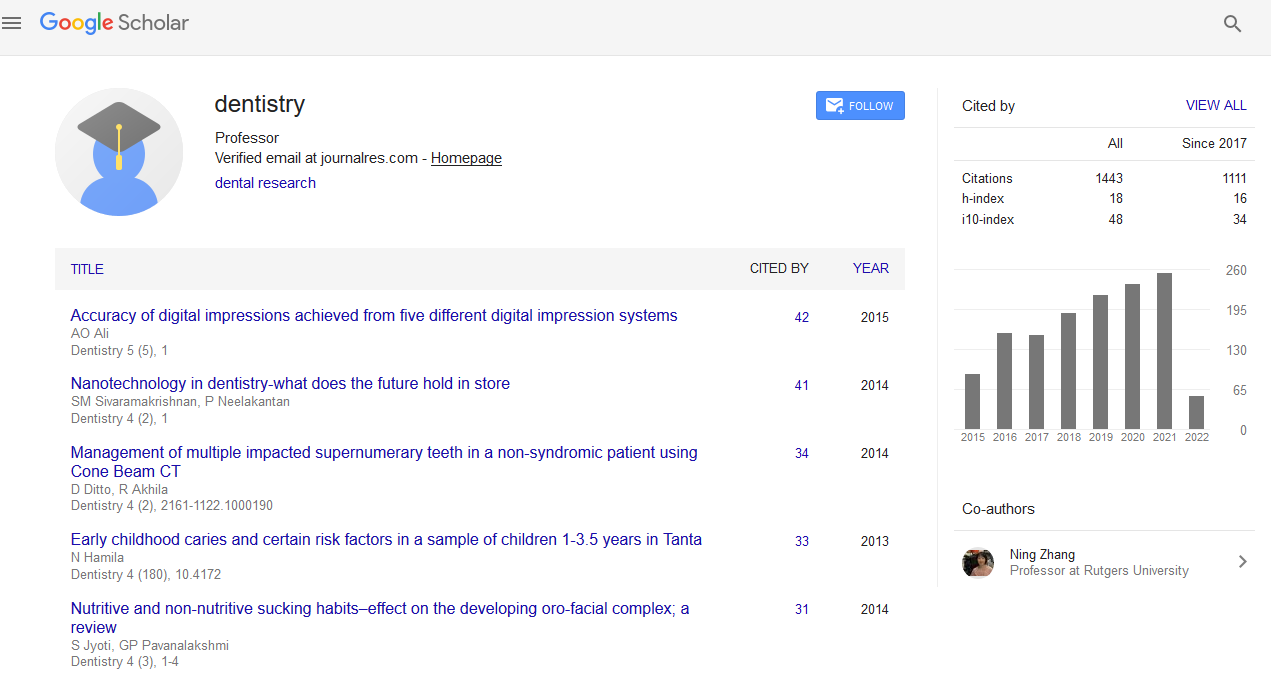
Citations : 1817
Dentistry received 1817 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2020) Volume 10, Issue 7
Orofacial Pain-An Introduction to the New Dental Specialty
Harpreet Singh*Received: 11-Aug-2020 Published: 07-Oct-2020, DOI: 10.35248/2161-1122.20.10.570
Abstract
As per the American Academy of Orofacial Pain (AAOP), Orofacial Pain (OFP) is the discipline of dentistry which includes the assessment, diagnosis and treatment of patients with orofacial pain disorders, including temporomandibular disorders, oro-motor and jaw behavior disorders, neuropathic and neurovascular pain disorders, related orofacial sleep disorders, and chronic orofacial, head and neck pain, as well as the pursuit of knowledge of the underlying pathophysiology and mechanisms of these disorders. In April 2020, American Dental Association (ADA) has approved the OFP as the 12th dental specialty in United States. The significance of orofacial pain specialty is that a trained specialist in OFP can identify all symptoms, diagnoses and causes of the pain based on the thorough evaluation. Treatment plan is developed to treat the condition which also includes training of the patient to reduce the patient-centered causes of the condition. This patient care and management will also prevent incidence of chronic pain and its consequences such as opioid addiction and other drugs, limitation in work and function, other comorbidities such as depression and anxiety, and long-term dependency on treatment. This review will briefly discuss the different aspects of OFP diagnosis.
