Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 4, Issue 1
Oesophageal Perforation Management in a Tertiary Care Hospital
Usha R Dalal, Ashwani K Dalal*, Ravinder Kaur, Lakesh Anand and Ashish DuaReceived: 06-Jan-2020 Published: 27-Feb-2020, DOI: 10.35248/2684-1606.20.4.127
Abstract
Recognition of oesophageal injury is often delayed due to its protean manifestations. Principles of management are: control of sepsis and contamination by diversion and/or drainage, nutrition, broad spectrum antibiotics and restoration of continuity. Age, general condition of the patient, aetiology, the anatomical location and size of perforation, early versus delayed presentation, clinical condition of the patient, underlying oesophageal disease and other associated co-morbid medical conditions are important determinants of the outcome. Primary repair is the gold standard treatment in early hours. Drainage and diversion are required when perforation is not localised and in late and unstable cases. Endoscopic stenting with drainage may be useful in selected cases. Oesophagectomy is required in extensive damage, stricture or carcinoma.
We retrospectively analyzed the data of nine patients of oesophageal injuries managed in a tertiary care hospital from 2009 to 2019. Various causes of oesophageal injury were; spontaneous perforation in 3 cases, foreign bodies in 3 cases (one each of razor blade, coin, denture), blunt trauma chest in one case, iatrogenic injury in 2 cases (one during cervical spine fixation and another due to endoscopic dilatation of corrosive oesophageal stricture). Mainstay of the treatment was: nutritional support, control of sepsis with antibiotics and drainage and/or diversion with early or delayed repair of the rent. Transhiatal esophagectomy was done in one patient. Out of eight patients who survived, oesophageal injury was diagnosed within 24 hours in only one case; however, in seven patients it was diagnosed after 24 hours. One case of delayed presentation died due to uncontrolled sepsis and multi-organ failure.
Keywords
Oesophageal perforation; Oesophageal injuries
Introduction
The true incidence of oesophageal perforation is not clear due to paucity of literature, reporting bias and publication bias [1].The treatment principles are based on different institutional series of patients diagnosed over a period of decades [2-5]. Prompt and repeated imaging studies in cases of high index of suspicion for early diagnosis and careful selection of operative versus nonoperative treatment by experienced clinician can translate into better outcomes in these patients. The morbidity and mortality following oesophageal perforations are significant [6,7].Management strategies are operative interventions (primary/delayed repair/drainage/diversion procedures, resection) or non-operative approach or endoscopic stenting or a hybrid approach (by endotherapy, placement of drains and/or diversion procedures [8,9]. The aim of this review is to analyze aetiology, detailed clinical profile and the management outcome of oesophageal injuries admitted in a tertiary care hospital with pertinent review of literature.
Materials and Methods
A total of nine patients of oesophageal perforation over a period of ten years (2009 – 2019) were included in the study. The demographic data including aetiology, age, gender, early versus delayed presentation, clinical features, radiological findings, treatment rendered and outcome were compiled from the medical records (Table 1).
| Group | S.No. | Cause | Age and Sex | Location | Early/Delayed Presentation | Clinical Presentation | Radiological Findings | Management | No. Of Admissions | Hospital Stay | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 1 | Spontaneous | 46 M | Lower 3rd | Early | Acute chest pain,Dyspnoea,Crepitus neck. | CXR showing Left sided hyderpneumothorax. CECT showing leak of contrast from lower oesophagus in left pleural cavity. | Primary repair, feeding J and drainage. | 1 | 2 Weeks | Survived |
| 2 | Spontaneous | 55 F | Lower 3rd | Delayed | Chest pain, Dyspnoea. | CXR showing Rt hyderopneumothorax, CT chest chest, leak from lower 3rd Oesophagus. | Drainage, diversion and feeding J. | 2 | 6 Weeks | Survived | |
| 3 | Spontaneous | 25 M | Lower 3rd | Delayed | Chest pain,Dyspnoea, Fever. | CXR showing B/L hyderopneumothorax. CT chest, leak Lower 3rd oesophagus | Drainage, diversion and feeding J. | 2 | 3 Weeks | Death | |
| B | 1 | Razor Blade | 35 M | Upper Thoracic | Delayed | Chest pain,Dysphagia, Fever and Crepitus neck. | CXR and CT showing Razor blade in upper chest and surgical emphysema | Retreival, primary repair and drainage. | 1 | 2 Weeks | Survived |
| 2 | Coin | 8 M | Upper Thoracic | Delayed | Chest pain, Dyspnoea, Dysphagia, Fever, following endoscopic retrieval. | CXR and CT showing B/L pneumothorax and surgical emphysema. | Drainage, diversion,cholecystectomy,Jejunal perforation repair,feeding J, and delayed repair of oesophageal perforation. | 2 | Survived | ||
| 6 Months | |||||||||||
| 3 | Hooked Denture | 50 m | Lower Cervical | Delayed | Chest pain, Fever Dysphagia, Abdominal wall and Scrotal abscess following endoscopic retreival. | CXR showing Rt sided hyderopneumothorax,CT chest showing Rt hyderopneumothorax and collection communicating with mediastinum and retroperitoneum. | Drainage, Nasogastric feed. | 1 | 6 Weeks | Survived | |
| C | 1 | Endoscopic Dilation | 44 M | Mid Thoracic | Delayed | Chest pain,Fever, Dysphagia,Dyspnoea, | CXR showing Rt sided hyderpneumothorax and surgical emphysema. CT showing huge mediastinal collection and contrast leak from mid oesophagus. | Drainage and feeding J followed by THE | 2 | 4 Months | Survived |
| 2 | Cervical Spine Fusion | 40 M | Cervical | Delayed | Neck pain and Fever | None | Primary repair | 1 | 3 weeks | Survived | |
| D | 1 | Blunt Trauma Chest and Abdomen | 35 M | Mid Thoracic | Delayed | Chest pain, Dyspnoea. | CXR showing Rt sided hyderthorax. CT showed Rt sided hyderothorax and leak from lower oesophaugus. | Drainage and feeding J followed by delayed repair at 6 weeks. | 2 | 4 Months | Survived |
Table 1: General Information about patients.
