection prevalence or population immunity. The presence of SARS-CoV-2-specific T cells in the majority of convalescent patients is a promising sign that infection may give rise to immunity, but whether these T cells afford protection from reinfection remains to be tested”.
While the hope exists that an effective vaccine (for some) may emerge from current studies with the candidate vaccines now under consideration, it is clear that more attention to the role of a bolstered innate immune response, and the value of adjuvants as triggers of the latter, along with careful analysis of the role of the nature (and degree) of any acquired resistance mechanisms which may be effective, will be paramount to success across populations, and particularly for those at greatest risk. It is wise to remember indeed that the universal argument made in favor of mass quarantine in the early stages in virtually all affected countries was this notion that we must protect the vulnerable (elderly) and those with co-morbidities who were at greatest risk. Vaccination strategies must do likewise.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
REFERENCES
- Agapito G, Settino M, Scionti F, Altomare E, Guzzi PH, Tassone P, et al. DMETTM Genotyping: Tools for Biomarkers Discovery in the Era of Precision Medicine. High-throughput. 2020; 9(2):8.
- Beger RD, Schmidt MA, Kaddurah-Daouk R. Current Concepts in Pharmacometabolomics, Biomarker Discovery, and Precision Medicine. Metabolites. 2020; 10(4):129.
- Ho D, Quake SR, McCabe ER, Chng WJ, Chow EK, Ding X, et al. Enabling Technologies for Personalized and Precision Medicine. Trends Biotechnol. 2020; 38(5):497-518.
- Ren D, Hua Y, Yu B, Ye X, He Z, Li C, et al. Predictive biomarkers and mechanisms underlying resistance to PD1/PD-L1 blockade cancer immunotherapy. Mol Cancer. 2020; 19(1):1-9.
- Azim HA, Ghosn M, Oualla K, Kassem L. Personalized treatment in metastatic triple-negative breast cancer: The outlook in 2020. Breast J. 2020; 26(1):69-80.
- Wong EM, Southey MC, Terry MB. Integrating DNA methylation measures to improve clinical risk assessment: are we there yet? The case of BRCA1 methylation marks to improve clinical risk assessment of breast cancer. Br J Cancer. 2020; 18:1-8.
- Jiang Y, Zhao X, Fu J, Wang H. Progress and challenges in precise treatment of tumors with PD-1/PD-L1 blockade. Front Immunol. 2020;11.
- Koulis C, Yap R, Engel R, Jardé T, Wilkins S, Solon G, Shapiro JD, et al. Personalized Medicine—Current and Emerging Predictive and Prognostic Biomarkers in Colorectal Cancer. Cancers. 2020; 12(4):812.
- Aversa I, Malanga D, Fiume G, Palmieri C. Molecular T-Cell Repertoire Analysis as Source of Prognostic and Predictive Biomarkers for Checkpoint Blockade Immunotherapy. Int J Mol Sci. 2020; 21(7):2378.
- PRETE CD, Azzoli CG. Non-Small Cell Lung Cancer in the Era of Personalized Medicine: Molecular Tests that Matter. R I Med J. 2020; 103(3).
- Said R, Guibert N, Oxnard GR, Tsimberidou AM. Circulating tumor DNA analysis in the era of precision oncology. Oncotarget. 2020; 11(2):188.
- Zhao D. Single Nucleotide Alterations in MicroRNAs and Human Cancer-A Not Fully Explored Field. Noncoding RNA Res. 2020.
- Ma M, Liu J, Jin S, Wang L. Development of tumour peptide vaccines: From universalization to personalization. Scand J Immunol. 2020; 91(6):e12875.
- Kasanen H, Hernberg M, Mäkelä S, Brück O, Juteau S, Kohtamäki L, et al. Age-associated changes in the immune system may influence the response to anti-PD1 therapy in metastatic melanoma patients. Cancer Immunol Immunother. 2020; 8:1-4.
