Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
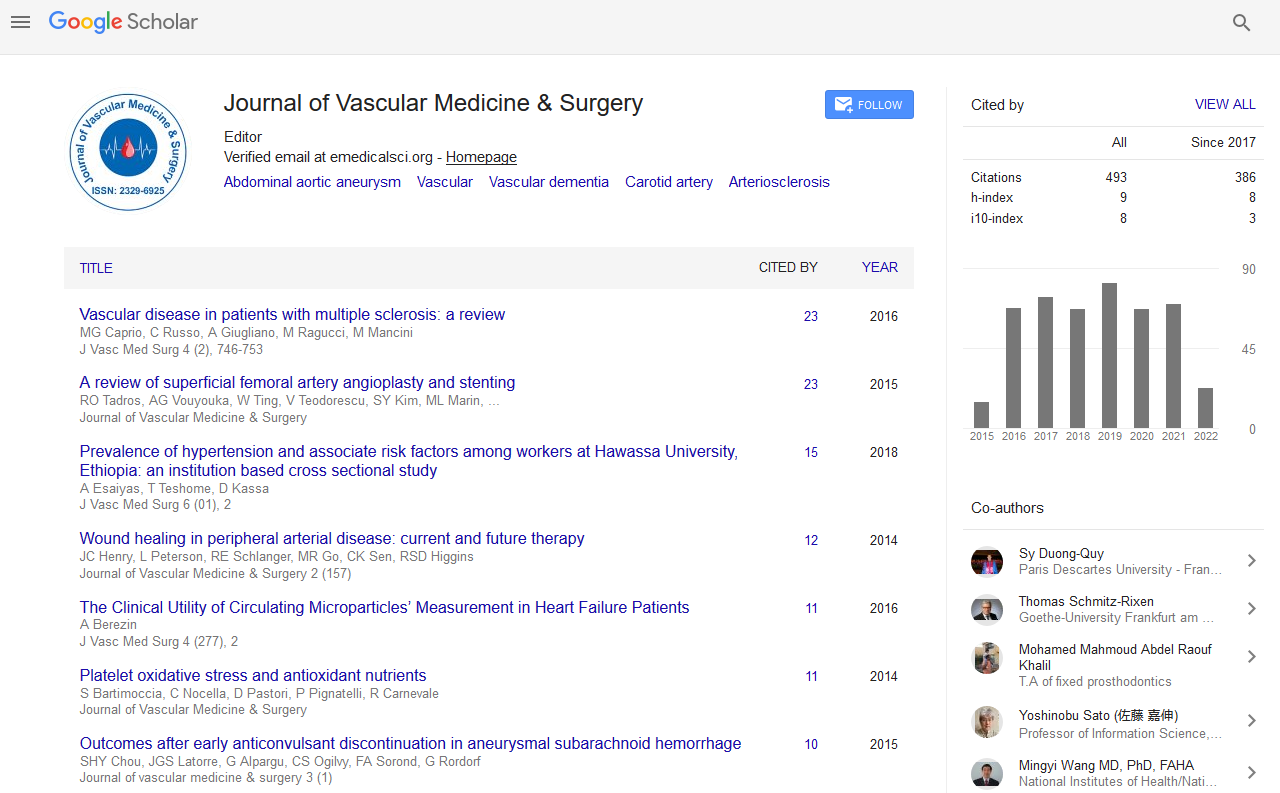
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2019) Volume 7, Issue 1
Outcome Analysis Following Iliac Endarterectomy with Ileofemoral Bypass in Patients with TASC C and D Iliac Disease
Sridhar M*, Sritharan N, Prathap Kumar S and Devarajan IReceived: 08-Jan-2019 Published: 27-Feb-2019, DOI: 10.35248/2329-6925.19.7.379
Abstract
Objective: Aim of this study is to evaluate the outcomes following unilateral iliac revascularization by iliac endarterectomy followed by ileo-femoral bypass in patients with TASC C and TASC D Aorto-iliac lesion, with respect to patency and limb salvage.
Method of study: Prospective study.
Results: A total of 26 patients underwent unilateral iliac intervention during the period from August 2016 to January 2017. Mean age at presentation was 68 years (range 45-78). Primary graft patency rate was 92% at end of 1 year. Limb salvaged rate was 100%. No early graft failure was seen. Late graft failure was seen in one patient.
Conclusion: Unilateral iliac revascularization is a viable option in patients with TASC C and D Aorto- iliac lesions, not amenable to endovascular therapy and severe comorbidities.
Keywords: Iliac endarterectomy; CLI; TASC C and D iliac disease
Keywords
Iliac endarterectomy; CLI; TASC C and D iliac disease
Introduction
Aorto-iliac disease generally affects patient of advanced ages with severe co-morbidities. And patients with advanced age were found to have diffuse disease, involving long segments and multilevel occlusion not amenable for endovascular therapy. Aorto-femoral bypass has been the standard operation, against which other results are compared. But Aorto-femoral bypass has been associated with morbidity and peri-operative mortality, especially in patients with severe co-morbidities [1].
