Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
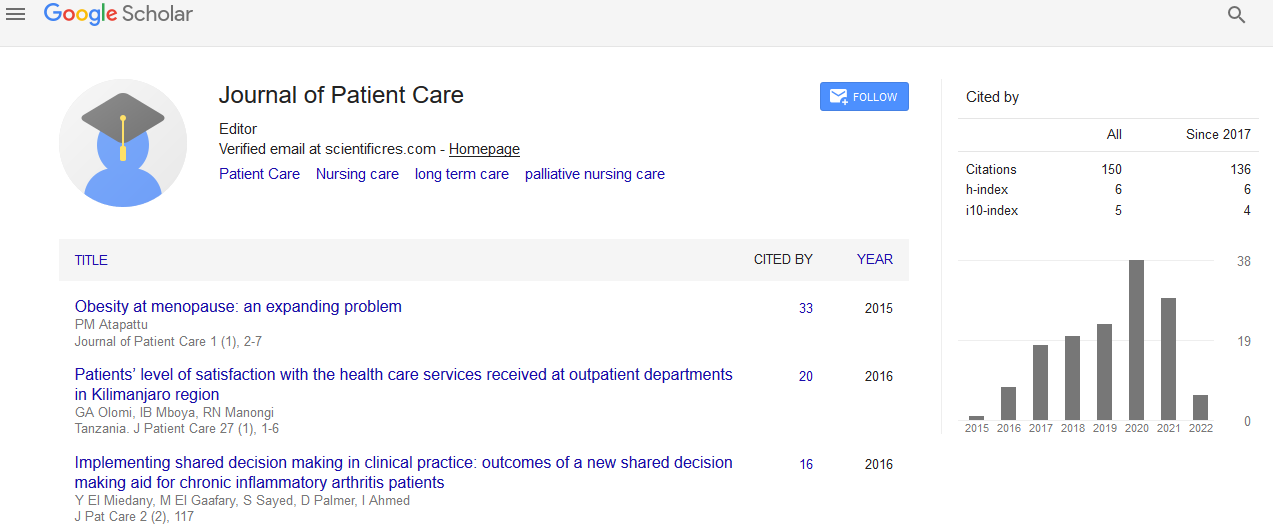
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 6, Issue 2
Impact of Advanced Access Scheduling on Missed Appointment Rates in Primary Care
Helen Yvonne Krippel1*, Miriam K Ross1 and Ronald P Hudak22U.S. Department of Defense Health Agency, Falls Church, Virginia, USA
Received: 11-Apr-2020 Published: 12-Jun-2020, DOI: 10.35248/2573-4598.20.6.149
Abstract
A major problem encountered within outpatient physician offices are missed appointments. The purpose of this study was to determine if there was an association between advanced access scheduling and missed appointment rates for patients scheduled with preferred primary care physicians vis-a-vis non-preferred primary care physicians from a large multispecialty clinic. The health belief model was the conceptual framework because missing a prescheduled appointment is a health behavior. The first and second research questions examined whether there was a statistically significant mean proportion difference between the national no-show rate and the no-show rates of the population samples. The third research question examined the association between the preferred and non-preferred primary care physicians and no-show visit status. Patients prescheduled with primary care providers and over the age of 18 were included in the study, which totaled 4,815 visits. Data were analyzed using one and two sample z test as well as Chi Square test for associations. Study results demonstrated statistically significant mean proportion difference between the national no-show rate and the study and a significant association between physician type and visit status. The results suggested the potential for improved appointment compliance with advanced access scheduling if patients are scheduled with their preferred primary care physician. This study may promote patient care by providing healthcare clinicians and administrators with an understanding of the significance surrounding advanced access scheduling and patient no-show behaviors, thus decreasing missed appointment rates in primary care.