- Khan MA, Ologun G, Arora R, McQuade JL, Wargo JA. Gut Microbiome Modulates Response to Cancer Immunotherapy. Dig Dis Sci. 2020; 64:885-896.
- Crisci CD, Ardusso LR. A Precision Medicine Approach to Rhinitis Evaluation and Management. Curr Treat Options Allergy. 2020; 7(1) 93-109.
- Renaudineau Y. Immunophenotyping as a new tool for classification and monitoring of systemic autoimmune diseases. Clin Rev Allergy Immunol. 2017; 53(2):177-80.
- Nagafuchi Y, Shoda H, Fujio K. Immune profiling and precision medicine in systemic lupus erythematosus. Cells. 2019; 8(2):140.
- Carini C, Hunter E; Scottish Early Rheumatoid Arthritis Inception cohort Investigators, Ramadass AS, Green J, Akoulitchev A, McInnes IB, Goodyear CS. Chromosome conformation signatures define predictive markers of inadequate response to methotrexate in early rheumatoid arthritis.J Transl Med. 2018; 16:18.
- Kang I, Bucala R. The immunobiology of MIF: Function, genetics and prospects for precision medicine. Nat Rev Rheumatol. 2019; 15(7):427-437.
- Maranville JC, Di Rienzo A. Combining genetic and nongenetic biomarkers to realize the promise of pharmacogenomics for inflammatory diseases. Pharmacogenomics. 2014; 15(15):1931-1940.
- Poland GA, Ovsyannikova IG, Jacobson RM. Genetics and immune response to vaccines. In: Genetic susceptibility to infectious diseases. Oxford University Press, New York. 2008; 414–429.
- Desombere I, Willems A, Leroux-Roels G. Response to hepatitis B vaccine: multiple HLA genes are involved. Tissue antigens. 1998; 51(6):593-604.
- Poland GA, Ovsyannikova IG, Jacobson RM, Vierkant RA, Jacobsen SJ, Pankratz VS, et al. Identification of an association between HLA class II alleles and low antibody levels after measles immunization. Vaccine. 2001; 20(3-4):430-438.
- Wang C, Tang J, Song W, Lobashevsky E, Wilson CM, Kaslow RA. HLA and cytokine gene polymorphisms are independently associated with responses to hepatitis B vaccination. Hepatology. 2004; 39(4): 978-988.
- Thio CL, Carrington M, Marti D, O'Brien SJ, Vlahov D, Nelson KE, et al. Class II HLA alleles and hepatitis B virus persistence in African Americans. J Infect Dis. 1999; 179(4):1004-6.
- Thursz M. Pros and cons of genetic association studies in hepatitis B. Hepatology. 2004; 40(2):284-286.
- Fischinger S,Boudreau CM ,1Butler AL, Streeck H, Alter G. Sex differences in vaccine-induced humoral immunity Semin Immunopathol. 2019; 41(2): 239–249.
- Zimmermann P, Curtis N. Factors that influence the immune response to vaccination. Clinical microbiology reviews. 2019; 32(2).
- Black FL, Schiffman G, Pandey JP. HLA, Gm, and Km polymorphisms and immunity to infectious diseases in South Amerinds. Exp Clin Immunogenet. 1995; 12:206-216.
- Mauldin IS, Wages NA, Stowman AM, Wang E, Olson WC, Deacon DH, et al. Topical treatment of melanoma metastases with imiquimod, plus administration of a cancer vaccine, promotes immune signatures in the metastases. Cancer Immunol Immunother. 2016; 65(10):1201-1212.
- Poland GA, Grabenstein JD, Neff JM. The US smallpox vaccination program: a review of a large modern era smallpox vaccination implementation program. Vaccine. 2005; 23(17-18):2078-2081.
- Halsell JS, Riddle JR, Atwood JE, Gardner P, Shope R, Poland GA, et al. Myopericarditis following smallpox vaccination among vaccinia-naive US military personnel. JAMA. 2003; 289(24):3283-3289.
