Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- SWB online catalog
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
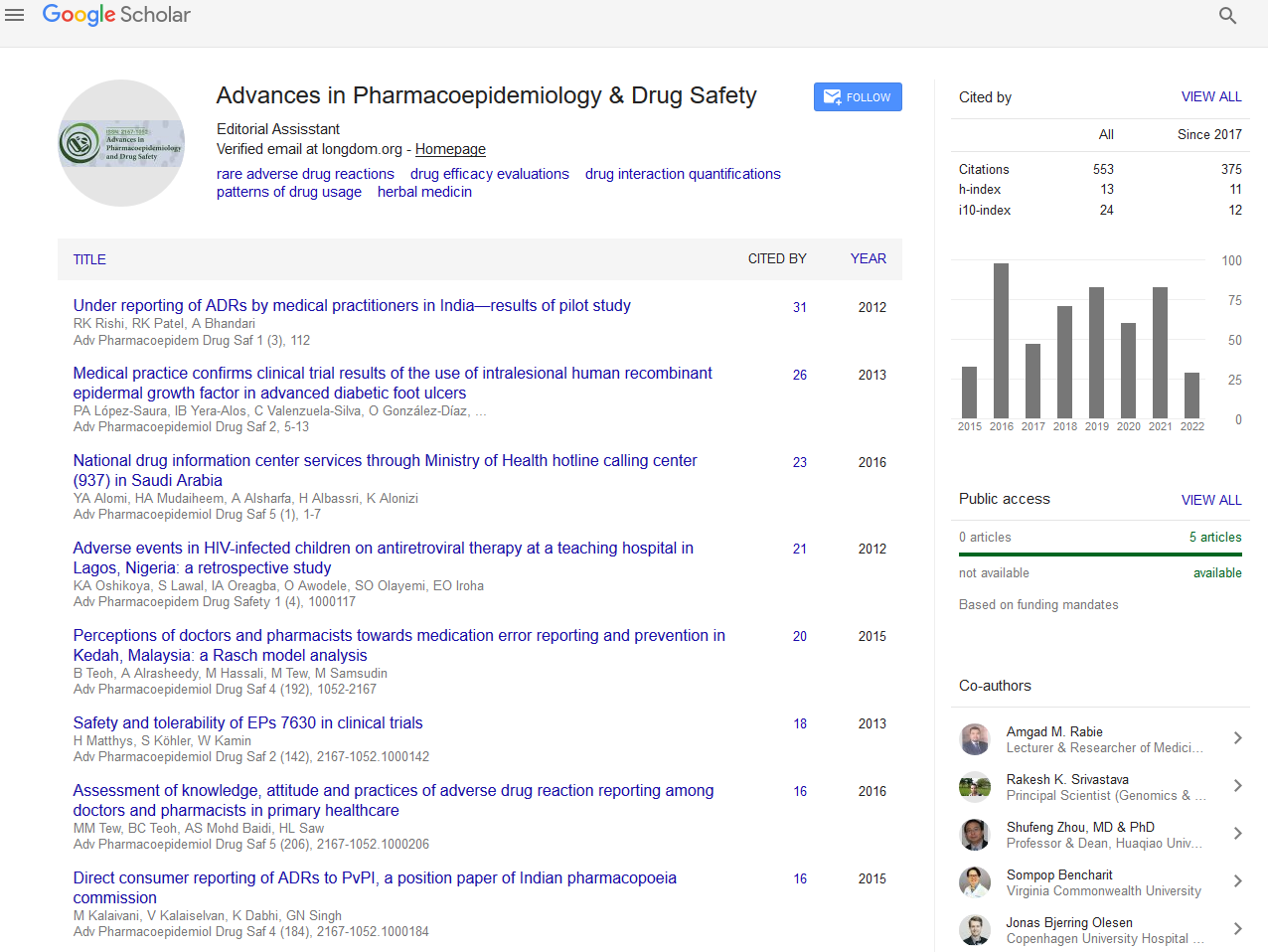
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2021) Volume 10, Issue 4
Local Drug Delivery in Periodontal Therapy: A Contemporary Review
Deepa G. Kamath* and Razia HaidrusReceived: 20-May-2021 Published: 10-Jun-2021, DOI: 10.35248/2167-1052.21.10.246
Abstract
Background: Periodontal disease is characterized by inflammation of supporting tissues of the teeth, resulting in progressive attachment loss, bone loss and subsequent tooth loss. Both non-surgical and surgical therapy can be used for the management of periodontal diseases. Systemic and local drug delivery of antimicrobials can be used as an adjunct to non-surgical therapy. Objective: The aim of this review article is to provide a better understanding regarding various local drug delivery agents used in periodontal therapy and their advantage over systemic delivery of antimicrobials. Conclusion: Placement of Local drug delivery restricts the drug within the periodontal pocket itself wherein they attain a much-elevated concentration. This review article includes various advances in local drug delivery systems. Most of the research is aimed at the use of LDD as either monotherapy or in combination with SRP. Further studies are required to determine the long-term benefit of these devices.