Keywords
Healthcare administration; Scheduling; Missed appointments; Primary care; Patient access
Introduction
A patient who fails to show up for a prescheduled primary care appointment is, unfortunately, not a new worry for healthcare administrators who manage the wide variety of healthcare clinics ranging from physicians’ offices to large multispecialty clinics. Missed appointments have been a constant research focus for healthcare administrators over many decades with minimal impact to reducing the missed appointment rates. The range of these rates remains constant between 5 to 55% [1-5] Previous missed appointment research has provided healthcare administrators with some tools and resources dedicated to decreasing missed appointment rates. For example, research exploring predictive methods, classification models, exploratory explanations, impacts surrounding missed appointments, and the development of countless administrative strategies used to reduce missed appointment rates continues to reveal to healthcare administrators that the complex, multifaceted origins surrounding missed appointments are vast and definitive solutions are slim [1,6-8]. However, regardless of all the efforts and energy dedicated to the missed appointment dilemma, it continues to be a major concern that healthcare administrators need to fully examine and strategically scrutinize in order to achieve specific, sustainable, and noticeable results in decreasing missed appointment rates.
Method
Problem statement
Patients who fail to attend prescheduled primary care appointments with a preferred primary care physician or a nonpreferred primary care physician set off a series of damaging events that can impact a host of elements. A preferred primary care physician is defined as one who practices general family medicine and whom the patient sees regularly and has developed a trusting medical relationship. In contrast, a nonpreferred primary care physician is defined as one who practices general family medicine but the patient has not previously seen and has not developed a trusting medical relationship.
Missing prescheduled primary care appointments can have serious consequences related to a patient’s health and wellness [9-11]. In addition, missed prescheduled primary care appointments can contribute to overall financial impediments to patients, physicians and health care spending [5,12-17]. Furthermore, missed prescheduled primary care appointments increases the potential of weakening the physician-patient relationship [18,19].
Missed prescheduled primary care appointments also have serious negative health and wellness impacts. Patients who miss their appointments create disorder and self-inflicted interference with their care and the potential delivery of timely treatment. Patients who miss appointments put themselves at risk for worsening current chronic medical conditions because chronic illnesses require regular visits to the physician for monitoring, medication, and care plan management [9-11]. Failing to attend a prescheduled primary care appointment jeopardizes patients’ wellness opportunity for the prevention and possible identification of new, preventable medical conditions [9,10,11].
Patients missing prescheduled appointments also impact other patients who are seeking appointments with a primary care physician [2]. Patients who are no-shows to prescheduled appointments prevent other patients from receiving timely medical care. When a missed appointment happens, there is not sufficient time to rebook the appointment, therefore negatively impacting other patients calling into the office for appointments.
Missed prescheduled appointments have serious negative impacts on the physician-patient relationship. In primary care, being able to have scheduled appointments with a preferred primary care physician encourages the growth of the physicianpatient relationship, which promotes positive patient behaviors and healthy outcomes [18,19]. Physician-patient relationships involve trust, respect and engagement, all of which are developed over time [19,20]. Research has provided healthcare administrators with the understanding that positive, continuous physician-patient relationships can positively impact health outcomes of patients [19-21]. Patients repeatedly scheduled with non-preferred primary care physicians impact continuity of care because a long-term patient-physician relationship is unable to develop [22].
In addition to clinical implications, missed prescheduled primary care appointments have serious financial implications for patients, physicians, healthcare administrators and the national health care system. Physician office enforcement of missed appointment fees and no-show policies result in financial penalties and potential dismissal procedures that patients will endure for failing to attend appointments [5,13,23]. Missed appointment fees are expenses that insurance companies will not cover and are patients’ financial responsibility [16]. No-show policies inform patients of their risk of being dismissed from the physician office for excessive missed appointments. Dismissals from primary care physician offices often result in patients seeking medical attention in the emergency room that can result in higher copays and additional out-of-pocket financial responsibilities [14,15,17]. These preventable emergency room visits are a major financial burden on the national healthcare system by generating billions of dollars in expenses annually [12,15,24].
Physician offices also experience financial setbacks from missed appointments, such as an inability to capture budgeted profits from expected visits, waste of scheduled resources and increased operational expenses related to numerous policies and procedures designed specifically to decrease missed appointments [9,12,24,25]. The physician office cannot capture expected revenues when patients miss prescheduled appointments. The average cost associated with a missed primary care appointment averages close to $200 per patient visit which can add up to hundreds of thousands of dollars in annual lost revenue for the physician office [12,16].
Missed patient appointments negatively impact the physician office ’ s operational budgeted expenses related to staffing resources. The number of physicians and staff scheduled to care for patient needs is based on a specific number of prescheduled patients. Therefore, when patients miss appointments. it creates physician idle time, decreases physician productivity and generates over-staffing expenses [26]. Physician offices can also incur fluctuating operational expenses driven by daily patient volumes for prescheduled appointments such as direct mailings, auto reminder phone calls, advanced texting programs and email. These proactive strategies to address missed appointments contribute to additional operational expenses [25,27,28].