- Vestergaard M, Hviid A, Madsen KM, Wohlfahrt J, Thorsen P, Schendel D, et al. MMR vaccination and febrile seizures: evaluation of susceptible subgroups and long-term prognosis. JAMA. 2004; 292(3):351-357.
- Reif DM, McKinney BA, Motsinger AA, Chanock SJ, Edwards KM, Rock MT, et al. Genetic basis for adverse events after smallpox vaccination. The Journal of infectious diseases. 2008; 198(1):16-22.
- Ovsyannikova IG, Jacobson RM, Dhiman N, Vierkant RA, Pankratz VS, Poland GA. Human leukocyte antigen and cytokine receptor gene polymorphisms associated with heterogeneous immune responses to mumps viral vaccine. Pediatrics. 2008; 121(5):e1091-1099.
- Shrestha S, Wang C, Aissani B, Wilson CM, Tang J, Kaslow RA. Interleukin-10 gene (IL10) polymorphisms and human papillomavirus clearance among immunosuppressed adolescents. Cancer Epidemiol Biomarkers Prev. 2007; 16(8):1626-1632.
- Green MS, Shohat T, Lerman Y, Cohen D, Slepon R, Duvdevani P, Varsano N, et al. Sex differences in the humoral antibody response to live measles vaccine in young adults. Int J Epidemiol. 1994; 23(5):1078-1081.
- Mitchell LA, Zhang T, Tingle AJ. Differential antibody responses to rubella virus infection in males and females. J Infect Dis. 1992; 166(6):1258-1265.
- Fish EN. The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol. 2008; 8(9):737-744.
- Goronzy JJ, Fang F, Cavanagh MM, Qi Q, Weyand CM. Naive T cell maintenance and function in human aging. J Immunol. 2015; 194(9):4073-4080.
- Lee KA, Shin KS, Kim GY, Song YC, Bae EA, Kim IK, et al. Characterization of age-associated exhausted CD 8+ T cells defined by increased expression of Tim-3 and PD-1. Aging Cell. 2016; 15(2):291-300.
- Francis T. On the doctrine of original antigenic sin. Proc Am Philos Soc. 1960; 104(6):572-578.
- Jensen KE, Davenport FM, Hennessy AV, Francis T. Characterization of influenza antibodies by serum absorption. J Exp Med. 1956; 104(2):199-209.
- Kosikova M, Li L, Radvak P, Ye Z, Wan XF, Xie H. Imprinting of repeated influenza A/H3 exposures on antibody quantity and antibody quality: implications for seasonal vaccine strain selection and vaccine performance. Clin Infect Dis. 2018; 67(10):1523-1532.
- Jang H, Ross TM. Preexisting influenza specific immunity and vaccine effectiveness. Expert Rev Vaccines. 2019; 18(10):1043-1051.
- Zhang A, Stacey HD, Mullarkey CE, Miller MS. Original antigenic sin: how first exposure shapes lifelong anti–influenza virus immune responses. J Immunol. 2019; 202(2):335-340.
- World Health Organization
- Benoit A, Beran J, Devaster JM, Esen M, Launay O, Leroux-Roels G, et al. Hemagglutination inhibition antibody titers as a correlate of protection against seasonal A/H3N2 influenza disease. Open Forum Infect Dis. 2015; 2(2):ofv067.
- Thorrington D, van Leeuwen E, Ramsay M, Pebody R, Baguelin M. Assessing optimal use of the standard dose adjuvanted trivalent seasonal influenza vaccine in the elderly. Vaccine. 2019; 37(15):2051-2056.
- Shahid Z, Kleppinger A, Gentleman B, Falsey AR, McElhaney JE. Clinical and immunologic predictors of influenza illness among vaccinated older adults. Vaccine. 2010; 28(38):6145-6151.
- McElhaney JE, Kuchel GA, Zhou X, Swain SL, Haynes L. T-cell immunity to influenza in older adults: a pathophysiological framework for development of more effective vaccines. Front Immunol. 2016; 7:41.