Introduction
Periodontal disease is characterized by inflammation of supporting tissues of the teeth, resulting in progressive attachment loss, bone loss and subsequent tooth loss [1]. Both non-surgical and surgical therapy can be used for the management of periodontal diseases. However, solely mechanical therapy may sometimes be ineffective, especially in areas inaccessible to periodontal instrumentation (deep pockets, furcation areas) or in cases of refractory and recurrent periodontitis patients [2]. In such situations, systemic and local drug delivery of antimicrobials can be used with NSPT (nonsurgical periodontal therapy) as an adjunct [3]. However, use of systemic antimicrobials has various disadvantages like: toxicity, development of bacterial resistance, limited patient compliance and drug interaction (Table 1).
| Local | Systemic | |
|---|---|---|
| Route of administration | Site specific | Oral/ Parenteral |
| Drug dosage | Low (in μg) | High (in mg) |
| Pain /discomfort | nil | Not painful |
| Pharmacokinetics | Minimal body distribution to different compartments with maximum concentration at delivered site. | Distribution to different compartments where antimicrobial effect may not be required |
| Peak levels | Within few minutes in GCF | Few hours in plasma |
| Superinfection | Limited | Present |
| Frequency | Usually once a week | Once in 6-12 hours |
| Patient compliance | Patient delivered - compliance required | Required for better efficacy |
| Professional delivered - not required. |
Table 1: Comparison of systemic and locally delivered antimicrobials.
A study conducted in 2012 concluded that use of 2% minocycline did not have added benefit over SRP in the management of chronic periodontitis. However, a study conducted in 2015 concluded that Arestin delivered in biodegradable system are a safe and efficient adjunct to SRP and can produce significant clinical benefits when compared to SRP
Therefore, to overthrow these limitations, local delivery of antimicrobial agents came into picture. Dr. Max Goodson in 1979 introduced the idea of controlled release Local Drug Delivery (LDD) which escapes the limitations related to systemic therapy by restricting the drug within the periodontal pocket itself wherein they attain a much-elevated concentration [4]. And since we know that periodontal diseases are localized to direct environment of periodontal pocket, thus it’s the most appropriate site for placement of local drug delivery agents. This forms the foundation for the application of local drug delivery devices in the management of periodontal diseases.
Historical Perspective
Early treatment modalities for severe form of periodontitis included single drug therapies with Tetracycline, Metronidazole, Penicillin or Clindamycin. Problems related to the use of systemic antibiotics like gastrointestinal disorders, allergies, toxicity, drug interaction, bacterial resistance, limited patient compliance etc were a concern [5].
Presently only 5 products are FDA approved and commercially available which include tetracycline fibers (ACTISITE), minocycline ointment (ARESTIN), metronidazole gel (ELYSOL), doxycycline hyclate in a resorbable polymer (ATRIDOX) and chlorhexidine chip (PERIOCHIP).