One approach to addressing missed prescheduled appointments is the advanced access scheduling model. Also known as open access or same day scheduling, this management technique offers patients appointments with a preferred primary care physician on the day the patient calls, or within 24 hours of the schedule request, regardless of medical urgency [24,29-35]. Unfortunately, there is limited research to assist healthcare administrators in determining the utility of this scheduling technique.
In summary, the problem is the research gap between missed appointments in relation to advanced access scheduling for preferred vis-à-vis non-preferred primary care physicians.
Purpose statement
The purpose of this non-experimental quantitative, correlation study was to determine if there was an association between advanced access scheduling and missed appointment rates, specifically focusing on no-shows with preferred vis-a-vis nonpreferred primary care physicians. The dependent variables of the study were missed appointment rates with preferred primary care physicians and missed appointment rates with nonpreferred primary care physicians. The independent variable was the advanced access scheduling model.
Potential for positive patient care
This study was designed to promote positive patient care because reducing missed appointments rates may contribute to better healthcare access, better healthcare outcomes, and controllable healthcare finances. Specifically, patients who miss prescheduled primary care appointments put themselves and others at risk for negatively impacting health and wellness, straining overall finances, and compromising the physician-patient relationship. Healthcare administrators need to be able to accurately identify progressive operational opportunities and contribute to decreasing inefficiencies for the overall positive promotion of healthy medical and financial outcomes. The knowledge gained from this study should strengthen healthcare administrators ’ decision-making to enable better operational evaluation techniques and strategic deployment of action plans to improve missed appointment rates in physician offices and multispecialty clinics.
Significance of the study
Given the multiple dimensions that occur as a result of missed prescheduled primary care appointments, the findings may be used to ensure patients, physicians, clinics and healthcare administrators appreciate the complexity of the missed appointment challenges and partner for solutions. The results of this study may improve healthcare administrators understanding of the dynamics surrounding the advanced access scheduling model. In addition, the results of this study may lead healthcare administrators to establish advanced access scheduling criteria, best practices and action plans, thus creating a systematic and effective approach to reducing missed appointment rates. In addition, healthcare administrators would gain operational knowledge targeted to achieve improved access, patient experiences, and patient health outcomes while decreasing missed appointment rates and operational inefficiencies. As a result, a notable reduction in missed appointment rates should have a positive impact on patients, the physicians, clinics and the national health care system.
Research questions
The three research questions were:
1. Is there a statistically significant mean proportion difference between the national no-show rate and the missed appointment rate of the non-preferred primary care physician sample?
2. Is there a statistically significant mean proportion difference between the national no-show rate and the missed appointment rate of the preferred primary care physician sample?
3. Is there an association between primary care physician type, preferred and non-preferred, and advanced access scheduling model visit status of arrived, cancelled, and no-show?
Conceptual framework
The conceptual framework for this study was the health belief model. The health belief model is used to explain and predict health behaviors of individuals [36,37]. Missing a prescheduled primary care appointment is a health behavior that can evolve into identifiable patterns of undesirable patient health behaviors [6]. Patients existing missed appointment behavior may alter if there is a benefit in going to the appointment, which may result in the patients attending their prescheduled primary care appointment [37,38].
Approach
This study was a non-experimental quantitative, correlational research study designed to examine if there was an association between advanced access scheduling on missed appointment rates for preferred primary care physicians and non-preferred primary care physicians. A non-experimental quantitative, correlational research study is guided by a research question and hypotheses that are built on existing knowledge proposing an association between variables [39] therefore the research design was considered appropriate for this study.
Participants
This study included a target population of patients who were prescheduled for primary care visits from multispecialty and primary care office that is part of a large medical group. The target population for this study was patients, 18 years of age and older, who had been prescheduled with a primary care physician.