Keywords
Orofacial pain; Specialty; Classification; Diagnosis; Categories; Disorders
Introduction
OFP is characterized as pain experienced in the orofacial region caused by diseases or dysfunction of regional structures or nervous system or by referral from distant sources. OFP is a comprehensive term consisting of numerous painful conditions or diseases affecting the area of the throat, mouth, face, head, neck, and cervical region [1]. These conditions may include various structures and may be musculoskeletal, neurological, neurovascular, neuropathic, idiopathic, and psychogenic in origin [1]. OFP affects up to 7%- 12% of the population globally. Oral health care doctors and other health care professionals, such as pain practitioners, pain neurologists and provide the early assessment to patients with OFP [2]. OFP of most common origin is due to odontogenic causes, whereas the second most common cause is musculoskeletal and neuropathological diseases [3,4]. OFP 's specialty is committed to providing evidence-based knowledge of the mechanisms of these diseases [3]. The evaluation, care, and management of OFP disorders frequently include several factors and often require an interdisciplinary approach and collaborative process with other specialties [4]. This review will briefly sum-up the different aspects of history taking, examination, diagnostic tests, and various categories in the OFP specialty.
History
It is important that chief complaint and comprehensive history be reported accurately for the correct diagnosis. The description of pain should contain the following particulars:
• Date and start of the event
• Location
• Quality
• Intensity
• Frequency
• Duration
• Remissions or changes over time
• Modifying (alleviating, precipitating, or exacerbating) factors
• Outcome of previous diagnosis or treatment
• Associated factors such as changes in taste sensation, salivary flow, clenching, wake-up and night bruxism, jaw joint locking or clicking, altered sensation, autonomic symptoms such as nasal, eye or ear symptoms such as redness and weeping of the eye, running nose, and/or drooping of the eye should also be reported
• Pain’s effect on sleep, mood, focus, memory, concentration, fatigue, and quality of life or vice versa [5]
• History of present illness, medical and dental history, medication, family history, psychosocial and sleep history, any widely diverse body pain such as fibromyalgia, osteoarthritis should be carefully assessed along with the examination [5]
Physical Examination
A physical examination is mainly divided into the following parts:
• Vital signs: Baseline blood pressure, pulse rate, respiration rate, and temperature
• Neurologic screening: Cranial nerve screening and note signs and symptoms
• General inspection: Overall appearance, asymmetry of face or jaw, presence of scars, abnormal posture, and involuntary movements
• Palpation: Masticatory and cervical muscles, joints, lymph nodes, and/or arteries
• Range of motion: Recording Temporomandibular Joint (TMJ) movements in the opening, lateral and protrusive is essential
• Ear, Nose, Throat (ENT): diseases or disorders of ENT
• Intraoral examination of the oral mucosa, tongue, soft palate, tonsils, teeth for caries, mobility, excessive wear facets (indicating bruxism), occlusion should be evaluated [5]
Diagnostic Tests
The gold standard for orofacial pain treatment is a comprehensive history, evaluation, psychosocial assessment and effective investigation that includes pain questionnaires, radiographic imaging, magnetic resonance imaging, laboratory testing, diagnostic anesthesia including dental nerve block, trigger point injection, trigger zone infiltration, intracapsular block and much more [6]. Dental X-ray such as periapical X-ray or bitewings is of great importance for odontogenic pain, while a panoramic X-ray is a very useful screening tool for TMJ, bone, or cystic lesions and is present most of the dental clinics, radiology centers, and academic centers. Various validated and informative questionnaires such as the brief pain inventory, General Anxiety Disorder (GAD) scale, Primary Health Questionnaire (PHQ), McGill pain questionnaire, and Oral Impacts on Daily Performance (OHIP) can be used [7]. Laboratory investigations such as Erythrocyte Sedimentation Rate (ESR) for conditions such as giant cell arteritis is an important diagnostic aid to know the right diagnosis. Local anesthesia infiltration is useful in the diagnosis of certain conditions such as myofascial pain [7].