The patients were categorised into four broad groups according to the aetiology of perforations. Group A (Spontaneous Perforation), Group (Foreign bodies), Group C (Iatrogenic), and Group D (Blunt Trauma). Along with supportive care and resuscitation (nil orally, broad spectrum antibiotics, nutrition and ICU care), the patients were managed by hybrid of various interventions i.e. drainage, diversion, decortications, feeding jejunostomy, exploratory laparotomy and oesophagectomy (Table 1).
Group A: Spontaneous perforation
Case 1: A 46 years male was admitted in medical emergency with severe chest pain and dyspnoea following forceful emesis after a heavy meal the previous night. The vitals were stable and there was subcutaneous in the cervical region. There was left sided hydro-pneumothorax in preliminary CXR. CECT chest findings suggested lower oesophageal rupture (Figure 1). Left antero-lateral thoracotomy revealed a 5 cm long tear in the left postero-lateral wall of oesophagus near gastro-oesophageal junction. Primary suture repair over a T-tube of 14 Fr size along with feeding jejunostomy were done. Patient was allowed orally after 2 weeks and discharged. Feeding jejunostomy and T-tube were removed after 6 weeks.
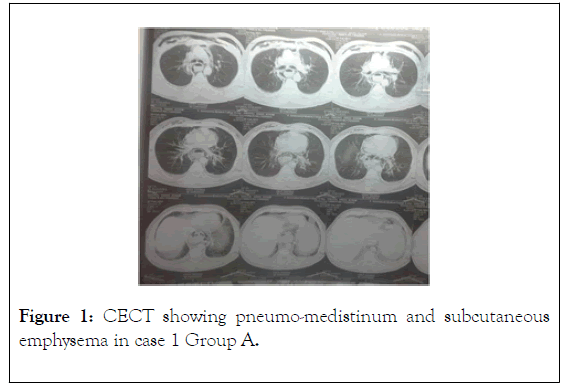
Figure 1. CECT showing pneumo-medistinum and subcutaneous emphysema in case 1 Group A.
Case 2: A 55 years old female developed sudden right sided chest pain following vigorous laughing after a heavy lunch. At periphery right sided intercostals drain was put for right hydropneumothorax. She was referred to GMCH for further management as the intercostals drain was draining ingested food material. CECT showed leak from right border of lower thoracic oesophagus. Loop cervical oesophagostomy with closure of distal end of the loop oesophagostomy along with feeding Jejunostomy were done. The oesophageal continuity was restored after 6 weeks when the contrast study did not reveal any leak. Patient was discharged in satisfactory condition with normal oral intake.
Case 3: A 25 years old young male with alcohol dependence developed sudden chest pain following forceful induced emesis after heavy water intake as a Yoga maneuver for de-addiction. He developed high grade fever after one day for which he took treatment from private practitioner. Chest X-ray done at periphery after two days revealed left sided hydrothorax (Figure 2). The case was referred to Pulmonary Medicine Department emergency with provisional diagnosis of pneumonitis. Intercostal drain put in the left thoracic cavity for hydrothorax drained one litre of blood stained contents (Figure 3). Fever continued and patient did not improve. Repeat Chest X-ray showed hydrothorax on right side also for which intercostals drain was put in right thoracic cavity. Right sided chest drain also drained fresh blood stained food contents. Patient developed features of systemic sepsis and a CECT chest done after ten days revealed lower oesophageal rupture (Figure 4). Patient was shifted in ICU for IPPV in view of continuing respiratory distress and sepsis and a surgical consultation was taken. Due to poor clinical condition, only cevical loop oesophagostomy with closure of distal lumen of the oesophagostomy and a feeding jejunostomy were done. Patient sepsis could not be controlled and he died after 15 days due to multiorgan failure.
Figure 2. X-ray chest of case 3 of group a, showing left sided hyderothorax.
Figure 3. Intercostal tube drainage in left thoracic cavity showing blood stained contents in group a case 3.
Figure 4. CECT chest of case 3, group A, showing right sided hyderothorax.
Group B: Foreign body injury
Case 1: A 35 years old male ingested razor blade with suicidal intention and he presented in surgery emergency after 3 days with dysphagia, neck pain, fever and crepitus in the neck. Chest X-ray PA view and CECT chest showed razor blade perforating the upper part of thoracic oesophagus (Figures 5 and 6). Emergency exploration was done by left cervical approach and the razor blade which had perforated the left lateral wall of the upper thoracic oesophagus was retrieved and a primary repair of the rent was done. Wound was closed over a drain. Patient was discharged after ten day.
Figure 5. X-ray chest of case 1, group B showing razor blade in upper thoracic oesophagus.
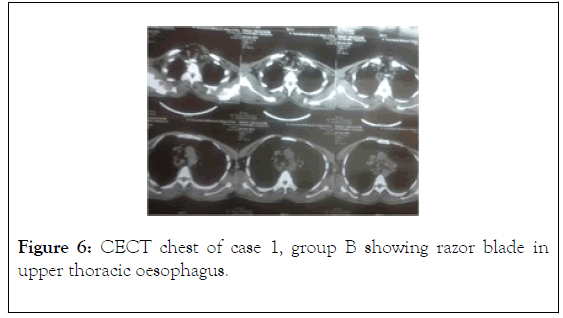
Figure 6. CECT chest of case 1, group B showing razor blade in upper thoracic oesophagus.
Case 2: An 8 years male child was referred to Paediatric Emergency Department with neck pain, fever, dysphagia and respiratory distress 3 days after endoscopic retrieval of a coin by a private practitioner. Crepitus in the neck was present. Broad spectrum antibiotics and steroids were given with provisional impression of brochospasm. He was intubated and kept on IPPV. Chest X-ray showed pneumo-mediastinum and right side pneumothorax for which ICD was inserted. ENT consultation ruled out iatrogenic airway injury. On 4th day of admission while on IPPV, broad spectrum antibiotics, analgesics and steroids, suddenly ICD started draining fresh blood, with sudden abdominal pain and distension. There were clinical features of peritonitis. USG and CECT revealed gross free fluid in the abdomen and pleural effusion in right chest. Emergency exploratory laparotomy findings were: a two centimetre duodenal perforation with active gastro-duodenal artery bleed and a two centimetre gall bladder perforation at its neck with massive haemoperitoneum and bile in the abdominal cavity probably due to due to sepsis, steroids and analgesics. Cholecystectomy, repair of duodenum over tube duodenostomy, decompression gastostomy and feeding jejunostomy were done. ICD was inserted in the left pleural cavity. An oral feed trial after four weeks showed food particles in the right side ICD. CECT chest suspected a significant oesophageal leak near carina and patient was kept only on feeding jejunostomy. Inspite of a 3 months conservative trial, leak was persistent Oesophgogram with Gastrografin revealed collection and leak near carina. Right thoracotomy for decortications and repair of the oesophageal rent was undertaken after another one month. Decortication done, however, leak could not be localised in the thorax. A repeat contrast study with Barium showed the contrast leak from cervical oesophagus which was explored with left cervical approach and rent was repaired. Patient was discharged drain free after 14 days.