Principle
Oral administration of antibiotics has various adverse effects like inadequate drug concentration in they periodontal pocket, problems related to patient compliance, rapid fall in concentration to sub therapeutic level demanding repeated drug placement and development of bacterial resistance. Periodontal pocket bathed by GCF (Gingival Crevicular Fluid) offers an accessible natural reservoir for placement of LDD device. Local drug delivery provides a leeching medium for the release of a drug from solid dosage form and for its distribution throughout the pocket.The objective of using an intra pocket device is to obtain and maintain therapeutic levels of drug for required period of time that causes inhibition or killing of microorganism without any harm to the tissues. Controlled delivery systems are released slowly for sustained drug action and prolonged drug availability. Thus, periodontal pocket is the most appropriate site for placement of LDD and is considered the best modality. [6]
Indications
• Patients with recurrent/refractory periodontitis.
• Patients under supportive periodontal therapy/maintenance therapy.
• As an adjunct to SRP.
• Isolated periodontal pocket of 5 mm after successful phase I therapy.
• Medically compromised patients who either cannot undergo surgical therapy or who refuse to surgical periodontal therapy.
• During regenerative periodontal surgical procedures.
• Since sustained release devices are less invasive and less time consuming when compared to surgical treatment, LDD can be advantageous in patients with moderate periodontitis to restrict the extent of degree of surgical intervention required in the future.
Advantages
• When compared to systemic drug regimen, LDD attains 100- fold higher concentrations in subgingival site.
• Employs antimicrobial agents not suitable for systemic administration, such as various broad-spectrum antiseptic solutions.
• Better compliance.
• Decreases the risk of development of drug resistant microbial populations at non-oral body sites.
• Less invasive when compared to surgical intervention.
Disadvantages
• Difficulty in placement (deeper periodontal pockets/furcation areas).
• Time consuming and labour intensive.
• Use of LDD into periodontal pocket does not significantly affect the periodontal pathogens harbouring in the adjacent oral structures like tonsils, tongue etc. Hence, there is increased risk of recurrence of the disease.
• Relatively expensive.
Devices used as Local Drug Delivery
Fibers
These are threadlike, reservoir-type drug delivery systems that can be inserted and positioned in place by cyanoacrylate adhesive, thereby providing sustained release of tetracycline within the pocket. Goodson and co-workers developed tetracycline hydrochloride fibers [7]. Single application of these fibres resulted in significant reduction in spirochetes population. However, since the fibres were hollow it resulted in rapid draining of the drug. Therefore, to overthrow this limitation, matrix type of fibres was introduced to obtain tetracycline loaded ethyl vinyl acetate fibres, commercially available as Actisite. However, these were non-bioabsorbable, so once exhausted they required replacement with new ones. Other polymers used so far contain nylon, chitosan, polycaprolactone, collagen and alginate. Use of tetracycline fibres had an advantage of improving clinical parameters but were associated with a number of disadvantages like placement was time consuming, associated patient discomfort, was associated with redness and dislodgement of the fibers. Hence its use proved to be problematic for both clinician and the patient.
Films
Films are one of the most commonly used local drug delivery devices available and are prepared either by direct milling or solvent casting. They consist of drugs dispersed throughout the polymer and the ones made of non-degradable/water insoluble polymers are released by simple diffusion only while the films made of biodegradable/soluble polymers are released either by diffusion/matrix dissolution or erosion. Films can be sectioned into desired dimension and positioned into the periodontal pocket. Use of films has several advantages like: Easy insertion, customizability and less discomfort to the patient [8]. Films with sufficient tackiness and a width of <400 mm cannot be easily dislodged during routine oral hygiene procedures performed by the patient. Ethyl cellulose films integrating various drugs like metronidazole, tetracycline, chlorhexidine diacetate and minocycline have been developed.
Gels
Gels are semisolid system that are used for targeted delivery of antibiotics. They possess various advantages like: easy preparation and administration, faster drug release rate, biocompatible and bio-adhesive nature, therefore they stick to the periodontal pocket, also they have a minimum risk of irritation/allergic host reactions on the site of application since they can be quickly eliminated though catabolic pathway.