- Andrew MK, Bowles SK, Pawelec G, Haynes L, Kuchel GA, McNeil SA, et al. Influenza vaccination in older adults: recent innovations and practical applications. Drugs Aging. 2019; 36(1):29-37.
- McElhaney JE, Xie D, Hager WD, Barry MB, Wang Y, Kleppinger A, et al. T cell responses are better correlates of vaccine protection in the elderly. J Immunol. 2006; 176(10):6333-6339.
- Gianchecchi E, Torelli A, Montomoli E. The use of cell-mediated immunity for the evaluation of influenza vaccines: an upcoming necessity. Hum Vaccin Immunother. 2019; 15(5):1021-30.
- Isakova-Sivak I, Grigorieva E, Rudenko L. Insights into current clinical research on the immunogenicity of live attenuated influenza vaccines. Expert Rev Vaccines. 2020; 19(1):43-55.
- Jegaskanda S, Vanderven HA, Wheatley AK, Kent SJ. Fc or not Fc; that is the question: antibody Fc-receptor interactions are key to universal influenza vaccine design. Hum Vaccin Immunother. 2017; 13(6):1288-1296.
- Vanderven HA, Jegaskanda S, Wines BD, Hogarth PM, Carmuglia S, Rockman S, et al. Antibody-dependent cellular cytotoxicity responses to seasonal influenza vaccination in older adults. J Infect Dis. 2018; 217(1):12-23.
- Ng S, Nachbagauer R, Balmaseda A, Stadlbauer D, Ojeda S, Patel M, et al. Novel correlates of protection against pandemic H1N1 influenza A virus infection. Nat Med. 2019; 25(6):962-967.
- Valiathan R, Lewis JE, Melillo AB, Leonard S, Ali KH, Asthana D. Evaluation of a flow cytometry-based assay for natural killer cell activity in clinical settings. Scand J Immunol. 2012; 75(4):455-462.
- Awate S, Babiuk LA, Mutwiri G. Mechanisms of action of adjuvants. Front Immunol. 2013; 4: 114.
- Cao Y, Zhu X, Hossen MN, Kakar P, Zhao Y, Chen X. Augmentation of vaccine-induced humoral and cellular immunity by a physical radiofrequency adjuvant. Nat Commun. 2018; 9(1):1-3.
- Pleguezuelos O, Dille J, de Groen S, Oftung F, Niesters HG, Islam MA, et al. Immunogenicity, Safety, and Efficacy of a Standalone Universal Influenza Vaccine, FLU-v, in Healthy Adults: A Randomized Clinical Trial. Ann Intern Med. 2020; 172(7):453-462.
- Liu YV, Massare MJ, Barnard DL, Kort T, Nathan M, Wang L, et al. Chimeric severe acute respiratory syndrome coronavirus (SARS-CoV) S glycoprotein and influenza matrix 1 efficiently form virus-like particles (VLPs) that protect mice against challenge with SARS-CoV. Vaccine. 2011; 29(38):6606-13.
- Yong CY, Ong HK, Yeap SK, Ho KL, Tan WS. Recent advances in the vaccine development against Middle East respiratory syndrome-coronavirus. Fron Microbiology. 2019; 10:1781.
- Yang W, Petkova E, Shaman J. The 1918 influenza pandemic in N ew Y ork C ity: age-specific timing, mortality, and transmission dynamics. Influenza and other respiratory viruses. 2014; 8(2):177-88.
- Ray TK. Swine flu--an epidemiological review. J Commun Dis. 2009; 41(3):139.
- Morens DM, Fauci AS. The 1918 influenza pandemic: insights for the 21st century. J Infect Dis. 2007; 195(7):1018-1028.
- Rosenwald M. History’s Deadliest Pandemics, from Ancient Rome to Modern America. Washington Post. 2020.
- Hirsch EF, McKinney M. An epidemic of pneumococcus bronchopneumonia. J Infect Dis. 1919: 594-617.
