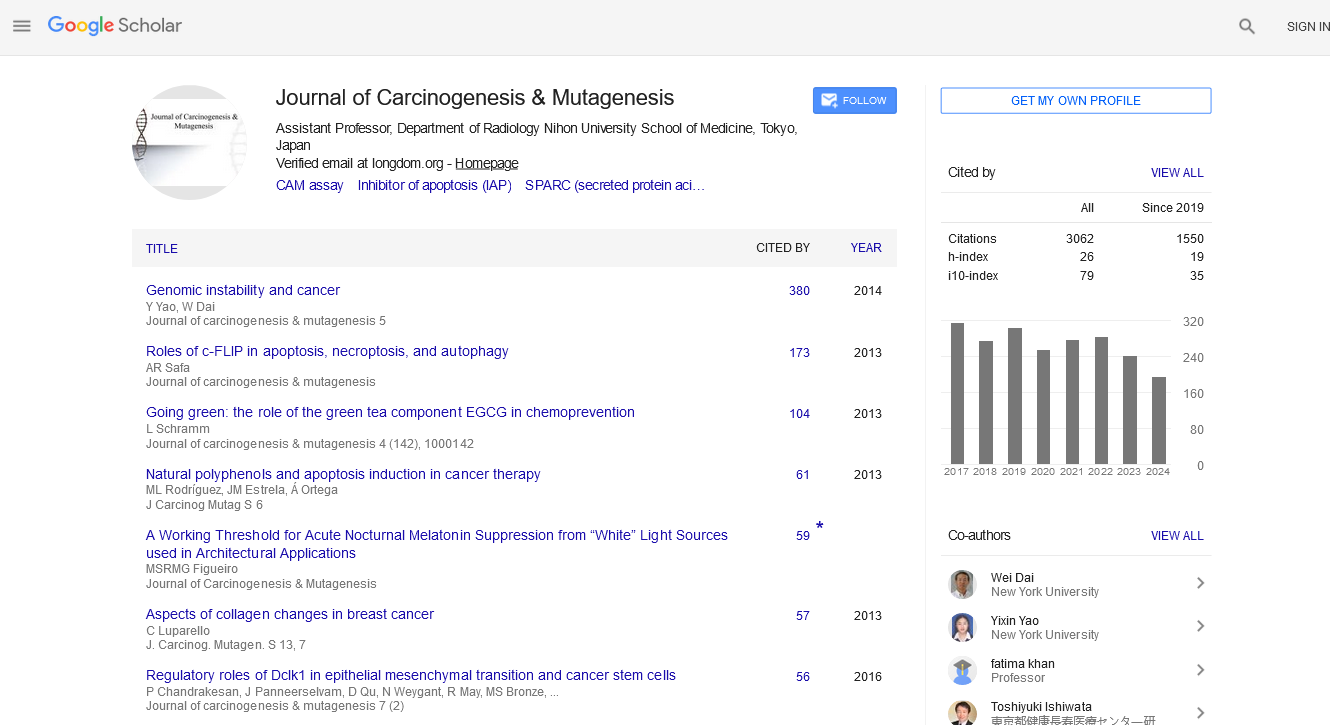
PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2021) Volume 0, Issue 0
Minimally Invasive Distal Pancreatectomy for the Management of Left-Sided Pancreatic Cancer
Yasunari Kawabata*, Takeshi Nishi and Yoshitsugu TajimaReceived: 12-Apr-2021 Published: 03-May-2021, DOI: 10.35248/2157-2518.21.s17.003
Abstract
Curative surgical resection is considered the most effective treatment option to achieve long–term survival in patients with pancreatic cancer. In performing a Distal Pancreatectomy (DP) for left–sided pancreatic cancer, there are two main approaches to dissection: proceeding from left to right and from right to left. The conventional DP procedure was the Standard Retrograde Pancreatosplenectomy (SRPS), with a left–to–right dissection, and then the radical antegrade Modular Pancreatosplenectomy (RAMPS), with a right–to–left dissection, was developed. A greater number of harvested lymph nodes and an increase in R0 resection have been achieved in RAMPS as compared to SRPS; however, oncological outcomes, including patient survival, are comparable in these procedures. Recently, Minimally Invasive Distal Pancreatectomy (MIDP) using laparoscopy for pancreatic cancer has been advanced. The MIDP also has not been enough to show oncological benefits as compared with an open DP. Additional randomized controlled trials should be conducted to clarify the impacts and benefits of each surgical approach in performing DP for cancer of the body or tail of the pancreas
Keywords
p> Distal pancreatectomy; Left–to–right dissection; Right–to–left dissection; Minimally invasive surgery; Left–sided pancreatic cancerIntroduction
Pancreatic cancer is the fifth most common cause of cancer death, and the annual death toll has reached 34,900 in Japan. The vast majority of pancreatic cancer patients are diagnosed with locally advanced or unresectable disease, and most patients experience relapse after treatment [1]. Although a treatment strategy including diagnostics and adjuvant therapies has been advanced in recent decades, surgical resection still remains the gold-standard treatment option to achieve long–term survival in patients with pancreatic cancer. In performing a Distal Pancreatectomy (DP) for left–sided pancreatic cancer, there are two main approaches to dissection: proceeding from left to right and from right to left [2,3]. Furthermore, Minimally Invasive Distal Pancreatectomy (MIDP) utilizing laparoscopic or robotic techniques has advanced dramatically and has become more prevalent in recent years. The first Laparoscopic DP (LDP) was reported by Cuschieri, and MIDP including LDP has become a safe and effective surgical option for pancreatic disorders, including malignant tumors [4].
Recent Randomized Controlled Trials (RCTs), meta–analyses, and systematic reviews have revealed that short–term outcomes after DP, such as intraoperative blood loss and hospital stay, were significantly improved with MIDP as compared to open DP [5-8]. However, there is no evidence to prove oncological superiority among pancreatic dissection techniques or surgical approaches, including MIDP and open DP, in the management of left–sided pancreatic cancer.
Left-to-Right and Right-to-Left Dissection Procedures in DP for the Management of Cancer of the Body or Tail of the Pancreas
Pancreatosplenectomy is the standard surgical procedure for cancer of the body or tail of the pancreas. This procedure, which involves an en bloc mobilization of the spleen and pancreas in a left–to–right dissection, was initially performed by Trendelenburg and then established by Mayo in 1913 as the so– called Standard Retrograde Pancreatosplenectomy (SRPS) [2,9]. To achieve more complete tumor clearance with negative posterior surgical margins and radical lymphadenectomy around the body and tail of the pancreas, Strasberg demonstrated a modified SRPS for left–sided pancreatic cancer in 2003, namely, Radical Antegrade Modular Pancreatosplenectomy (RAMPS) [3]. The surgical concepts of RAMPS are as follows: (1) right–to–left dissection to control the major vessels initially, (2) modular setting of the dissection plane behind the body and tail of the pancreas to obtain negative posterior margins, and (3) complete lymph node clearance around the body and tail of the pancreas [3,10]. RAMPS achieved a high R0 resection rate of 82%–89.3% in open surgery for advanced pancreatic cancer [10,11]. Moreover, systematic reviews and meta–analyses comparing RAMPS and SRPS for left–sided pancreatic cancer revealed that the number of lymph nodes harvested and the R0 resection rate were significantly greater in RAMPS than in SRPS, without an increase in intraoperative blood loss or postoperative complications [12-15].
However, there were no significant differences between the two surgical techniques with regard to recurrence rates, disease–free survival, and overall survival [12-15]. In addition, laparoscopic and robotic RAMPS showed no superiority in terms of the number of lymph nodes harvested, the R0 resection rate, intraoperative blood loss, and postoperative complications as compared to open SRPS in well–selected left–sided pancreatic cancer using matched–pair analysis [16]. No RCT has been published as of the time of our research comparing left–to–right and right–to–left dissection techniques in the management of cancer of the body or tail of the pancreas both in the minimally invasive and open methods.
Oncological Outcomes in MIDP
MIDP is strongly recommended over open DP in treating benign or low–grade malignant tumors because of lower blood loss during surgery, equivalent complication rates, and a shorter hospital stay [6-8,17]. However, previous systematic reviews and meta–analyses showed comparable oncological outcomes with regard to cancer–free resection margin, disease–free survival, and overall survival between MIDP and open DP in patients with left–sided pancreatic cancer [5,8,13-15,17].
Furthermore, a large international retrospective cohort study of DP for left–sided pancreatic cancer identified Gerota’s fascia resection, R0 resection, and a decreased lymph node ratio to be significant prognostic predictors for overall survival after DP in patients with left–sided pancreatic cancer, whereas MIDP did not show improved patient survival as compared with open DP [18]. At present, MIDP seems to be a feasible, safe, and oncologically equivalent technique when managing well–selected patients with left–sided pancreatic cancer at high–volume centers with experienced surgeons [17,19]. To clarify the oncological benefits of MIDP, properly conducted RCTs will provide a further evidence of the benefits of MIDP for the management of left–sided pancreatic cancer.
Conclusion
Both MIDP and open DP play an important role in the management of pancreatic disorders, including benign and malignant tumors. Future studies including RCTs should be conducted to clarify the impacts and benefits of each surgical approach in performing DP for cancer of the body or tail of the pancreas
REFERENCES
- Tempero MA. NCCN Guidelines Updates: Pancreatic Cancer. J Natl Compr Canc Netw. 2019;17(1):603-605.
- Mayo WJ. I. The surgery of the pancreas: I. Injuries to the pancreas in the course of operations on the stomach. II. Injuries to the pancreas in the course of operations on the spleen. III. Resection of half the pancreas for tumor. Ann Surg. 1913;58(2):145-150.
- Strasberg SM, Drebin JA, Linehan D. Radical antegrade modular pancreatosplenectomy. Surgery. 2003;133(5):521-527.
- Cuschieri A. Laparoscopic surgery of pancreas. JR Coll Surg Edinb. 1944;39(3):178-184.
- Riviere D, Gurusamy KS, Kooby DA, Vollmer CM, Besselink MGH, Davidson BR, et al. Laparoscopic versus open distal pancreatectomy for pancreatic cancer. Cochrane Databases Syst Rev. 2016;4(4):1-49.
- Klompmaker S, Thijs DR, Koerkamp BG, Shankar AH, Siebert U, Besselink MG, et al. Dutch pancreatic cancer group. International validation of reduced major morbidity after minimally invasive distal pancreatectomy compared with open pancreatectomy. Ann Sur. 2019;270(4):1-10.
- Rooij DT, van Hilst J, van Santvoort H, Djamila B, Peter VDM, Freek D, et al. Minimally invasive versus open distal pancreatectomy (LEOPARD):a multicenter patient-blinded randomized controlled trial. Ann Surg. 2019;269(1):2-9.
- Van Hilst J, de Rooij T, Klompmaker S, Majd R, Francesca A, Bilal AS, et al. Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a pan-European propensity score matched study. Ann Surg. 2019;269(1):10-17.
- Witzel O. Aus der Klinik des Herrn Prof. Trendelenburg. Beitrage zur Chirurgie der Bauchorgane. Dtsch Zeitschr Chir. 1886;24(2):326-354.
- Mitchem JB, Hamilton N, Gao F, Hawkins WG, Linehan DC, Strasberg SM, et al. Long-term results of resection of adenocarcinoma of the body and tail of the pancreas using radical antegrade modular pancreatosplenectomy procedure. J Am Coll Surg. 2012;214(1):e46-e52.
- Kawabata Y, Hayashi H, Takai K, Kidani A, Tajima Y. Superior mesenteric artery-first approach in radical antegrade modular pancreatosplenectomy for borderline resectable pancreatic cancer: a technique to obtain negative tangential margins. J Am Coll Surg. 2015;220(1):e49-e54.
- Abe T, Ohuchida K, Miyasaka Y, Ohtsuka T, Oda Y, Nakamura M. Comparison of surgical outcomes between radical antegrade modular pancreatosplenectomy (RAMPS) and standard retrograde pancreatosplenectomy (SPRS) for left-sided pancreatic cancer. World J Surg. 2016; 40(9):2267-2275.
- Cao F, Li J, Li A, Li F. Radical antegrade modular pancreatosplenectomy versus standard procedure in the treatment of left-sided pancreatic cancer: a systemic review and meta-analysis. BMC Surgery. 2017;17(3):67.
- Chun YS. Role of radical antegrade modular pancreatosplenectomy (RAMPS) and pancreatic cancer. Ann Surg Oncol. 2018;25(1):46-50.
- Zhou Q, Gao F, Gong J, Xie Q, Liu Y, Wang Q, Lei Z. Assessment of postoperative long-term survival quality and complications associated with radical antegrade modular pancreatosplenectomy and distal pancreatectomy: a meta-analysis and systematic review. BMC Surgery. 2019;19(1):12.
- Lee SH, Kang CM, Hwang HK, Choi SH, Lee WJ, Chi HS. Minimally invasive RAMPS in well-selected left-side pancreatic cancer within Yonsei criteria: long-term (>median 3 years) oncologic outcomes. Surg Endosc. 2014;28(3):2848-2855.
- Asbun HJ, Moekotte AL, Vissers FL, Filipe K, Federica C, Adnan A, et al. The Miami international evidence-based guidelines on minimally invasive pancreas resection. Ann Surg. 2020;271(1):1-14.
- Korrel M, Lof S, van Hilst J, Alseidi A, Boggi U, Busch OR, et al. Predictors for survival in an international cohort of patients undergoing distal pancreatectomy for pancreatic ductal adenocarcinoma. Ann Surg Oncol, 2021;28(2):1079-1087.
- Kawabata Y, Hayashi H, Kaji S, Fujii Y, Nishi T, Tajima Y. Laparoscopic versus open radical antegrade modular pancreatosplenectomy with artery-first approach in pancreatic cancer. Langenbecks Arch Surg. 2020;405(6):647-656.
Citation: Kawabata Y, Nishi T, Tajima Y (2021) Minimally Invasive Distal Pancreatectomy for the Management of Left-Sided Pancreatic Cancer. J Carcinog Mutagen. S17:003.
Copyright: © 2021 Kawabata Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.