Visit data of patients that were seen by specialty physicians, pediatricians, nurse visits, chronic care management, outpatient lab, radiology, and immediate walk-in care visits at the multispecialty and primary care medical office were excluded. Prescheduled primary care appointments that were reserved 25 hours or more prior to the scheduled appointment were also excluded. For reasons surrounding the health belief model, which is used to focus on individual beliefs about health, this study did not include patients under the age of 18. Patients under the age of 18, also termed pediatric patients, are dependent upon a guardian or parent to accompany the patient to the appointment as required by law. Additionally, patients who were not prescheduled with thorough registration information that comprised the omission of an identified primary care physician, current insurance or self-pay section validated and completed demographic section were excluded.
Sampling and sampling procedures
It was not feasible for this study to examine 86,672 prescheduled primary care visits for 2018. Therefore, a probability sampling was conducted, specifically, cluster sampling. The total number of 2018 prescheduled primary care patient visits were grouped into each calendar month, January through December, and then combined into fiscal quarters, that is, January - March, April - June, July - September, and October - December. One month was randomly selected from each fiscal quarter in 2018 using a rotating pattern from the groupings. The total patient visits for these four months totaled 35,574. After exclusions and inclusions, the total patient visits for prescheduled primary care analysis totaled 4,815.
As noted in Table 1, there were more female patients than male patients. Female patients represented 65.9% (n=3,175) of the population, whereas 34.1% (n=1,640) were males. The patients spanned in age from 18 to 99 years old. African American patients were the majority of the sample. Regarding ethnicity, the majority identified as Not Hispanic/Latino/Spanish origin patients. Almost half the patients had commercial insurance while a third had Medicare/Medicare HMO insurance. And, finally, Cook County, where the large multispecialty and primary care office is located, serviced most of the patients.
Table 1: Descriptive Statistics Demographics - Gender, Age, Race, Ethnicity, Insurance Type, and Geographical Location via Zip Code.
| Data Element | Characteristic | Frequency | Valid Percentage (%) |
|---|---|---|---|
| Gender | Male | 1,640 | 34.10% |
| Female | 3,175 | 65.90% | |
| Age | 18-29 | 524 | 10.90% |
| 30-39 | 613 | 12.70% | |
| 40-49 | 887 | 18.40% | |
| 50-59 | 941 | 19.50% | |
| 60-69 | 925 | 19.20% | |
| 70-79 | 653 | 13.60% | |
| 80-89 | 232 | 4.80% | |
| 90-99 | 40 | 0.80% | |
| Race | Caucasian | 1,160 | 24.90% |
| African American | 2,926 | 62.70% | |
| Asian | 11 | 0.20% | |
| Other | 203 | 4.30% | |
| Declined | 367 | 7.90% | |
| Missing | 148 | ||
| Ethnicity | Hispanic/Latino/Spanish Origin | 188 | 4.10% |
| Not Hispanic/Latino/Spanish Origin | 3,947 | 84.80% | |
| Declined | 518 | 11.10% | |
| Missing | 162 | ||
| Insurance | Commercial | 2,345 | 48.70% |
| Medicare/Medicare HMO | 1.64 | 34.10% | |
| Medicaid | 706 | 14.70% | |
| Other/Crime Victim/Motor Vehicle | 11 | 0.20% | |
| Self-Pay | 113 | 2.30% | |
| Zip Code | Cook County, Illinois | 3,910 | 81.20% |
| Other Illinois Counties | 801 | 16.60% | |
| Out of State Counties (14) | 104 | 2.20% |
Data collection and management
The secondary data set utilized in the research study was obtained from the electronic appointment scheduling system of the medical office described as a multispecialty and primary care office that is a part of a large medical group.
Results
The results are organized by the three research questions.
1. Is there a statistically significant mean proportion difference between the national no-show rate and the missed appointment rate of the non-preferred primary care physician sample? The answer is yes. Specifically, applying the one sample z-test of proportions, it was found that the true proportion of the noshow rate in this study had a statistically significant difference in the mean proportion than the national no-show rate.
2. Is there a statistically significant mean proportion difference between the national no-show rate and the missed appointment rate of the preferred primary care physician sample? The answer is yes. Applying the one sample z-test of proportions, it was found that the true proportion of the no-show rate in this study had a statistically significant difference in the mean proportion than the national no-show rate.
3. Is there an association between primary care physician type, preferred and non-preferred, and advanced access scheduling model visit status of arrived, cancelled, and no-show? The answer is yes. However, the association is weak because the V value is closer to 0 than 1. This small Cramer’s V value indicates that even though there is an association between the variables, the strength of the association is not very high.