- Gagnon A, Miller MS, Hallman SA, Bourbeau R, Herring DA, Earn DJ, et al. Age-specific mortality during the 1918 influenza pandemic: unravelling the mystery of high young adult mortality. PLoS One. 2013; 8(8):e69586.
- Brundage JF, Shanks GD. What really happened during the 1918 influenza pandemic? The importance of bacterial secondary infections. J Infect Dis. 2007; 196(11):1717-1718.
- Antonio R. Blood tests show 14% of people are now immune to covid-19 in one town in Germany. 2020.
- Fung WK, Philip LH. SARS case-fatality rates. CMAJ. 2003; 169(4):277-2778.
- Klompas M, Morris CA, Sinclair J, Pearson M, Shenoy ES. Universal masking in hospitals in the Covid-19 era. NEJ Med. 2020; 382(21):e63.
- Catherine Offord. Scientists’ latest understanding of the facts, the suspicions, and the discounted rumors of SARS-CoV-2’s transmission from person to person. 2020.
- Wickramasinghe NC, Steele EJ, Gorczynski RM, Temple R, Tokoro G, Qu J, et al. Comments on the Origin and Spread of the 2019 Coronavirus. VirolCurr Res. 2020; 4(1).
- Wickramasinghe NC, Steele EJ, Gorczynski RM, Temple R, Tokoro G, Wallis DH, et al. Growing Evidence against Global Infection-Driven by Person-to-Person Transfer of COVID-19. VirolCurr Res. 2020; 4(1).
- Steele EJ, Gorczynski RM, Rebhan, H, Carnegie P, Temple R, Tokoro G, et al. Implications of haplotype switching for the origin and global spread of COVID-19. Virol Curr Res. 2020; 4:2.
- Wickramasinghe NC, Steele EJ, Gorczynski RM, Temple R, Tokoro G, Wallis DH, et al. On The Fragility of Empires and Paradigms. Virology. 2020; 4(1).
- Steele EJ, Gorczynski RM, Lindley RA, Liu Y, Temple R, Tokoro G, et al. Lamarck and Panspermia-On the Efficient Spread of Living Systems Throughout the Cosmos. Prog Biophys Mol Biol. 2019; 149:10-32.
- Jim R. Trillions Upon Trillions of Viruses Fall From the Sky Each Day. 2018.
- Hoyle F, Wickramasinghe NC. Evolution from space. JM Dent. 1981.
- Qu, J, Wickramasinghe NC. The world should establish an early warning system for new viral infectious diseases by space-weather monitoring. MedComm. 2020; 1-4.
- Shivaji S, Chaturvedi P, Suresh K, Reddy GS, Dutt CB, Wainwright M, et al. Bacillus aerius sp. nov., Bacillus aerophilus sp. nov., Bacillus stratosphericus sp. nov. and Bacillus altitudinis sp. nov., isolated from cryogenic tubes used for collecting air samples from high altitudes. Int J Syst Evol Microbiol. 2006; 56(7):1465-1473.
- Shivaji S, Chaturvedi P, Begum Z, Pindi PK, Manorama R, Padmanaban DA,et al. Janibacter hoylei sp. nov., Bacillus isronensis sp. nov. and Bacillus aryabhattai sp. nov., isolated from cryotubes used for collecting air from the upper atmosphere. Int J Syst Evol Microbiol. 2009 ; 59(12):2977-2986.
- Grebennikova TV, Syroeshkin AV, Shubralova EV, Eliseeva OV, Kostina LV, Kulikova NY, et al. The DNA of bacteria of the World Ocean and the Earth in cosmic dust at the International Space Station. Sci World J. 2018.
- Reche I, D’Orta G, Mladenov N, Winget DM, Suttle CA. Deposition rates of viruses and bacteria above the atmospheric boundary layer. ISME J. 2018; 12(4):1154-1162.
- Wickramasinghe NC, Rycroft MJ. On the Difficulty of the Transport of Electrically Charged Submicron Dust from the Earth’s Surface to the High Ionosphere. Advances in Astrophysics. 2018; 3(3):150-153.