Case 3: A 50 years old male ingested a hooked denture during sleep and endoscopic retrieval of the denture was done in a private hospital. After 48 hours patient developed high grade fever and antibiotics started. After one week, he developed cellulitis of the left lower abdominal wall and scrotum. An abdominal drain was inserted after incision and drainage of pus from scrotum and lower abdomen and patient was referred to GMCH Chandigarh (Figure 7). Chest X-ray revealed hydrothorax on left side for which an ICD was inserted and it drained about 2 litres of foul smelling fluid. Broad spectrum antibiotics were started and fever subsided. A CECT of chest and abdomen was done, which showed a minor leak in cervical oesophagus and the abdominal tube drain in posterior mediastinum which was used to drain scrotal abscess (Figure 8). An endoscopic guided nasogastric tube was inserted for feeding purpose (Figure 9). ICD drain subsided completely after 4 weeks and it was removed. He was discharged with nasogastric tube feeding for another 2 weeks after which full oral feeding was resumed.
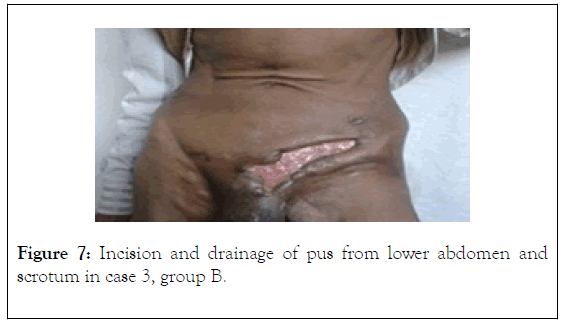
Figure 7. Incision and drainage of pus from lower abdomen and scrotum in case 3, group B.
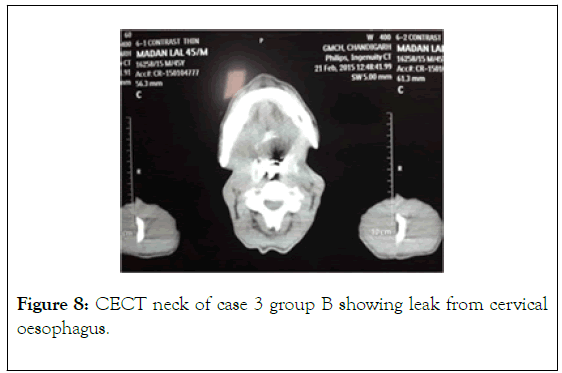
Figure 8. CECT neck of case 3 group B showing leak from cervical oesophagus.
Figure 9. Nasogastric tube inserted endoscopically for feeding purpose in group B case 3.
Group C: Iatrogenic injuries
Case 1: A 44 years old male was getting repeated endoscopic dilatation for corrosive oesophageal stricture in Medicine Department. During the 3rd time of dilatation, he developed chest pain and procedure was abandoned. Antiboitics started but patient developed high grade fever and respiratory distress. Chest X- ray revealed air and fluid with widening of the mediastinum and surgical emphysema in the subcutaneous tissues (Figure 10). CECT done after 4 days showed huge fluid collection in mediastinum which was protruding in the right pleural cavity compressing the right lung. Emergency right sided limited anterior thoracotomy was done and 2 litres of foul smelling pus was drained from the mediastinum. Thoracotomy was closed with an ICD drain in the mediastinum and a feeding jejunostomy was done in view of underlying oesophageal stricture. ICD was removed after 3 weeks. Transhiatal oesophagectomy with gastric pull up was done after 3 months as a definitive treatment for oesophageal stricture. Patient had an uneventful recovery.
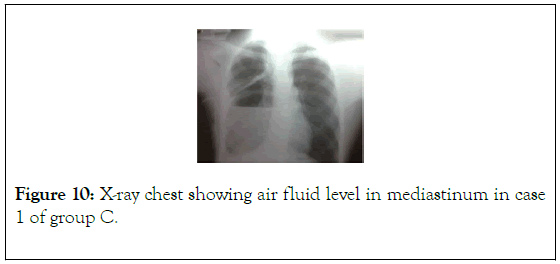
Figure 10. X-ray chest showing air fluid level in mediastinum in case 1 of group C.
Case 2: A 40 years old male had undergone anterior cervical spine fusion. On the 2nd postoperative day patient developed fever and the negative suction drain started draining copious amount of clear fluid. Surgical consultation was taken. Patient was re-explored and a 2 cm rent on the posterior wall of oesophagus was repaired. Postoperative recovery was uneventful.
Group D: Blunt trauma abdomen and chest
Case: A 35 years old male was admitted in private hospital after blunt trauma of chest and abdomen by high speed motor vehicle road side accident. The Chest X-ray showed left side hydropneumothorax for which an ICD was inserted which drained blood and food material. Exploratory laparotomy with upper midline incision was done to rule out stomach injury by ICD; however stomach and all other abdominal viscera were normal. Endoscopy and CECT chest findings were suggestive of a large rent in lower thoracic oesophagus near gastrooesophageal junction. Patient was referred to GMCH after 15 days with ICD in situ. Patient was kept nil orally and feeding jejunostomy was done for nutrition. Eventually patient developed left sided empyema and non-expanding lung in the course of treatment and ICD drainage did not decrease even after 8 weeks. A repeat contrast study with Gastrografin to localize the exact anatomical location of the oesophageal perforation was done before definitive surgery of repair and again a leak near GE junction was suggested. Thin barium contrast study was also done to ensure the location and the same findings were suggested. By left postero-lateral thoracotomy, decortication and oesophageal repair of a 4 centimetre longitudinal rent of mid thoracic oesophagus just below the arch of aorta were done. There was a minor leak which subsided after ten days.
Results
A total of nine cases of oesophageal injuries were treated in Surgery department. Male to female ratio was 8:1. The age ranged from 8 years to 55 years. The interval between perforation and diagnosis exceeded 24 hours in 8 cases. 4 cases were directly admitted in Surgery department, 2 cases were referred from Medicine and one case each from Pulmonary Medicine, Paediatric Medicine and Neurosurgery department.
One case of spontaneous oesophageal perforation with its early recognition and primary repair within 24 hours had speedy recovery. 8 cases presented after 24 hours and despite delayed diagnosis, 7 patients survived. Only one patient of spontaneous oesophageal perforation with delayed recognition died due to ongoing sepsis. Total hospital stay ranged from two weeks to 3 months and seven patients required more than one admission for staged interventions.
There were 3 cervical, one upper thoracic, 2 mid thoracic and 3 lower thoracic oesophageal perforations. One patient of lower thoracic oesophageal rupture died. Out of 3 cervical perforations, two presented after endoscopic retrieval of foreign body (one each of a coin and a denture) and one occurred during anterior cervical spine discectomy and fusion. All these presented in Surgery Department after 24 hours. The child with coin ingestion was managed with multiple interventions: first intercostal drainage for right side pneumothorax, then exploratory laparotomy (for duodenal perforation, active gastroduodenal artery bleed and gall bladder perforation along with feeding jejunostomy), later on right thoracotomy for empyema and finally oesopheal perforation repair. The second patient presented with high grade fever along with lower anterior abdominal and scrotal cellulitis and collection 4 days after endoscopic retrieval of denture from cervical oesophagus. Drainage (for collections in right pleural cavity, retroperitoneum and scrotum), nil orally, broad spectrum antibiotics, nutritional support by long nasogastric tube resulted in spontaneous healing of oesophageal leak. In case of cervical oesophageal injury during anterior cervical fusion presenting after two days, primary repair was successful.
In the patient upper thoracic perforation due to razor blade who presented on third day of ingestion, retrieval of razor blade and primary suture repair of perforation was successful.
Patient of corrosive oesophageal stricture who sustained mid thoracic oesophageal perforation during endoscopic dilatation was managed by ICD drainage of mediastinal collection by right anterior thoracotomy and a feeding jejunostomy in emergency. Definitive surgery by transhiatal oesophagectomy with gastric pull up was done after 3 months.
Patient of mid-thoracic oesophagus injury due to blunt abdominal and chest trauma presented with left hydrothorax. He underwent multiple interventions: initial exploratory laparotomy at periphery with impression of traumatic diaphragmatic hernia as ICD was draining ingested food particles, second laparotomy for a feeding jejunostomy and after 3 months left posterolateral thoracotomy for decortication and repair of rent.
The various clinical symptoms and signs were: neck or chest pain, dysphagia, dyspnoea, crepitus, fever and in case of anterior cervical fusion copious amount of drain output. In chest X-ray posteroanterior films findings were: subcutaneous/mediastinal air, pneumothorax, widening of mediastinum and evidence of pleural fluid favoured the diagnosis. The CECT done in 8 cases although estabilished the diagnosis of oesophageal injuries, however, it could not localise the exact anatomical site in two cases (in child with coin ingestion and in case of blunt injury chest and abdomen). Gastrograffin study also failed to localise the site of leak in these cases. Barium study could localise the exact site of perforation in child, but not in case of perforation due to blunt trauma. Endoscopy was done for retrieval of foreign body, dilatation of corrosive oesophageal stricture and localisation of oesophageal injury (coin/denture ingestion and blunt trauma case). However, it failed to provide exact anatomical localisation of perforation.
Discussion
Anatomy of oesophagus, lack of serosa, proximity to vital structures, diversity of symptoms and signs, delayed diagnosis, rarity of this condition, and lack of experience are the important causes of delayed recognition of oesophageal perforations. Leaked salivary, gastro-oesophageal and enteric contents incite a chemical burn in mediastinum, pleural and peritoneal cavity and may lead to sequestration of large amount of fluids further exacerbating sepsis and hypotension with significant morbidity and mortality [10,11]. Mortality for oesophageal perforation in intra-thoracic region is 18%, in cervical region is 8% and in intra-abdominal oesophageal perforation is 3%. Early recognition with timely intervention is crucial for early recovery.
Aetiology
Spontaneous transmural rupture of the oesophagus due to sudden rise in intraluminal pressure of oesophageal lumen after induced forceful or prolonged emesis i.e Boerhaave’s Syndrome represents only 15% of cases [12]. Other causes of increased intraluminal pressure are severe retching, forceful swallowing, forceful laughing (especially after heavy meals), forceful childbirth, forceful defaecation and heavy weight lifting, status epilepticus, Heimlich maneuver. Abbott and colleagues described three factors resulting in oesophageal rupture: (1) increased intraluminal pressure, (2) pre-existing oesophageal disease and (3) neurogenic causes, each of which independently can cause perforation but they are usually combined in an individual patient.12 The site of rupture is left postero-lateral aspect just above the diaphragm due to an anatomical weakness in this area resulting from the reduced number and size of longitudinal smooth muscle fibres and from entrance of nerves and blood vessels into oesophageal wall.
Iaterogenic injury following oesophageal instrumentation for diagnostic and therapeutic endoscopy accounts for nearly 60% of all oesophageal perforations [13,14]. The common procedures known for the increased risk of oesophageal procedures are: sclerotherapy for oesophageal varices, attempt to remove foreign body, dilatations and stent, endoscopic resections, temperature probe, repeated attempt for endotracheal intubation. With increasing use of flexible endoscopy the incidence of injuries is likely to increase. Iatrogenic injuries may also occur during Heller’s myotomy, pneumonectomy, truncal vagotomy (0.5%), thyroid surgery and anterior cervical spine fusion [15-18].
Retained or impacted foreign bodies both blunt and sharp are can cause oesophageal perforations eg. In children swallowing of coin/battery cell and a piece of artificial denture in adults. Oesophagus gets injured either due to impaction or during attempted retrieval by endoscopy especially when the foreign body is pushed distally into the stomach too vigorously [19].
Oesophageal perforation may occur due to ingestion of caustic liquids, cleaners, battery [20,21]. Acid cause coagulative tissue necrosis with lower risk of perforations while alkalies produce liquifactive necrosis that rapidly becomes transmural.
