PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
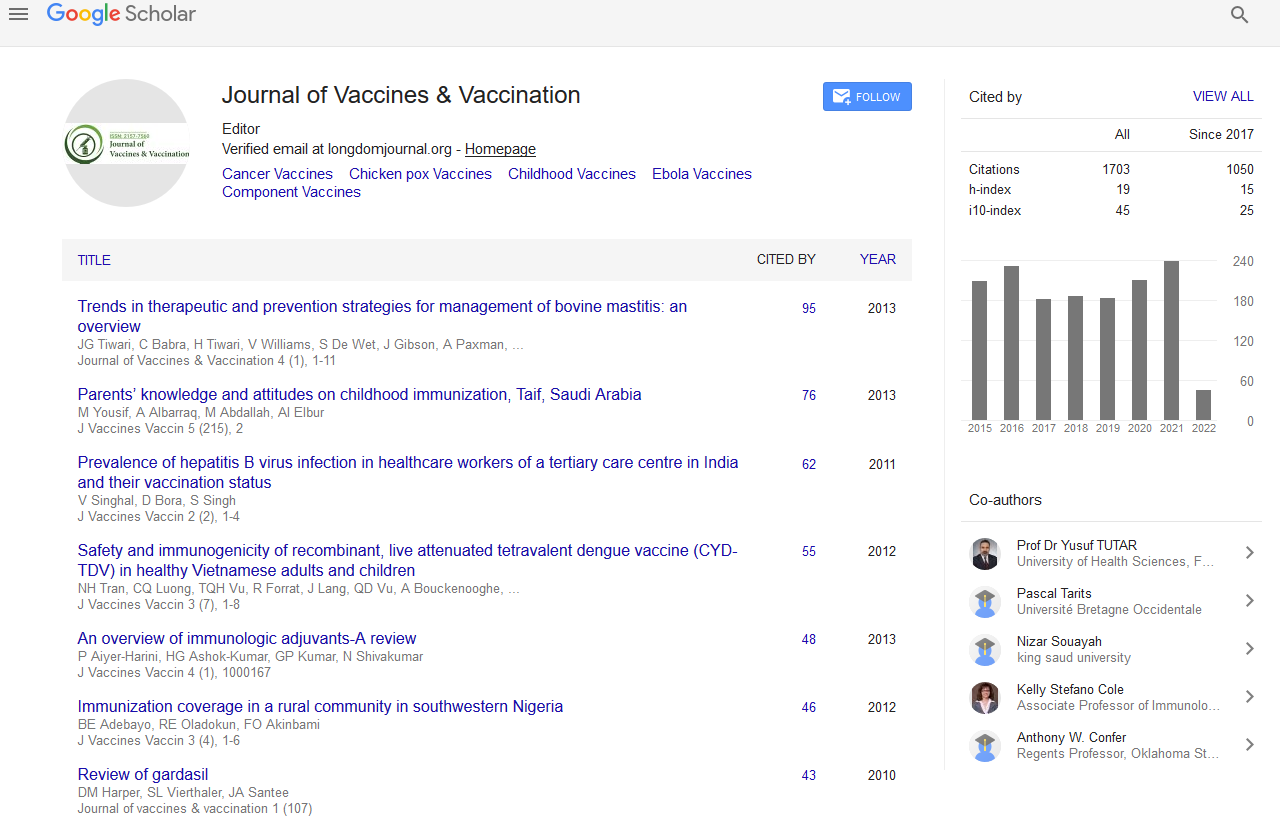
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Editorial - (2020) Volume 0, Issue 0
Pathophysiology of Crohn’s Disease
Montserrat Sanmartí*Received: 27-Nov-2020 Published: 18-Dec-2020, DOI: 10.35248/2157-7560.20.S7:e003
Introduction
Crohn's disease may be a sort of inflammatory bowel disease (IBD). It causes inflammation of your alimentary canal, which may cause abdominal pain, severe diarrhoea, fatigue, weight loss and malnutrition. Inflammation caused by regional enteritis can involve different areas of the alimentary canal in several people.
A chronic inflammatory bowel disease that affects the liner of the alimentary canal. Crohn's disease can sometimes cause lifethreatening complications. Crohn's disease can cause abdominal pain, diarrhoea, weight loss, anaemia and fatigue. Some people could also be symptom-free most of their lives, while others can have severe chronic symptoms that never get away [1].