- Qu J, Gao Z, Zhang Y, Wainwright M, Omairi T. Sunspot activity, influenza and ebola outbreak connection. Astrobiology & Outreach. 2016; 1 -7.
- Born B, Dietrich A, Müller GJ. Do lockdowns work? A counterfactual for Sweden. 2020; 16:1-22.
- Romero HA, Pavía TA, Cervantes MA, Pliego AF, Repetto AC, Juárez ML. The dual role of the immune response in reproductive organs during Zika virus infection. Front Immunol. 2019; 10.
- Jackson BR, Chow N, Forsberg K, Litvintseva AP, Lockhart SR, Welsh R, Vallabhaneni S, Chiller T. On the origins of a species: what might explain the rise of Candida auris?. Journal of Fungi. 2019; 5(3):58.
- Jeffery-Smith A, Taori SK, Schelenz S, Jeffery K, Johnson EM, Borman A, Manuel R, Brown CS. Candida auris: a review of the literature. Clin Microbiol Rev. 2018; 31(1).
- Lockhart SR, Etienne KA, Vallabhaneni S, Farooqi J, Chowdhary A, Govender NP, et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin Infect Dis. 2017; 64(2):134-140.
- Drug Target Review. Mapping the immune response to COVID-19. 2020.
- Zhu FC, Li YH, Guan XH, Hou LH, Wang WJ, Li JX, et al. Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial. Lancet. 2020.
- Cao WC, Liu W, Zhang PH, Zhang F, Richardus JH. Disappearance of antibodies to SARS-associated coronavirus after recovery. N Engl J Med. 2007; 357(11):1162-1163.
- Choe PG, Perera RA, Park WB, Song KH, Bang JH, Kim ES, et al. MERS-CoV antibody responses 1 year after symptom onset, South Korea, 2015. Emerg Infect Dis. 2017; 23(7):1079.
- Zhao J, Zhao J, Perlman S. T cell responses are required for protection from clinical disease and for virus clearance in severe acute respiratory syndrome coronavirus-infected mice. J Virol. 2010; 84(18):9318-9325.
- Channappanavar R, Fett C, Zhao J, Meyerholz DK, Perlman S. Virus-specific memory CD8 T cells provide substantial protection from lethal severe acute respiratory syndrome coronavirus infection. J Virol. 2014 ; 88(19):11034-1044.
- Wang X, Guo X, Xin Q, Pan Y, Hu Y, Li J, et al. Neutralizing antibodies responses to SARS-CoV-2 in COVID-19 inpatients and convalescent patients. Clin Infect Dis. 2020.
- Wu F, Wang A, Liu M, Wang Q, Chen J, Xia S, et al. Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their implications. 2020.
- Weiss P, Murdoch DR. Clinical course and mortality risk of severe COVID-19. Lancet. 2020; 395(10229):1014-1015.
- Lövgren Bengtsson K, Morein B, Osterhaus AD. ISCOM technology-based Matrix MTM adjuvant: success in future vaccines relies on formulation. Expert Rev Vaccines. 2011; 10(4):401-403.
- Wang Q, Zhang L, Kuwahara K, Li L, Liu Z, Li T, et al. Immunodominant SARS coronavirus epitopes in humans elicited both enhancing and neutralizing effects on infection in non-human primates. ACS Infect Dis. 2016; 2(5):361-376.
- Grifoni A, Weiskopf D, Ramirez SI, Mateus J, Dan JM, Moderbacher CR, et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020.
- Helen B. ‘Against all odds’: The inside story of how scientists across three continents produced an Ebola vaccine. 2020.
- Rosini R, Nicchi S, Pizza M, Rappuoli R. Vaccines Against Antimicrobial Resistance. Front Immunol. 2020; 11:1048.
- Keech C, Albert G, Cho I, Robertson A, Reed P, Neal S, et al. Phase 1–2 trial of a SARS-CoV-2 recombinant spike protein nanoparticle vaccine. NEJM. 2020.