Iliac endarterectomy followed by ileo-femoral bypass through retroperitoneal approach can be performed with regional anesthesia. It avoids the need for aortic clamping and there by avoids the effects of aortic clamping and de-clamping [2]. Extra anatomic bypasses are usually reserved for patients with poor life expectancy. Extra anatomic bypasses have poor patency and limb salvage is less in patients with critical limb ischemia [3].
Materials and Methods
A total of 26 patients underwent unilateral iliac intervention during the period from August 2016 to January 2018, at Institute of Vascular Surgery, Madras Medical College, Chennai [4]. They were followed up for a period of one year. All patients were clinically evaluated, Routine work up, Cardiac evaluation, Pulmonary function Test were done. CT Angiogram was done and patients with TASC C and D lesions were included in the study [5]. Patients wound status was stratified based on Rutherford’s Classification. All patients underwent Preoperative Anesthetic evaluation and graded using American Society Anesthesiologist (ASA) Classification System [6].
Endpoints: Primary Patency and Limb Salvage rate were the primary endpoints. Post-operative Morbidity and Mortality were secondary endpoints. Primary patency defined as patency without repeat intervention not only on the bypass and its anastomoses but also on the donor iliac artery [7].
Patient Selection Criteria: Patients with TASC C and D Aorto-iliac lesions, not amenable for endovascular therapy, and patients with severe comorbid conditions, ASA III and ASA IV were included in the study. Patients with TASC A and B Aorto-iliac lesions, and bilateral critical limb ischemia were excluded from the study [8].
Postoperative assessment: Bypass patency was assessed by clinical pulse evaluation and Ankle Brachial pressure (ABI) measurement. ABI improvement more than 0.15 of the preoperative ABI, is considered as successful bypass. Groin incisions were checked to detect complications including lymphocele, lymphorrea, and superficial or deep infection.
Follow-up assessment: Follow-up assessment was done after 1st month and after every Outpatient visit. Follow-up assessed using clinical pulse examination and Ankle brachial index measurement. Early graft failure was defined as graft thrombosis occurring within 30 days. Graft surveillance was done in those patients with ABI drop more than 0.15 of the previous value, or patients symptoms of pain and/or absence of previously palpable pulse.
Results
Between August 2016 and January 2018, 26 patients were intervened, for unilateral Iliac Lesions. Following is the observations made. Mean age at presentation was 68 years (range 45-78), comprising of 25 males and 1 female patient. Male sex was most commonly affected involving 25 of 26 patients. Baseline characteristics and risk factors observed are enumerated in the Table 1.
| Age in years | 68 (Range 45-78) |
|---|---|
| Male sex | 25(96%) |
| Female sex | 1(4%) |
| Risk factors Tobacco Alcohol consumption Diabetes mellitus Hypertension Cardiac dysfunction Respiratory dysfunction Renal failure |
24 (92%) 22 (84%) 13 (50%) 15 (57%) 10(38%) 15 (57%) 2(7%) |
| Pre-operative symptoms Non-healing ulcer Gangrene Rest pain |
6 (24%) 13 (50%) 7 (26%) |
| Iliac lesion with TASC class TASC C TASC D With SFA lesion |
15(57%) 11 (43%) 9 (34%) |
| Rutherford’s class Class 4 Class 5 Class 6 |
7(26%) 17(57%) 2(7%) |
| ASA III ASA IV |
9 (34%) 16 (61%) |
Table 1: Baseline Characteristics.
Surgical technique
All patients underwent Iliac Endarterectomy via Retro-peritoneal approach. Common Iliac artery control taken before bifurcation, Common Iliac artery transected, Eversion Endarterectomy done. Common iliac artery was used as inflow in all the cases. Ileo-femoral bypass was done in 12(46%) patients. Landing zone was either common femoral artery or profundal femoris artery. Concomitant sequential femoropopliteal or femorotibial bypasses were done in 9(34%) patients. Aorto-bifemoral conversion was required in 5 (20%) patients. Of the 5 patients who required conversion, there was a plaque disruption to opposite side in 4 patients, and one patient had an aneurysmal degeneration.