Gels can be either oleogels or hydrogels. Hydrogels comprise of 3 dimensional cross-linked structures of ionic interaction and hydrogen bonding and can be either macroporous, microporous or nonporous with a pore size of 0.1-1 mm and 100-1000 A˚ respectively with a potential to absorb water (10-20 times than their molecular weight) and therefore causing them to swell-up [9].
Strips and Compacts
A strip is a thin and elongated matrix band comprising of an elastic polymer with drugs dispersed throughout the polymer and it occupies a wide range of interproximal area. Strips are fabricated either by pressure melt method or solvent casting.
Acrylic strips made of single or a combination of drugs has been used by researchers in the past which bought remarkable improvement in clinical parameters by effective elimination of microbes from periodontal pocket. However, strips have their own limitation. Since the strips are non-biodegradable, they require removal after therapy, which may interfere with regeneration of the tissues at the placement site.
Vesicular systems
Liposomes are similar to biomembranes in structure and behaviour; therefore, they are exclusively used in periodontal diseases. Liposomes are microscopic lipid-based vesicles and can be either uni/multi lamellar. They are manufactured using long chain fatty acids, non toxic surfactants, cholesterol, membrane proteins, sphingolipids and glucolipids Liposomes are formed by self-assembling phospholipids in aqueous medium and can vary in size, charge, composition, lamellarity, lipids and method of preparation. Size of vesicles range between 0.1-0.5 mm for multilamellar, 0.02-0.05 mm for small unilamellar and >0.06 mm for large unilamellar respectively. They have various advantages like: biocompatibility, biodegradability, nonimmunogenic, non-toxic, good stability and ability to protect the drug from external environment. Nonetheless they have various disadvantages: leakage of the encapsulated drugs, high production cost and shorter half-life.
Microparticle system
Microspheres are solid spherical structures containing drugs dispersed in polymeric matrix. They offer controlled and sustained drug release at the site of insertion. They can be either biodegradable or non-biodegradable and can be either obtained from natural or synthetic source. They can be used to dental paste chip, or can be injected directly into the periodontal pocket. Microparticles have various advantages which include improved patient compliance, decreased intensity and frequency of adverse effects, guarding of unstable drug before and after administration, sustained therapeutic effect, and enhanced bioavailability and controlled drug release.
Nanoparticle system
Drug release of micro particle-based hydrogels used in dentistry is affected by their structure. Nanoparticles are more advantageous than emulsion-based delivery systems microparticles and microspheres. They have a size range from 10-1000 nm. The drug is attached, encapsulated, entrapped or dissolved to a nanoparticle matrix. They are very dispersible in aqueous medium, offer controlled release rate and enhanced stability.
Since they have a small size, they can reach sites that cannot be reached by other devices. An equal drug distribution for extended period of time is achieved with nanoparticles with an additional advantage of decreasing the dosage frequency.
Nano fibers
Nanofiber technology is a new and developing field. Polymeric fibres have a size range of nanometre or submicron order and are referred to as nanofibers [10]. They provide numerous remarkable physical properties like better strength and a larger surface area to volume ratio. Preparation of nanofibers is carried out by various methods and electro spinning is the most accepted method for their manufacture.
Various Agents Used As Local Drug Delivery
Tetracycline
The first extensively studied LDD product in U.S. was ACTISITE tetracycline fibre. These are cylindrical nonresorbable devices of 0.5 mm diameter made of a biologically inert vinyl acetate/ethylene copolymer comprising of tetracycline 12.7 mg/9 inches. The fiber is removed from the pocket after 7-10 days. It obtains a concentration of 1,300 μg/ml in the pocket wall which is superior to the concentration required for inhibition of growth of periodontal pathogens [11]. Metaanalysis published in 2003 reported a significant mean reduction in Probing Depth (PD) in favour of local tetracycline therapy and suggested more advantage with fibres compared to other devices. A meta-analysis conducted in 2016 concluded that there was a significant improvement in periodontal parameters such as CAL, PD, and sulcular bleeding index in favour of tetracycline as local drug delivery compared to placebo.