Discussion
Previous research made assumptions that appointments made 24 hours or less to the actual appointment have little to no missed appointment rates [5,24,31,33,34]. This study’s results showed that patients did miss prescheduled appointments made 24 hours or less prior to the actual appointment. In fact, the missed appointment rate in this study for prescheduled appointments made 24 hours or less was 5.5%.
Similarly, previous research calculated missed appointment rates between wide ranges of 5% to 55%, [1-5]. Boyer [40] and Medical Group Management Association [41] claim current benchmarks for national no-show rates in primary care are 19%. The missed appointment rate in this study was 5.5%, which aligned with the lower end of the missed appointment percentage range in missed appointment rate research and much lower than the MGMA’s benchmarks.
Findings from past studies have shown that patients scheduled with non-preferred physicians are more likely to miss initial appointments and subsequent appointments or not seek care at all [19,20,42]. This aligned with the findings in this study, specifically, there is a statistical significant association between preferred vis-a-vas non-preferred primary care physicians and the advanced access scheduling model’s status of arrived, cancelled and no-show. The percentage of advanced access scheduled missed appointments with a preferred primary care physician was 46.6%, whereas the percentage of advanced access scheduled missed appointments with a non-preferred primary care physician was higher (53.4%).
Recommendations
The following recommendations are based on the findings of the three research questions.
1. Healthcare administrators should align appointment policies and procedures, as well as patient no-show behaviors, to facilitate the appointment of patients with their preferred primary care physician.
2. Healthcare administrators should consider policies and procedures to minimize the appointment of patients with nonpreferred primary care physicians.
3. Healthcare administrators should consider incorporating or adapting the advanced access scheduling model to optimize the number of patients who make their appointments and minimize the number of patients who cancel or are no-shows.
4. Future research should be conducted to consider other variables. For example, extending the research to include reason for the visit, primary diagnosis or level of service, as well as previous missed appointment patterns, may align identification of possible predicative health behaviors based on the patient’s medical conditions and past behaviors. In addition, as suggested by Squires & Dorsen (2018), research might be extended to include qualitative variables that align with the quantitative variables.
Implications
This study’s findings have implications for professional practice and patient care regarding the impact of advanced access scheduling on missed appointment rates in primary care. Regarding professional practice implications, healthcare administrators are continuously challenged to solve no-show appointments which results in lost revenue and quality issues related to patient care [9-12,24,25]. This study provides healthcare administrators with affirmation that advanced access scheduling models may improve the number of patients who keep their appointments [31,34]. In addition, healthcare administrators are provided with an understanding of the significance surrounding advanced access scheduling and patient no-show behaviors [1,30-34]. Accepting that certain advanced access scheduling factors impact no-show behavior is important to healthcare administrators when developing interventions to lessen the number of missed appointments. As such, this study ’ s results substantiate the need for necessary changes in scheduling templates, policies including overbooking and best practices for advanced access scheduling. Knowing that patients are more likely to attend advanced access prescheduled appointments with preferred primary care providers allows healthcare administrators to design and implement more effective provider scheduling templates to improve prescheduled appointment compliance.
Regarding patient care implications, patients who fail to attend prescheduled appointments with a preferred, or non-preferred, primary care physician stimulate a host of unfavorable health outcomes. Reducing missed appointment rates reverses these problematic outcomes and improves compliance with medical treatments [9-11,17]. Therefore, determining the impact that advanced access scheduling has on missed appointment rates in primary care supports appointment attendance. This study suggests that advanced access scheduling models may positively influence patient appointment behaviors and health outcomes as well as contributing to reducing the nation’s health care costs.
Conclusion
This study addressed the knowledge gap in missed appointment literature by contributing to existing research about advanced access scheduling and missed appointments with preferred vis-avis non-preferred primary care physicians. The findings indicated that there were significantly different no-show rates in this study than that of the national no-show rates suggesting an advantage of using an advanced access scheduling model in primary care clinics. Results also indicated a statistical significant association between physician type, that is, preferred vis-à-vis non-preferred primary care, and the visit status of arrived, cancelled, and no-show which suggests that the physician-patient relationship contributes to attending prescheduled appointments. Based on this study, advanced access scheduling with preferred primary care physicians should lead to reduction of missed appointment rates, which enhances positive health outcomes for patients, decreases financial impediments, and strengthens the physician-patient relationship. Healthcare administrators have a responsibility to embrace best practices to develop, refine, and execute policies and procedures that improve patients’ quality of care and health care experience. Creating positive health care experiences that encourage patients to attend appointments is essential for the health of patients and the nation and contributes to positive patient care.