Crohn's disease can't be cured. Medications like steroids and immunosuppressant’s are wont to slow the progression of disease. If these aren't effective, a patient may require surgery. Additionally, patients with regional enteritis may have to receive regular screening for colorectal cancer thanks to increased risk.
Symptoms
Symptoms of Crohn’s vary widely counting on the person and on the a part of the alimentary canal, or alimentary canal, that the disease attacks. In the lower alimentary canal, or colon, common symptoms include:
Belly pain and cramps, Blood in your poop, Diarrhoea, Drainage from a painful sore near your anus, Urgent bowel movements, Feeling such as you haven’t totally emptied your bowels after you poop, Loss of appetite and weight loss (talk to your doctor about this), Constipation, which can cause blocked bowel.
Causes
The explanation for regional enteritis is unknown. Crohn’s disease isn't contagious. You can't “get” it from another person. Diet can affect and trigger Crohn’s disease flare-ups; however, it's doubtful that diet causes the disease. Researchers and doctors don't know the explanation for Crohn’s disease; however, some suspect that the cause is thanks to certain bacteria, for instance, mycobacterium. Crohn's disease can cause ulcers within the intestine, colon, or both. The disease also may cause obstruction of the tiny intestine.
Diagnosis
Blood tests can help your doctor search for certain indicators of potential problems, like anemia and inflammation. A fecal occult test can help your doctor detect blood in your alimentary canal. Your doctor may request an endoscopy to urge a far better image of the within of your upper alimentary canal. Your doctor may request a colonoscopy to look at the massive bowel [2,3].
Imaging tests like CT scans and MRI scans give your doctor more detail than a mean X-ray. Both tests allow your doctor to ascertain specific areas of your tissues and organs. Your doctor will likely have a tissue sample, or biopsy, taken during an endoscopy or colonoscopy for a better check out your intestinal tract tissue. Once your doctor has completed reviewing all the required tests and ruled out other possible reasons for your symptoms, they'll conclude that you simply have Crohn’s disease.
Treatment
Treatment may involve medication, surgery, and nutritional supplements. The aim is to regulate inflammation, correct nutritional problems, and relieve symptoms. There is no cure for Crohn’s disease, but some treatments can help by reducing the amount of times a patient experiences recurrences.
Medication for Crohn’s disease
Anti-inflammation drugs-the doctor will presumably start with mesalamine (Sulfasalazine), which helps control inflammation.
Cortisone or steroids-corticosteroids are drugs containing cortisone and steroids.
Antibiotics-fistulas, strictures, or prior surgery may cause bacterial overgrowth. Doctors will generally treat this by prescribing ampicillin, sulphonamide, cephalosporin, tetracycline, or metronidazole.
Anti-diarrheal and fluid replacements-when the inflammation subsides, diarrhoea usually becomes less of a drag. However, sometimes the patient may have something for diarrhoea and abdominal pain. Immunomodulatory drugs. Biologics appear to assist people with Crohn’s disease.
Examples of biologics for Crohn’s include: Infliximab (Remicade), adalimumab (Humira), 6-mercaptopurine (Purinethol), Methotrexate, Imuran (Azathioprine), certolizumab pegol (Cimzia)
Biologic treatments can have side effects include vomiting, nausea, and a weaker resistance to infection.
REFERENCES
- Fayyaz B, Gunawan F, Rehman HJ. 'Preclinical' rheumatoid arthritis in patients with celiac disease: a cross-sectional study. J Community Hosp Intern Med Perspect. 2019;9(2):86-91.
- Podas T, Nightingale JMD, Oldham R, Roy S, Sheehan NJ, Mayberry JF. Is Rheumatoid arthritis a disease that starts in the intestine? A pilot study comparing an elemental diet with oral prednisolone. Postgrad Med J. 2007;83(976):128-131.
- Rostami K, Bold J, Parr A, Johnson MW. Gluten-free diet indications, safety, quality, labels, and challenges. Nutrients. 2017;9(8):846.
Citation: Sanmartí M (2020) Pathophysiology of Crohn’s Disease. J Vaccines Vaccin. S7:e003.
Copyright: © 2020 Sanmartí M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.