Minocycline
Minocycline is available as biodegradable gel, biodegradable mix in syringe and as ointment. Semisynthetic tetracycline was first introduced in 1967. Film, microspheres, and ointment has been tried for local delivery of minocycline [12]. Minocycline is an antibiotic with bacteriostatic properties; however, no data are available regarding the extent of its subgingival drug reservoir.
A study conducted in 2012 concluded that use of 2% minocycline did not have added benefit over SRP in the management of chronic periodontitis. However, a study conducted in 2015 concluded that Arestin delivered in biodegradable system are a safe and efficient adjunct to SRP and can produce significant clinical benefits when compared to SRP alone.
Doxycycline polymer
Atridox is 10% doxycycline gel system in a syringe which is FDA approved. Observed peak levels is 1,500-2,000 μg/ml in gingival crevicular fluid in 2 hours, which was maintained above 1000 μg/ml for 18-20 hours, gradually decreasing thereafter. Walker et al 2000 evaluated the effectiveness of Atridox on the microbial flora and antibiotic resistance. He stated that there was a significant reduction in anaerobic microorganisms in plaque but there was no change in development of antibiotic resistant or the number of resistant bacteria.
A 9 months study was conducted in 2000 to test the efficacy of biodegradable controlled release doxycycline hyclate into the periodontal pocket. The results showed that subgingival doxycycline hyclate is superior to placebo with oral hygiene and equally effective as SRP in reducing the clinical signs in moderate to severe periodontitis patients.
Metronidazole gel
Elysol contains 25% metronidazole benzoate in a matrix containing a mixture of sesame oil and glyceryl mono-oleate. It is introduced into the periodontal pocket using a blunt canula in viscous consistency but gets liquidized due to body heat, however it forms crystals when in contact with water. A study conducted in 2009 provided a better understanding of metronidazole release kinetics and demonstrated its ability to inhibit bacteroides fragilis growth and hence their use in the treatment of periodontal disease.
Chlorhexidine chip
Periochip is a controlled delivery device and contains 2.5 mg chlorhexidine gluconate in a biodegradable matrix of hydrolysed gelatin cross linked with glutaraldehyde, purified water and glycerine with a dimension of 5 mm × 4 mm × 0.3 mm.
Perio Col CG consists of 2.5 mg chlorhexidine with a dimension of 4 × 5 mm, thickness of 0.25-0.32 mm and 10 mg weight which resorbs after 30 days.
Chlo Site contains 1.5% of xanthan type chlorhexidine (Ghimas Company, Italy). The gel resorbs within 10-30 days and maintains an effective concentration against microorganism for 15 days.
Use of chlorhexidine chip in combination with SRP showed no clinical or microbiologic benefit at 9 monthsA Systematic review in 2006 concluded that the clinical and microbiologic data on chlorhexidine chip is limited and conflicting.
Future Trends
A variety of formulations containing herbs are used nowadays. These formulations show no side effects and at the same time have beneficial effects. These are cost effective too.
Aloe Vera
Peeling of the leaves gives a pulp that provides the medicinal effect of aloe vera. These substances include
• Has the capacity to penetrate the tissue and carry elements with it.
• Provide antiseptic quality and cleansing.
• Vit A, Vit C, Vit E are all needed for various functions of the body.
• Increases the tensile strength of wound.
• Helps in repair and regeneration of injured tissue.
• Have antibacterial, antifungal, antiviral properties and produce analgesia.
• Such as fructose, glucose, and polymannose which can modulate the immune system and have anti-inflammatory actions.
• Enzymes.
Neem
Periodontal disorders are seen to benefit from the use of neem extract. Inhibition of plaque growth and other oral infections is seen. Neem has various actions like: Astringent, Antimicrobial properties, Antiviral, Antibacterial, Anti-inflammatory, and Antiseptic properties. It removes toxins from the body, neutralizes damaging free radicals and purifies the blood. It may have a locally healing enhancing effect. Neem has no known adverse reactions and is available easily.