REFERENCES
- Anisi S, Zarei E, Sabzi M, Chehrazi M. Missed appointments: factors contributing to patient no-show in outpatient hospital clinics in Tehran, Iran. Shiraz E-Medical J. 2018;19:e63238.
- Boos EM, Bittner MJ, Kramer MR. A profile of patients who fail to keep appointments in a veterans affairs primary care clinic. Wisconsin Medical Society. 2016;115:185-190.
- Drewek R, Mirea L, Adelson PD. Lead time to appointment and no-show rates for new and follow-up patients in an ambulatory clinic. T Health Care Man. 2017;36:4-9.
- Goffman RM, Harris SL, May JH, Milicevic AS, Monte RJ, Myaskovsky L, et al. Modeling patient no-show history and predicting future outpatient appointment behavior in the Veterans Health Administration. Military Med. 2017;182:e1708-e1714.
- Liu N. Optimal choice for appointment scheduling window under patient no- show behavior. Prod Oper Manag. 2016;25:128-142.
- Williams AE, Ellis DA, Wilson P, McQueenie R, McConnachie A. Understanding repeated non-attendance in health services, a pilot analysis of administrative data and full study protocol for a national retrospective cohort. BMJ. 2017;7:e014120.
- Samuels RC, Ward VL, Melvin P, Macht-Greenberg M, Wenren LM, Yi J, et al. Missed appointments: factors contributing to high no-show rates in an urban pediatrics primary care clinic. Clin Pediatr. 2015;54:976-982.
- Torres O, Rothberg MB, Garb J, Ogunneye O, Onyema J, Higgins T. Risk factor model to predict a missed clinic appointment in an urban, academic, and underserved setting. Popul Health Manag. 2015;18:131-136.
- Aggarwal A, Davies J, Sullivan R. “Nudge” and the epidemic of missed appointments: Can behavioural policies provide a solution for missed appointments in the health service? J Health Organ Manag. 2015;30:558-564.
- AlRowaili MO, Ahmed AE, Areabi HA. Factors associated with no-shows and rescheduling MRI appointments. BMC Health Services Research. 2016;16:679.
- Hwang AS, Atlas SJ, Cronin P, Ashburner JM, Shah SJ, He W, et al. Appointment no-shows are an independent predictor of subsequent quality of care and resource utilization outcomes. J Gen Intern Med. 2015;30:1426-1433.
- Kheirkhan P, Feng Q, Travis LM, Tavakoli-Tabasi S, Sharafkhaneh A. Prevalence, predictors, and economic consequences of no-shows. BMC. 2016;16:13.
- Liu N, Ziya S. Panel size and overbooking decisions for appointment-based services under patient no-shows. Prod Oper Manag. 2014;23:2209-2223.
- McGough PM, Norris TE, Scott JD, Burner TG. Meeting the demands of the Affordable Care Act: improving access to primary care. Popul Health Manag. 2017;20:87-89.
- Ostermeyer B, Baweja NUA, Schanzer B, Han J, Shah AA. Frequent utilizers of emergency departments: characteristics and intervention opportunities. Psychiatr Ann. 2018;48:42-50.
- Peck III EA, Roberts III LW, O’Grady JM. Clinical neuropsychology practice and the Medicare patient. In L.D. Ravdin, & H.L. Katzen (Eds.), Handbook on the neuropsychology of aging and dementia (2nd ed.). Switzerland: Springer. 2019;193-216
- Weisz D, Gusmano MK, Wong G, Trombley J. Emergency department use: a reflection of poor primary care access? Am J Manag Care. 2015;21:e152-e160.
- Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the physician. Ann Fam Med. 2014;12:573-576.
- Dang BN, Westbrook RA, Njue SM, Giordano TP. Building trust and rapport early in the new doctor-patient relationship: a longitudinal qualitative study. BioMed Central Medical Education. 17.