The broad categories included in the OFP according to International Classification of Orofacial Pain (ICOP), 1st edition (Table 1) is:
• Disorders of dentoalveolar and anatomically related structures
• Myofascial orofacial pain
• TMJ pain.
• Lesion or disease of the cranial nerves
• Vascular and nonvascular intracranial pain disorders
• Primary headaches
• Idiopathic orofacial pain [8]
| Categories | Pain conditions |
|---|---|
| Disorders of dentoalveolar and anatomically related structures | Dental pain: Pulpal pain, periodontal pain, gingival pain |
| Oral mucosal, salivary gland and jawbone pains | |
| Myofascial orofacial pain | Primary myofascial orofacial pain: Acute and chronic |
| Secondary myofascial orofacial pain: Attributed to tendonitis, myositis, muscle spasm | |
| Temporomandibular Joint (TMJ) pain | Primary TMJ pain: Acute and chronic |
| Secondary TMJ pain: Attributed to arthritis, disc displacement, degenerative joint disease, subluxation | |
| Lesion or disease of the cranial nerves | Pain attributed to lesion or disease of the Trigeminal nerve: trigeminal neuralgia, other trigeminal neuropathic pain |
| Glossopharyngeal nerve: glossopharyngeal neuralgia, glossopharyngeal neuropathic pain | |
| Presentations of primary headaches | Orofacial migraine |
| Tension-type orofacial pain | |
| Trigeminal autonomic orofacial pain | |
| Neurovascular orofacial pain | |
| Idiopathic orofacial pain | Burning Mouth Syndrome (BMS) |
| Persistent Idiopathic Facial Pain (PIFP) | |
| Persistent idiopathic dentoalveolar pain |
Table 1. Adapted from International Classification of Orofacial Pain, Edition 1.
Disorders of dentoalveolar and anatomically related structures
This category involves OFP caused by disorders of the tooth pulp, periodontal tissues, gingiva, oral mucosa, salivary glands, or jawbone tissue [8]. The form of pain is usually acute as it lasts less than three months and is usually results from nociception and/ or inflammation [8,9]. Typically, when the causative factors are properly managed, the pain usually does not continue for an extended amount of time and after therapy/management the patient is pain-free. In general, it is of high significance to distinguish between acute and chronic pain, because chronic pain which is present more than 3 months most likely warrant specific treatment and has a less poor prognosis [9].
Myofascial orofacial pain
The myofascial orofacial pain is divided into myalgia and myofascial pain according to Diagnostic Criteria for Temporomandibular Disorders (DC-TMD) [8]. Myalgia is the most common myofascial disease and the conditions for its diagnosis are muscle pain that is caused by the movement of the jaw and the palpation of the masseter or temporalis causes identical pain [7,8]. With myofascial pain, the pain occurs inside the muscle boundary, and if the pain is referred to other external systems, it is known as myofascial pain with referral [8,9] (Table 2).
| Categories | Frequency | Pain conditions |
|---|---|---|
| Musculoskeletal | Unilateral or bilateral continuous or episodic | TMD |
| Persistent orofacial muscle pain | ||
| Neuropathic | Unilateral continuous | Post-herpetic neuralgia |
| Unilateral episodic | Trigeminal neuralgia (Classical) | |
| Bilateral continuous | Burning mouth syndrome | |
| Vascular | Unilateral/bilateral continuous | Post stroke pain |
| Giant cell arteritis | ||
| Primary headache | Bilateral continuous/episodic | Tension-type headache |
| Unilateral episodic | Episodic migraine | |
| Unilateral continuous | Chronic migraine | |
| Mixed | Unilateral/bilateral continuous | Persistent idiopathic facial pain |
| Cancer pain |
Table 2: Various orofacial pain conditions.