When neem oil chip was used as LDD system, it resulted in improved clinical parameters and reduced number of P. gingivalisat 21 days.
Turmeric
Turmeric has beneficial properties like–Anti-mutagenic, Antiinflammatory, Anti-microbial, Anti-oxidant, Immuno-stimulant, Hepato-protective, Antiseptic, and additionally it accelerates wound healing.
A combination of turmeric chip, curcumin chip and SRP in treatment of periodontal pockets showed improved plaque and gingival index scores at 80 days.
Green tea
Green tea extract is a naturally occurring antimicrobial agent, consisting of polyphenols (catechin) with anti-collagenolytic, anti-inflammatory and anti-cariogenic properties. Use of thermo-reversible sustained release green tea gel resulted in reduced inflammation and probing depth in chronic periodontitis patients.
Propolis
Propolis is a resinous mixture that honey bees collect from tree buds, sap flows, or other botanical sources. It is used as a sealant for unwanted open spaces in the hive. Its actions are:
• Galangin and hydroxycinnamic acids like caffeic acid.
• Propolis exhibit both immune-suppressive and immunestimulant effects.
• As an oral hygiene product protect against dental caries and periodontal diseases, due to its antimicrobial properties.
• Antioxidant. Conducted a study which indicated a potentially useful role of Semisolid systems containing propolis in the treatment of chronic periodontitis.
Pomegranate
It has Punica granatum and Centella asiatica, which are known to promote tissue healing and modulate host response. Studies using local delivery of C. asiatica and P granatum in combination with SRP showed significant improvement in clinical parameters at 6 months
P granatum when compared to miconazole showed greater inhibition of microbial adherence of S. mitis, S. mutas and C albicans in oral cavity
Statins
Statins like Simvastatin, lovastatin, and pravastatin are specific competitive inhibitors of HMG-CoA reductase (3-hydroxy-2- methyl-glutaryl coenzyme A reductase). They lower cholesterol levels and have been used for the treatment of hyperlipidemia and arteriosclerosis. They also modulate bone formation by increasing the expression of BMP-2 and angiogenesis, hence they have a potential in the field of periodontal therapy.
When 1.2 mg Simvastatin was used in a biodegradable controlled release gel as an adjunct to SRP, improved clinical parameters with intrabony defect fill was observed at 6 months 1.2% atorvastatin was used as an adjunct to SRP can be used promisingly in the management of intrabony defects
Clarithromycin
Clarithromycin is a macrolide antibiotic which can be taken up by host cells and has favourable antimicrobial effect. Use of 0.5% clarithromycin as an adjunct to SRP showed enhanced clinical outcomes in treating chronic periodontitis patients in smokers.
Spirulina
Phycocyanin is one of the major pigment constituents of spirulina which has an anti-inflammatory effect. When spirulina gel was used as an adjunct to SRP, it showed statistically significant decrease in mean probing depth and gain in CAL after 120 days in chronic periodontitis patients [13].
Alendronate
Alendronate is an amino-bisphosphonate which is known to inhibit osteoclastic bone resorption and shows osteo-stimulative property both in-vitro and in-vivo. A study was conducted to explore the efficacy of 1% alendronate gel as an adjunct to SRP in the treatment of intrabony defects in patients with chronic periodontitis [14]. They observed a mean reduction in clinical parameters in alendronate group than in placebo at 2 and 6 months. Additionally, a significantly greater mean % of bone fill was observed in alendronate group than in placebo group.
Metformin
Metformin is an anti-diabetic drug and in vitro studies have shown that it can enhance osteoblastic differentiation and inhibit osteoclastic differentiation [15]. Various studies have been conducted using metformin which have concluded that
• Greatest reduction of intrabony defects was seen with 1% metformin at 6 months when compared to 0.5% and 1.5%.
• OFD+PRF + 1% metformin group showed better results at 9 months in terms of regeneration of intrabony defects, when compared to OFD+PRF, OFD + 1% metformin or OFD alone.