Graft patency and Limb salvage: Primary graft patency rate was 92% at end of 1 year. Limb salvaged rate was 100%. No early graft failure was seen. Late graft failure was seen in one patient. One patient had anastomotic pseudoaneurysm and blow out. He was managed with graft explantation and wound debridement. He was planned for extra-anatomic bypass, but patient declined surgery, as he was an above knee amputee on the opposite side and decided against any further intervention. One patient had late graft failure, three months after the procedure, and was managed with systemic thrombolysis. Other outcomes are detailed in Table 2.
| Procedure done Ileo-femoral bypass Ile-femoral with sequential bypass Aorto-bifemoral conversion Plaque disruption to opposite side Associated aneurysm |
12(46%) 9(34%) 5(19%) 4(15%) 1(3.8%) |
| Postoperative outcome Palpable pulse Ankle brachial index improvement |
20(76%) 6(23.7%) |
| Wound infection Major wound infection Minor wound infection/ lymphorrea Paresthesia |
2 6 1 |
| Graft thrombosis | 1 |
| Blow out | 1 |
| Toe debridement Forefoot amputation |
11 4 |
| Primary patency Limb salvage |
92% 100% |
Four patients developed plaque disruption to the opposite side, necessitating a Aorto-bifemoral conversion. In one patient there was an associated small infra-renal aortic aneurysm, needed endoaneurysmorarrphy and aorto-bifemoral bypass. Immediate post-operative outcome as suggested by palpable pulse was seen in 76% of patients and 23.7% showed improvement in ankle brachial index. Major wound infection was seen in two patients, one required sartorious flap for groin wound, and other case developed hematoma in the thigh wound which required re-exploration and evacuation of hematoma. Both cases had functioning bypass at the end of one year. Minor wound infection developed in 24% of patients and were managed conservatively with simple wound care. None of the patients required post-operative ventilation or developed cardiac events.
Discussion
Patients with unilateral Iliac occlusion, presenting with critical limb ischemia, often require Aorto-femoral bypass. Even though Aorto-femoral bypass can be done by a retroperitoneal approach, the physiological effects of aortic clamping and de-clamping, still adds to the morbidity and mortality. And the presence of severe co-morbidities adds to the complexity, regarding the mode of intervention. All though Endovascular intervention has been advocated in patients with severe co-morbidities, it has been seen that a subset of patients, have diffuse disease and often leads to failed endovascular therapy.
Iliac endarterectomy through retroperitoneal approach can be done without any of the physiological effects of aortic clamping and declamping. Iliac endarterectomy also removes the disease process at the aorto-iliac bifurcation and provides more of a physiological correction at aorto-iliac bifurcation. The operating time is reduced. Postoperative respiratory and cardiac complications are reduced.
However the risk of plaque disruption to the opposite limb should be borne in mind. Dissection and handling of the artery should be gentle.
Conclusion
Iliac endarterectomy and using the common Iliac artery as an inflow vessel in TASC C and D Aorto-iliac disease is a very useful procedure, especially in patients with severe co-morbidities and in lesions not amenable to endovascular therapy. The results following iliac endarterectomy with ileo- femoral bypass are as good as aortofemoral bypass.
REFERENCES
- van der Vliet JA, Scharn DM, de Waard JW, Roumen RM, van Roye SF, Buskens FG. Unilateral vascular reconstruction for iliac obstructive disease. J Vasc Surg. 1994;19(4):610-4.
- Ricco JB, Probst H. Long-term results of a multicenter randomized study on direct versus crossover bypass for unilateral iliac artery occlusive disease. J VascSurg. 2008;47(1):45-54.
- Cham C, Myers KA, Scott DF, Devine TJ, Denton MJ. Extraperitoneal Unilateral Iliac Artery Bypass for Chronic Lower Limb Ischaemia. Aust N Z J Surg. 1988;58(11): 859-863.
- Kretschmer G, Niederle B, Schemper M, Polterauer P. Extra-anatomic Femoro-femoral Crossover Bypass (FF) vs. Unilateral OrthotopicIlio-femoral Bypass (IF): An Attempt to Compare Results based on Data Matching. Eur J Vasc Surg. 1991;5(1): 75-82.
- Nazzal MM, Hoballah JJ, Jacobovicz C, Mohan CR, Martinasevic M, Ryan SM, et al. A Comparative Evaluation of Femorofemoral Crossover Bypass andIliofemoral Bypass for Unilateral Iliac Artery Occlusive Disease. Angiology. Angiology. 1998;49(4): 259-65.
- Harrington ME, Harrington EB, Haimov M, Schanzer H, Jacobson JH. Iliofemoral case for an versus femorofemoral bypass: The individualized approach. J Vasc Surg. 1992;16(6): 841-54.
- Kalman PG, Hosang M, Johnston KW, Walker PM. Unilateral iliac disease: The role of iliofemoral bypass. J Vasc Surg. 1987;6(2):139-43.
- Sidawy AN, Menzoian JO, Cantelmo NL, LoGerfo FW. Retroperitoneal Inflow procedures for IliacOcclusiveVascular Disease. Arch Surg 1985;120(7): 794-6.
Citation: Sridhar M, Sritharan N, Prathap Kumar S, Devarajan I (2019) Outcome Analysis Following Iliac Endarterectomy with Ileofemoral Bypass in Patients with TASC C and D Iliac Disease. J Vasc Med Surg 7:379. doi: 10.35248/2329-6925.19.7.379
Copyright: © 2019 Sridhar M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.