TMJ pain
Similar to other orofacial pain, TMJ pains are also classified into primary and secondary subtypes based on the chronic pain classification by the International Association for the Study of Pain (IASP). Primary TMJ pain is that occurs even at resting jaw or while movement or palpation of the jaw, without known causative factor and is mostly localized. Secondary TMJ pain triggered by other known conditions such as inflammation (due to injury, infection, crystal deposits, or autoimmune diseases), tissue sensitization, or any structural changes (osteoarthrosis, displacement, or subluxation). The diagnosis is completely associated with TMJ pain from the DC -TMD criteria [8,10].
Lesion or disease of the cranial nerves
Pain that is caused by a primary lesion or nervous system dysfunction is known as neuropathic pain [3]. Neuropathic pain can, however, be an idiopathic phenomenon that indicates irregular sensory perception in the Peripheral Nervous System (PNS) or Central Nervous System (CNS) but with no associated pathological lesion. Upon physical insult or illness affecting the PNS or CNS, secondary neuropathic pains occur [11].
Presentations of primary headaches
As per ICOP primary headache patients divided into mainly three categories. Firstly, the patients who experience additional ipsilateral face pain during the headache attacks. Secondly, the patients whose headache attacks ceased and were substituted by face pain episodes of the same character, duration, and severity. Lastly, headache naïve patients with or without the associated symptoms of these types of headaches that develop new OFP attacks which is identical to the primary headache in pain quality, duration, and severity [8].
Idiopathic orofacial pain
Unexplained oral and facial pain that may be unilateral or bilateral usually in the distribution area of the trigeminal nerve(s) or its branches. The pain is usually constant, intermittent, moderate in intensity, and characterized mainly as dull, pressurizing, or burning [8,10].
Conclusion
OFP specialty sets high standards for efficiency and integrity of evidence-based care and ensures continuity with existing guidelines in orofacial pain management among dental and medical clinics, emergency centers, and hospital practices. The key significance of this specialty is to combat, protect, and represent the public and to access evidence-based care. With emergence of new specialty in dentistry, patients with acute and chronic oro-facial pain conditions will have more access to orofacial pain specialist and therefore, diagnosis and management of these patients will be done with greater care. As it is scientifically proven that chronic pain is a disease not a symptom and can be preventable by improving the awareness of the patient and healthcare personnel and also by collaborating with other health providers.
Conflict of Interest
None
REFERENCES
- Shaefer JR, Khawaja SN, Bavia PF. Sex, gender, and orofacial pain. Dent Clin N A. 2018;62:665-682.
- Zakrzewska JM. Multi-dimensionality of chronic pain of the oral cavity and face. J Headache Pain. 2013;14:37.
- Jerolimov V. Temporomandibular disorders and orofacial pain. Med Sci. 2009;33:53-77.
- Šklebar D, Šklebar I, Cesarik M, Barada A, Maletić A. Neuropathic orofacial pain-diagnostic and therapeutic challenges. Period Biol. 2015;117:231-237.
- http://www.quintpub.com/display_detail.php3?psku=B6102#.X3UabWhKjIU.
- Greene CS. Managing the care of patients with temporomandibular disorders: a new guideline for care. J Am Dent Assoc. 2010;141:1086-1088.
- Zakrzewska JM. Differential diagnosis of facial pain and guidelines for management. Br J Anaesth. 2013;111:95-104.
- https://journals.sagepub.com/doi/full/10.1177/0333102419893823.
- Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. 2015;156:1003-1007.
- Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for Temporomandibular Disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. 2014;28:6-27.
- https://s3.amazonaws.com/rdcms-iasp/files/production/public/Content/ContentFolders/Publications2/FreeBooks/Classification-of-Chronic-Pain.pdf.
Citation: Singh H (2020) Orofacial Pain-An Introduction to the New Dental Specialty. Dentistry 10:570. doi: 10.35248/2161-1122.20.10.570
Copyright: © 2020 Singh H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : Nil