Oesophageal injuries can also occur in air blast trauma, gunshot injury, peneterating injury and external blunt trauma [22,23]. Incidence of injury due to blunt trauma is only 0.001% and most commonly seen in violent high speed vehicular accident, the common site being cervicothoracic oesophagus proximal to carina [24]. Penetrating objects injure the oesophagus more commonly than blunt trauma [25].
Clinical presentation
In recent perforations, symptoms may be mild or subtle. Common presenting complaint is pain. The site of pain is: in neck in case of cervical oesophagus injury, in chest which may refer directly to back in thoracic oesophageal injury, in abdomen in intra-abdominal oesophagus injury which may refer to left shoulder in 70%-90% of cases. Pain may be preceded by forceful or repeated episodes of vomiting or in about 25% of cases pain is followed by vomiting and shortness of breat. Dyspnoea is more common in thoracic oesophageal perforations than in cervical or abdominal oesophageal perforations. The triad of vomiting, chest pain and subcutaneous emphysema is known as Meckler triad [26]. Dysphonia, hoarseness of voice, dysphagia and crepitus in neck or chest wall are other important clinical features suggestive of mediastinitis. Hamman's sign (rarely, Hammond's sign or Hammond's crunch) is a crunching, rasping sound, synchronous with the heartbeat, heard over the precordium in mediastinal emphysema and is produced by the heart beating against air-filled tissues[27]. Oesophageal ruptures rarely manifest with haemetemesis or malena. Twenty- four to forty- eight hours after injury, frank sepsis with tachycardia, tachypnoea, fever, hypotension, altered mental status, and respiratory failure can become evident.
Investigations
Unfortunately, no diagnostic investigation is perfect in the evaluation of oesophageal perforation. Considerable judgement is required to decide the order and number of diagnostic studies based upon the clinical suspicion, information desired, patient tolerance, and possible therapeutic considerations.
A normal radiology does not exclude oesophageal injury. The Xray STN may reveal: free air in soft tissue neck and retropharyngeal or retrotacheal swelling. Chest X-ray may reveal free mediastinal or cervical air, mediastinal widening, pneumothorax or hydrothorax and in delayed cases pulmonary infilterates. Contrast oesophagogram with a water soluble contrast such as Gastrograffin is widely utilized to confirm the diagnosis, to localise the exact anatomical site of injury and any associated underlying oesophageal pathology such as stricture, malignancy, diverticulum, or a motility disorder.28 free perforation in the pleura or mediastinum is demonstrated by Gastrograffin. Patient should be alert and cooperative and should be able to swallow without aspiration as Gastrograffin has a potential to induce a severe chemical pneumonitis. Repeat studies may be required after 4-6 hours in case of a normal previous study as due to rapid passage of contrast medium while the patient is in upright position there can be false negative results. The study should be done in both right and left lateral decubitus positions. Once a gross leak is ruled out or in case of a negative study with Gastrograffi, a thin barium study is the next step to rule out small perforation. Barium should not be used as first choice for exacerbating mediastinal, pleural, or abdominal contamination should barium be leaked. Esophagography is limited by false negative rate of 10% to 38%, risk of aspiration as well as relative inability to assess mucosal detail [28,29].
More recently, computed tomography has proven an extremely useful diagnosing modality for assessing the various manifestations of oesophageal rupture. CECT chest may show free air or fluid or abscess in the mediastinum, pleural cavity, pericardium and peritoneum. The definitive finding of frank leakage of oral contrast is not always seen and should not be relied upon to prove or disprove the diagnosis [30,31]. Importantly, CT provides critical information regarding the extent and location of any extra-oesophageal fluid collection that may require operative intervention or percutaneous drainage. CECT is poor at localizing perforations.
Oesophagoscopy serves a critical role in assessment of the full spectrum of oesophageal pathology including perforations, perforation by retained foreign body, intra-operatively to localise the perforation in case it is not identified during exploration [32]. However, it is invasive and does not allow determination of the extent of extra-oesophageal contamination. Concen may also exist about the safety of flexible endoscopy, with its need for insufflations, in setting of acute perforation as it may increase the pneumo-mediastinum or cervical emphysema further aggravating the condition. However, the examination can be completed in experienced hands without any impact on the extent of injury keeping the insufflations at minimum level just necessary for adequate visualisation of the entire mucosa or using carbon dioxide for insufflations [33,34]. Consideration should be given to placement of chest tube prior to the procedure if concern concern exists about the potential to induce or exacerbate a pneumothorax. Small perforation may be subtle and rather than an obvious tear, only an echymotic and slightly disrupted mucosa that flutters with insufflations may be seen or perforation may get missed. As therapeutic maneuver endoscopy can be utilized for irrigation and suctioning of contained extraluminal fluid collections. Triple endoscopy (laryngoscopy, oesophagoscopy and bronchoscopy) is required in cases of peneterating, gunshot and missile injuries.
Tube thoracostomy for hydropneumothorax with demonstration of air leak not in synchrony with respiration may suggest oesophageal injury. Increased amylase levels in drainage fluid are highly suggestive of oesophageal leak.
Treatment Plan
Location and extent of perforation must be determined prior to any surgical intervention, in that the planning of incisions and the type of procedure performed will depend critically on the diagnostic findings [35].
Two fundamental principles of treatment are: (1) Eliminating the source of sepsis by repairing or otherwise controlling the leak, and (2) drainage of extra-oesophageal fluid collections. Initial treatment should be nil orally by mouth, administration of intravenous fluids, and initiation of broad spectrum antibiotics. Antibiotics should be directed towards a polymicrobial infection and in addition antifungal agents should be added in individuals with history of long-standing proton pump inhibitor use due to increased risk of fungal colonization in the stomach [36]. Goals of treatment are: to treat the infection, minimize or prevent further contamination, nutritional support and restoration of continuity of digestive tract [37]. Chest tube thoracostomy should be considered early to drain large pleural collections while preparations are made for definitive intervention.
Conservative/Non-operative management
In carefully selected patients non operative approach has been successful and it may avoid serious complications of major surgery in emergency [38]. The criteria selected by Cameron et al. and modified by Altorjay are: (1) minimal intraluminal dissection, (2) contained transmural perforation with drainage back into the oesophagus, (3) no associated distal obstruction, (4) perforation not into the abdominal cavity, (5) no evidence of sepsi, (6) oesophagus worth salvaging [39,40]. However, it is difficult to determine whether the leak will remain contained or will lead to mediastinitis or pleural contamination, respiratory distress and sepsis. In general, the perforations in the neck are better tolerated than those located in the thorax or abdomen. Close monitoring, nil per orally, antibiotic cover, proton pump inhibitors, hyperalimentation, appropriate pain management are the main aspects of conservative management. Percutaneous aspirations or surgical interventions may be considered as and when required for increasing collections. Non-operative treatment is also used in case of underlying inoperable malignant stricture.
Endoscopic management
Advances in endoscopic therapies have created new ways to manage oesophageal perforations and aims to restore continuity for early feeding, prevent ongoing contamination of the mediastinum, and facilitate re-epithelialisation of the mucosal defect by hemoclips, glue, sponges vacuum therapy and stents [41,42]. Endoscopic hemoclipping has been successful in 3-25 mm defects, less than 25% circumference defect with a median healing time of 18 days. A novel over-the-scope-clip has been developed for perforations upto 30 mm in diameter [43,44]. Large perforations can be successfully treated with stent placement if dehiscence is less than 70% circumference with overall success rate of 85% [45]. The availability of fully covered, self expanding, removable, plastic, metal, and hybrid stents have created new ways to manage oesophageal perforations e.g. FSEMS, PSEMS and SEPS (biodegradable) [46,47]. A stent should be selected to provide adequate coverage of the entire length of perforation, ideally with several centimetres of overlap both above and below the injury. Endoscopy with fluoroscopy is used to know the proximal and distal limit of perforation and stent is deployed over a guide wire placed till stomach under fluoroscopy for proper positioning. Repeat endoscopy is required to ensure adequate sealing of the perforation. Perforations not amenable to stenting are: high in the cervical oesophagus where a stent would extend into pharynx or cause significant discomfort, or those spanning the gastroesophageal junction that are difficult to occlude due to the bulbous nature of the gastric cardia and minimal distal overlap of the perforation, and the perforation more than six centimetre in length. Problems associated with stents are; stent migration (more common with covered stents), dysphagia. The stent needs to be removed if not biodegradable and the timing of stent removal is a matter of controversy because it is difficult to know when the perforation has healed and long time stent placement has risk of erosion into surrounding structures. The problems faced while stent retrieval are: bleeding, impaction, and stent fracture [48]. Stenting can be supplemented by percutaneous aspiration/intercostal drainage/open or laparoscopic or video assisted thoracoscopic drainage and debridement.
Operative management
Surgical options are: primary repair of oesophageal perforation, wide drainage, exclusion or diversion and oesophagectomy.
Primary Surgical Repair
In 1724, the Dutch physician Hermann Boerhaave published the first treatise on spontaneous oesophageal perforation, describing the demise of Baron de Wassenaer, the Grand Admiral of the Dutch fleet, after an episode of self-induced vomiting. In 1947, Barrett published the first report of a successfully repaired perforation of oesophagus and now the operative repair is the gold standard of care.8 One must move to open surgical repair in early diagnosed cases or even in cases with delayed presentation if the other therapeutic approaches are not available or proving futile. The various studies show the most favourable results in early diagnosed cases but identification of the rent may not be easy and in such situations instillation of methylene blue dye intraluminally with manual compression of the oesophagus or filling the operative field with saline and vigorously instilling air into the oesophagus may help to demonsterate the air leak or intra-operative endoscopy may be done. In primary suturing the repair should be in two layers and it should be buttressed with tissue flaps from sternocleidomastoid muscle, pleura, pericardium, diaphragm, lung, intercostals or external costal muscle, stomach wall or jejunum [49,50]. The deeper mucosal defects extend beyond the more superficial muscular one. The key principle for repair is: proximal and distal myotomy starting from the proximal and distal edges of the rent should be done to identify the edges of mucosa and to facilitate its complete closure. The mucosal edges should be debrided back to healthy non- inflamed tissue and reapproximated with sutures or by staplers over an oesophageal bougie to avoid narrowing by stapler. The muscular layer is then closed with interrupted sutures. Repair should be supplemented by appropriate cleaning and debridement with neck, mediastinal or pleural cavity drains, decompression by gastrostomy, diversion and feeding jejunostomy. Drain should not be directly abutting the suture line. Repair over T-tube is an alternative effective method in thoracic oesophagus repair allowing controlled oesophagus- cutaneous fistula and healing occur without contamination. P [51] T-tube can be removed after 4-6 weeks and oesophago-cutaneous fistula will eventually heal. When primary repair is attempted for rents proximal to stricture or achlasia, it should be supplemented with myotomy and defect should be covered with fundoplication. Recently if the facilities and expertise are available, laparoscopy or video assisted thoracic surgery may aid both in early and more efficient recognition of injuries, their repair along with drainage procedures [52,53].
Exclusion
Diversion of oesophageal secretions in very ill patients and in delayed presentation is intended to minimize the contamination and infection to expedite healing until the patient ’ s general condition stabilizes. Various exclusion techniques are; oesophagectomy with end oesophagostomy, placing absorbable suture/tape/staplers around the oesophagus above the cardia in order to prevent gastro oesophageal reflux that might interfere with the healing, T-tube or loop cevical oesophagostomy where an absorbable ligature is applied to the cervical oesophagus lumen distal to the oesophagostomy. The disadvantage of exclusion procedures are that these techniques require a second stage operation for reconstruction or removal of tape after healing, approach is complex, inconvenient for the patient and reported results of these procedures have not been uniformly satisfactory with a high morbidity and mortality.
Oesophagectomy
In cases of perforations associated with underlying oesophageal disease e.g. corrosive stricture, malignancy or extensive damage of oesophagus due to missile injury where oesophagus is not worth salvaging, transthoracic or transhiatal oesophagectomy and gastric pull up or colonic interposition should be contemplated. Transthoracic approach should be from the side of pleural collection for thorough debridement and decortications in case of empyema. In case of sepsis and hemodynamic instability only resection may be done deferring reconstruction for a later date. A long proximal oesophagus should be kept to aid in future reconstruction and also it can be easily brought out as oesophagostomy from upper chest rather than neck so that an appliance may be applied for collection of secretion.
To sum up the management strategies are: (1) conservative or non-operative treatment in small contained leaks without systemic sepsis and underlying oesophageal disease, (2) early/ delayed repair, reinforcement in larger defects along with drainage, (3) oesophageal exclusion procedures in critically ill patients with severe pleuro-mediastinal infection and necrosis, (4) irrigation and drainage of the contamination with gastric decompression leaving the oesophagus to heal spontaneously, (5) endotherapy supplemented with drainage procedures if the facilities are available. Absolute rules cannot be made about selection of non-operative or operative treatment. The different treatment modalities are not exclusive of each other but may be used altogether in the management of this condition. In most of the cases, single intervention or procedure is not sufficient and a hybrid or multidisciplinary approach is used in a timely manner to achieve good clinical outcome [54-56].
Summary
Early diagnosis is of utmost importance for effective management of oesophageal rupture. The radiological findings are subtle and may be missed, especially in non-endoscopic trauma and spontaneous perforations. The associated morbidity is incapacitating especially in late diagnosed cases resulting in high mortality. The overall treatment plan must be individualized, considering the availability of spectrum of non-operative, endoscopic and operative alternatives, since no single strategy has been recommended sufficient to deal with oesophageal perforation.
Conclusion
The diagnostic work up in oesophageal injuries should include repeated and extended examinations when there is strong clinical suspicion, even in patients who initially show negative imaging results. Treatment is a challenge, where one has to balance between operative and less invasive non-operative and endoscopic approaches.
REFERENCES
- Byard RW. Esophageal causes of sudden and unexpected death. J Forensic Sci. 2006; 51: 374-380.
- Amudhan A, Rajendran S, Raj VV. Management of esophageal perforation: experience from a tertiary center in India. Dig Surg. 2009; 26: 322-328.
- Chao YK, Liu YH, Ko PJ, Wu YC, Hsieh MJ, Liu HP, et al. Treatment of esophageal perforation in a referral center in Taiwan. Surg Today. 2005; 35: 828-832.
- Eroglu A, Turkyilmaz A, Aydin Y, Karaoglanoglu N. Current management of esophageal perforation: 20 years experience. Dis Esophagus. 2009; 22: 374-380.
- Bhatia P, Fortin D, Malthaner RA. Current concepts in the management of esophageal perforations: A twenty-seven year Canadian experience. Ann Thorac Surg. 2011; 92: 209-215.
- Brinster CJ, Singhal S, Lee L. Evolving options in the management ofoesophageal perforation. Ann Thorac Surg. 2004; 77(4): 1475-1483.
- Vidarsdottir H, Blondal S, Alfredsson H, Giersson A,Gudbjartsson T. Oesophageal perforation in Iceland: A whole population study on incidence aetiology and surgical outcome. Thorac Cardiovasc Surg. 2010; 58: 476-480.
- Barret NR. Report of a case of spontaneous perforation of the oesophagus successfully treated by operation. Br J Surg. 1947; 35: 216-218.
- Sepesi B, Raymond DP, Peters JH. Esophageal perforation: Surgical, endoscopic and medical management strategies. Curr Opin Gastroentrol. 2010; 26(4): 379-383.
- Ryom P, Ravn JB, Penninga L, Schmidt S, Iverson MG, Skov-Olsen P, et al. Aetiologytreatment and mortality after oesophageal perforationin Denmark. Dan Med Bull. 2011; 58: A4267.
- Jones 2nd WG, Ginsberg RJ. Esophageal perforation: A continuing challenge. Ann Thorac Surg. 1992; 53: 534-543.
- Abbott OA, Mansour KA, Logan WD. Atraumatic so called “spontaneous” rupture of the oesophagus: a review of 47 personal cases with comments on a new method of surgical therapy. J Thorac Cardiovasc Surg. 1970; 59: 67.
- Quine MA, Bell GD, McCloy RF, Matthews Hr. Prospective audit of perforation rates following upper gastrointestinal endoscopy in two regions of England. Br J Surg. 1995; 82: 530-533.
- Merchea A, Cullinane Dc, Sawyer MD, Iqbal CW, Baron TH, Wigle D, et al. Esophagogastroduodenoscopy-associated gastrointestinal perforations: A single-center experience. Surg. 2010; 148: 876-880.
- Gander JW, Berdon WE, Cowles RA. Iatergenic esophageal perforation in children. Pediatr Surg Int. 2009; 25: 395-401.
- Sanchez-Pernaute A, Aguirre EP, Talavera P, Valladres LD, de la Serna JP, Mantilla CS, et al. Laparoscopic approach to esophageal perforation secondary to pneumatic dilation for achlasia. Surg Endosc. 2009; 23: 1106-1109.
- Kau RL, Kim N, Hinni ML, Patel NP. Repair of esophageal perforation due to anterior spine instrumentation. Laryngoscope. 2010; 120: 739-742.
- Ozwr MT, Demirbas S, Harlak a, Ersoz N, Eryilmaz M, Cetiner S. A rare complication after thyroidectomy: Perforation of oesophagus: A case repot. Acta Chir Belg. 2009; 109: 527-530.
- Derbes VJ, Mitchell RE. Hermann Boerhaave’s (1) Atrocis, nec Descripti prius, Morbi Historia (2). the first translation of the classic case report of rupture of the esophagus, with annotations. Bull Med LIbr Assc. 1995; 43: 217.
- Riffat F, Cheng A. Pediatric caustic ingestion: 50 consecutive cases and a review of the literature. Dis Esophagus. 2009; 22: 89-94.
- Cheng HT, Cheng CL, Lin CH, Tang JH, Chu YY, Liu Nj, et al. Caustic ingestion in adults: The role of endoscopic classification in predicting outcome. BMC Gastroenterol. 2008; 8: 31-10.
- Roan JN, Wu MH. Esophageal perforation caused by external air-blast injury. J Cardiothorac Surg. 2010; 5: 130-140.
- Strauss DC, Tandon R, Mason RC. Distal thoracic oesophageal perforation secondary to blunt trauma: Case report. World J Emerg Surg. 2007; 2: 8-10.
- Beal I, Pottmeyer EW, Spisso JM. Esophageal perforation following external blunt trauma. J Trauma. 1998; 28: 1425.
- Shama DM, Odell J. Peneterating neck trauma with tracheal and oesophageal injuries. Br J Surg. 1984; 71: 534.
- Mackler SA. Spontaneous rupture of the esophagus; an experimental and clinical study. Surg Gynecol Obstet. 1952; 95: 345-356.
- Enguidanos L, Pfleiderer A, Smith W, Ramkumar S. Pneumomediastinum secondary to an apparently trivial stab wound to the neck: The value of Hamman’s sign and thorough radiological investigation. Emerg Med. J 2005; 22: 230-231.