- Chandler RE. Optimizing safety surveillance for COVID-19 vaccines. Nat Rev Immunol. 2020; 20(8):451-452.
- Calina D, Docea AO, Petrakis D, Egorov AM, Ishmukhametov AA, Gabibov AG, et al. Towards effective COVID-19 vaccines: Updates, perspectives and challenges. Int J Mol Med. 2020; 46(1):3-16.
- Lambert PH, Ambrosino DM, Andersen SR, Baric RS, Black SB, Chen RT, et al. Consensus Summary Report for CEPI/BC March 12-13, 2020 Meeting: Assessment of Risk of Disease Enhancement with COVID-19 Vaccines. Vaccine. 2020; 38(31):4783-4791.
- Logunov DY, Dolzhikova IV, Zubkova OV, Tukhvatullin AI, Shcheblyakov DV, Dzharullaeva AS, et al. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia. Lancet. 2020; 396(10255):887-897.
- Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S, Belij-Rammerstorfer S, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020; 396(10249):467-478.
- Netea MG. Training innate immunity: the changing concept of immunological memory in innate host defence. Europ J Clin Invest. 2013; 43(8):881-884.
- Arts RJ, Moorlag SJ, Novakovic B, Li Y, Wang SY, Oosting M, et al. BCG vaccination protects against experimental viral infection in humans through the induction of cytokines associated with trained immunity. Cell host & microbe. 2018; 23(1):89-100.
- Rieckmann A, Villumsen M, Sørup S, Haugaard LK, Ravn H, Roth A, et al. Vaccinations against smallpox and tuberculosis are associated with better long-term survival: a Danish case-cohort study 1971–2010. Int J Epidemiol. 2017; 46(2):695-705.
- Kaufmann E, Sanz J, Dunn JL, Khan N, Mendonça LE, Pacis A, et al. BCG educates hematopoietic stem cells to generate protective innate immunity against tuberculosis. Cell. 2018; 172(1-2):176-190.
- Covián C, Fernández-Fierro A, Retamal-Díaz A, Díaz FE, VASQUEZ AE, Lay MK, et al. BCG-induced cross-protection and development of trained immunity. Implication for vaccine design. Front Immunol. 2019; 10:2806.
- U.S. National Library of Medicine. Bacillus Calmette-guérin Vaccination to Prevent Infections of the Elderly (ACTIVATE). 2020.
- U.S. National Library of Medicine. BCG Vaccine for Health Care Workers as Defense Against COVID 19 (BADAS). 2020.
- Pereira M, Paixão E, Trajman A, De Souza RA, Da Natividade MS, Pescarini JM, et al. The need for fast-track, high-quality and low-cost studies about the role of the BCG vaccine in the fight against COVID-19. Respir Res. 2020; 21(1):1-3.
- Bunnik EM, Van Gils MJ, Lobbrecht MS, Pisas L, Nanlohy NM, Van Baarle D, et al. Emergence of monoclonal antibody b12-resistant human immunodeficiency virus type 1 variants during natural infection in the absence of humoral or cellular immune pressure. J Gen Virol. 2010; 91(5):1354-1364.
- McCoy LE. The expanding array of HIV broadly neutralizing antibodies. Retrovirology. 2018; 15(1):70.
- Sharun K, Tiwari R, Iqbal Yatoo M, Patel SK, Natesan S, Dhama J, et al. Antibody-based immunotherapeutics and use of convalescent plasma to counter COVID-19: advances and prospects. Expert Opin Biol Ther. 2020; 20(9):1033-1046.
- Morgan Jr RC, Reid TN. On Answering the Call to Action for COVID-19: Continuing a Bold Legacy of Health Advocacy. J Natl Med Assoc. 2020.
Citation: Gorczynski RM (2020) Personalizing Vaccination for Infectious Disease in the 21st Century. J Vaccines Vaccin. S5:005.
Copyright: © 2020 Gorczynski RM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.