- Chipidza FE, Wallwork RS, Stern TA. Impact of the doctor-patient relationship. The Primary Care Companion for CNS Disorders. 2015;17.
- Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE. 2014;9:e94207.
- Balasubramanian H, Biehl S, Dai L, Muriel A. Dynamic allocation of same-day requests in multi-physician primary care practices in the presence of prescheduled appointments. Health Care Manag Sci. 2014;17:31-48.
- Huang J, Zuniga P. Effective cancellation policy to reduce the negative impact of patient no-show. Journal of the Operational Research Society. 2014;65:610-615.
- Norris JB, Kumar C, Chand S, Moskowitz H, Shade SA, Willis DR. An empirical investigation into factors affecting patient cancellations and no-shows at outpatient clinics. Decision Support Systems. 2014;57:428-443.
- Saeed S, Somani N, Sharif F, Kazi AM. Evaluating the effectiveness of text messaging and phone call reminders to minimize no show at pediatric outpatient clinics in Pakistan: protocol for a mixed-methods study. JMIR Research Protocols. 2018;7:e91.
- Xiao G, Dong M, Li J, Sun L. Scheduling routine and call-in clinical appointments with revisits. Int J Prod. 55:1767-1779.
- McLean SM, Booth A, Nancarrow SA. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016;10:479-499.
- Palacios-Barahona U, Hernandez-Rendon M, Gaviria-Lopez A, Guerra-Herrera AC, Valencia-Diaz E, Ramos-Castaneda JA, et al. Effectiveness of text messages, calls and email on adherence to medical appointments review of systematic reviews and meta-analysis. Rev CES Med. 2018;32:14-22.
- Ansell D, Crispo JAG, Simard B, Bjerre LM. Interventions to reduce wait times for primary care appointments: a systematic review. BMC Health Serv Res. 2017;17:295.
- Kiran T, O’Brien P. Challenge of same-day access in primary care. Can Fam Physician. 2015;61:399-400.
- Malham SA, Touati N, Maillet L, Gaboury I, Loignon C, Breton M. What are the factors influencing implementation of advance access in family medicine units? A cross-case comparison of four early adopters in Quebec. Intern J Fam Med. 2017;2017:1-15.
- Riedl B, Kehrer S, Werner CU, Schneider A, Linde K. Do general practice patients with and without appointment differ? Cross-sectional study. BMC Family Practice. 2018;19:1-18.
- Samorani M, LaGanga LR. Outpatient appointment scheduling given individual day-dependent no-show predictions. Eur J Oper Res. 2015;240:245-257.
- Tsai PFJ, Teng,GU. A stochastic appointment scheduling system on multiple resources with dynamic call-in sequence and patient no-shows for an outpatient clinic. Eur J Oper Res. 2014;239:427-436.
- Jones CJ, Smith H, Llewellyn C. Evaluating the effectiveness of heath belief model interventions in improving adherence: a systematic review. Health Psychol Rev. 2014;8:253-269.
- Jones CJ, Smith H, Llewellyn C. Evaluating the effectiveness of heath belief model interventions in improving adherence: a systematic review. Health Psychol Rev. 2014;8:253-269.
- Montanaro EA, Bryan AD. Comparing theory-based condom interventions: health belief model versus theory of planned behavior. Health Psychol. 2014;33:1251-1260.
- Cronin RM, Hankins JS, Byrd J, Pernell BM, Kassim A, Adams-Graves P, et al. Modifying factors of the health belief model associated with missed clinic appointments among individuals with sickle cell disease. Hematology. 2018;23:683-691.
- Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches (4rded), Thousand Oaks, CA: Sage. 2014.
- Boyer L. Which wins? The national average no-show rate or yours? 2019.
- Medical Group Management Association (MGMA). MGMA 2018 DataDive Practice Operations Data. 2018.
- Fuertes JN, Toporovsky A, Reyes M, Osborne JB. The physician-patient working alliance: theory, research, and future possibilities. Patient Education and Counseling. 2016;100:610-615.
Citation: Krippel HY, Ross MK, Hudak RP (2020) Impact of Advanced Access Scheduling on Missed Appointment Rates in Primary Care. J Pat Care 6:149. doi: 10.35248/2573-4598.20.6.149
Copyright: © 2020 Krippel HY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.