- Swanson JO, Levine MS, Redfwrn RO. Usefulness of high density barium for detection of leaks after oesophagogastrectomy, total gastrectomy and total laryngectomy. AJR Am J Roentgenol. 2003; 181(2): 415-420.
- Soreide JA, Viste A. Esophageal perforation: diagnostic work-up and clinical decision-making in the first 24 hours. Scand J Trauma Resusc Emerg Med. 2011; 19: 66.
- White CS, Templeton PA, Attar S. Esophageal CT findings. AJR Am J Roengenol. 1993; 160(4): 767-770.
- Fadoo F, Ruiz DE, Dawn SK. Helical CT oesophagography for the evaluation of suspected oesophageal perforation or rupture. AJR Am J Roentgenol. 2004; 182(5): 1177-1178.
- Arantes V, Campolina C, Valerio SH, de Sa RN, Toledo C, Ferrari TA, et al. Flexible esophagoscopy as a diagnostic tool for traumatic esophageal injuries. J Trauma. 2009; 66: 1677-1682.
- Maeda Y, Hirasawa D, Fujita N, Obana T, Suagawara T, Ohira T. A pilot study to assess mediastinal emphysema after esophageal endoscopic submucosal dissection with carbon dioxide insufflations. Endoscopy. 2012; 44: 565-571.
- Uemura M, Ishii N, Itoh T, Suzuki K, Fujita Y. Effects of carbon dioxide insufflations in esophageal endoscopic submucosal dissection. Hepatogastroentrology. 2012; 59: 734-737.
- Attar S, Hankins JR, Sutter CM. Esophageal perforation: A therapeutic challenge. Ann Thorac Surg. 1990; 50: 45.
- Elsayed H, Shaker H, Whittle I. The impact of systemic fungal infection in patients with perforated oesophagus. Ann R Coll Surg Engl. 2012; 94: 579-584.
- Bufkin BL, Miller Jr JI, Mansour KA. Esophageal perforation: Emphasis on management. Ann Thorac Surg. 1996; 61: 1447-1451.
- Abbas G, Schuchert MJ, Pettiford BL, Pennathur A, Landreneau J. Contemporaneous management of oesophageal perforation. Surg. 2009; 146: 749-755.
- Cameron JL, Kiffer RF, Hendrix TR. Selective nonoperative management of contained intrathoracic disruptions. Ann Thorac Surg. 1997; 27: 404-408.
- Altorjay A, Kiss J, Voros A. Nonoperative management of oesophageal perforations. Is it justified? Ann Surg. 1997; 225: 415-421.
- Raju GS. Endoscopic management of gastrointestinal leaks. Gastrointest Endosc Clin N Am. 2007; 17: 487-503.
- Qadeer MA. Dumot JA, Vargo JJ, Lopez AR, Rice TW. Endoscopic clips for closing esophageal perforations: Case report and pooled analysis. Gastrointest Endosc. 2007; 66: 605-611.
- Gubler C, Bauerfeind O. Endoscopic closure of iaterogenic gastrointestinaltract perforations with the over-the-scope clip. Digestion. 2012; 85: 302-307.
- Kirschnaik A, Subotova N, Zieker D, Konigsrainer A, Kratt T. The Over-The-Scope-Clip (OTSC) for the treatment of gastrointestinal bleeding, perforations, and fistulas. Surg Endosc. 2011; 25: 2901-2905.
- Schubert D, Scheidbach H, Kuhn R,Wex C, Weiss G, Eder F. Endoscopic treatment of thoracic esophageal anastomotic leaks by using silicone-covered, self-expanding polyester stents. Gastrointest Endosc. 2005; 61: 891-896.
- Swinnen J, Eisendrath P, Rigaux J, Kahegeshe I, Lemmers A, Le MoineO. Self-expandable metal stents for the treatment of benign upper GI leaks and perforations. Gastrointest Endosc. 2011; 73: 890-899.
- Cerna M, Kocher M, Valek V, Aujesky R, Neoral C, Andrasina T. Covered biodegradable stent: New therapeutic option for the management of esophageal perforation or anastomotic leak. Cardiovasc Intervent Radiol. 2011; 34: 1267-1271.
- van Heel NC, Haringsma J, Spaander MC, Bruno MJ, Kuipers EJ. Short term esophageal stenting in the management of benign perforations. Am J Gastroentrol. 2010; 105: 1515-1520.
- Wright CD. Primary repair for delayed recognition of oesophageal perforation. In: Ferguson MK, ed. Difficult Decision in Thoracic Surgery: An Evidence-based Approach. London: Springer. 2007: 298-304.
- Luo B, Huang J, Tao H, Li M, Pan X, Li M, et al. Successful repair of delayed esophageal perforation with sternocleidomastoid muscle flap after anterior cervical spinal surgery. Int J Exp Med. 2016; 9: 9143-9151.
- Nakabayashi T, Kudo M, Hirasawa T, Kuwano H. Successful late management of esophageal perforation with T-tube drainage. Case Rep Gastroentrol. 2008; 2: 67-70.
- Landen S, EI Nakadi I. Minimally invasive approach to Boerhaave syndrome: A pilot study of three cases. Surg Endosc. 2002; 16: 1354-1357.
- Toelen C, Hendrickx I, Van Hee R. Laparoscopic treatment of Boerhaave’s syndrome: A case report and review of the literature. Acta Chir Beig. 2007; 107: 402-404.
- Schenfine J, Griffin SM. Oesophageal emergencies. Oesophageogastric surgery: A companion to specialist surgical practice. Edited by: Griffin SM, Raimes SA, Philadelphia: Elsevier Saunders 2006; 365-393.
- Ronald V, Romero, Khean-Lee Goh. Esophageal perforation: Continuing challenge to treatment. Gastrointest Interv. 2013; 2:1-6.
- Kuppusamy MK. Evolving management strategies in esophageal perforation: Surgeons using nonoperative techniques to improve outcomes. J Am Coll Surg. 2011; 213:164-171.
Citation: Dalal RU, Dalal KA, Kaur R, Anand L, Dua A (2020) Oesophageal Perforation Management in a Tertiary Care Hospital. J Surg Anesth. 10.35248/2684-1606.20.4.127
Copyright: �?�©2020 Dalal RU, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.