• SRP+1 % metformin group showed greater decrease in PD and CAL gain with significant IBD depth reduction at 9 months when compared to SRP + placebo in patients with moderate to severe periodontitis.
Satranidazole
Satranidazole is another antibiotic that belongs to the 5‑nitroimidazole group and pharmacokinetic studies have showed longer half-life and higher blood levels than metronidazole. When 3% Satranidazole gel+SRP was compared with SRP alone, a significant reduction in number of sites harbouring periodontopathogens was observed at 6 months.
Conclusion
It is shown that LDD can improve the periodontal health when introduced into the periodontal pockets but LDD cannot in any way replace conventional therapy. As a result, the benefit of using LDD alone is highly questionable. LDD compared to systemic antibiotics does not cause the development of resistant bacterial strains. Clinical cases such as localized periodontal lesions that are persistent are good candidates for LDD. Administration of LDD should be based on proper diagnosis, scientific evidence and clinical findings. Thus, it can be concluded that LDD cannot be used as monotherapy, however it can be used as an adjunct to conventional non-surgical periodontal therapy.
REFERENCES
- Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4(1):1-6.
- Caffesse RG, Sweeney PL, Smith BA. Scaling and root planing with and without periodontal flap surgery. J Clin Periodontology. 1986;13(3):205-210.
- Greenstein G. Nonsurgical periodontal therapy in 2000: A literature review. J Am Dent Assoc. 2000;131(11):1580-1592.
- Quirynen M, Teughels W, De Soete M, Van Steenberghe D. Topical antiseptics and antibiotics in the initial therapy of chronic adult periodontitis: Microbiological aspects. Periodontol. 2002;28(1):72-90.
- Bonito AJ, Lux L, Lohr KN. Impact of local adjuncts to scaling and root planing in periodontal disease therapy: A systematic review. J Periodontol. 2005;76(8):1227-1236.
- Herrera D, Alonso B, Leon R, Roldan S, Sanz M. Antimicrobial therapy in periodontitis: The use of systemic antimicrobials against the subgingival biofilm. J clin periodontol. 2008;35:45-66.
- Goodson JM, Haffajee A, Socransky SS. Periodontal therapy by local delivery of tetracycline. J Clin Periodontol. 1979;6(2):83-92.
- Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pocket. Periodontol. 1996;10(1):139-59.
- Greenstein G, Tonetti M. The role of controlled drug delivery for periodontitis. J Periodontol. 2000;71(1):125-40.
- Stoltze K, Stellfeld M. Systemic absorption of metronidazole after application of a metronidazole 25% dental gel. J of clin periodontol. 1992;19(9):693-697.
- Kong LX, Peng Z, Li SD, Bartold PM. Nanotechnology and its role in the management of periodontal diseases. Periodontolo. 2006;40(1):184-196.
- Pavia M, Nobile CG, Angelillo IF. Meta-analysis of local tetracycline in treating chronic periodontitis. J Periodontol. 2003;74(6):916-932.
- Nadig PS, Shah MA. Tetracycline as local drug delivery in treatment of chronic periodontitis: A systematic review and meta-analysis. J Indian Soc Periodontol. 2016;20(6):576.
- Pradeep AR, Rao NS, Naik SB, Kumari M. Efficacy of varying concentrations of subgingivally delivered metformin in the treatment of chronic periodontitis: A randomized controlled clinical trial. J periodontol. 2013;84(2):212-220.
- Pradeep AR, Kumari M, Rao NS, Martande SS, Naik SB. Clinical efficacy of subgingivally delivered 1.2% atorvastatin in chronic periodontitis: A randomized controlled clinical trial. J Periodontol. 2013;84(7):871-879.
Citation: Kamath DG, Haidrus R (2021) Local Drug Delivery in Periodontal Therapy- A Contemporary Review. Adv Pharmacoepidemiol Drug Saf. 10:245.
Copyright: © 2021 Kamath DG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited