PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
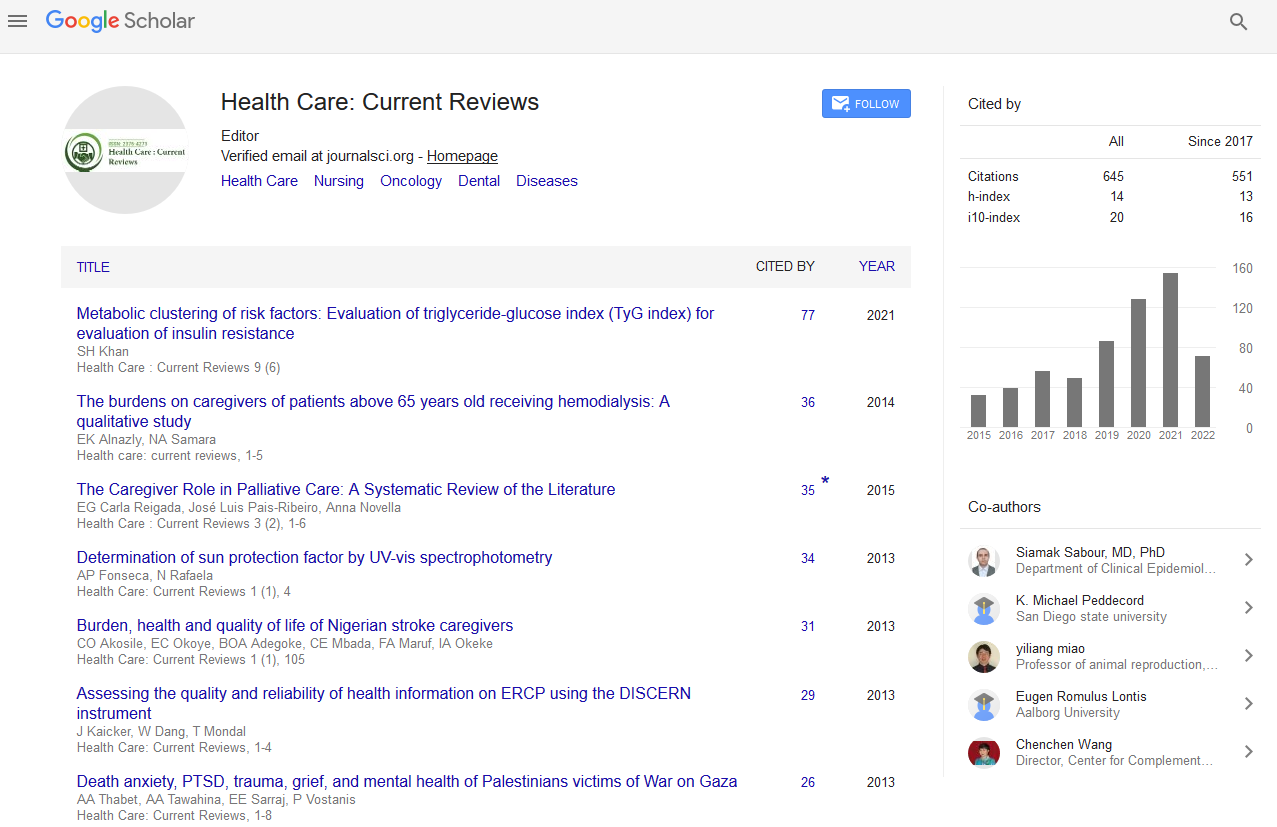
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2019) Volume 7, Issue 1
Health Reform as Political Instrument: Achieving Universal Health Coverage
Tabish SA*Received: 23-Nov-2018 Published: 08-Feb-2019, DOI: 10.35248/2375-4273.19.07.239
Abstract
India constitutes nearly one-fifth of the world’s population. People living in different parts of the country and states differ in their ethnic origin, culture, religious beliefs and other ways that influence their health status. An effective and efficient health care delivery system is indispensable. India has to focus on ever-evolving healthcare needs of its population. Affordability of quality care is a major issue. In India a large number of people still live below poverty line, the affordability of quality care needs to be addressed. With the rise in awareness, affordability and lifestyle diseases, healthcare is one of the essential needs of the nation. Launching of National Health Protection Scheme (NHPS) is a step in the right direction. The NHPS will be effective from 25 September 2018 as a political instrument towards achieving Universal Health Coverage. This is the world’s largest health insurance scheme covering nearly 40 percent of India’s population. Its success will depend on how well the plan is defined and implemented on the ground level. Primary care has to make affordable and accessible to all. It will improve the wellness of the population and reduce the overall cost to the exchequer. Interdisciplinary approach to healthcare underscores the importance of applying integrative strategies to the practice of health sciences. Continued progress and a large public-sector role in health systems reform are crucial. If effectively implemented, the NHPS is expected to make a substantial difference in the Indian health care system over the next decade. Being the largest health insurance plan, from a global perspective, its vision is to cover 50 crore poor and vulnerable beneficiaries.
Keywords
Health reform as political instrument; National health protection scheme; Universal health coverage; Ayushman bharat; Health insurance; Human development indicators
Introduction
AB-NHPS in nutshell
AB-NHPS is the biggest government-sponsored healthcare scheme in the world that aims to provide healthcare facilities to over 10 crore families covering urban and rural poor. It offers an insurance cover of INR 500,000 per year, which will cover almost 50 crore citizens. This scheme will be available for 10.74 crore beneficiary families (poor and vulnerable people), identified occupational category of urban workers' families as per the latest Socio-Economic Caste Census (SECC) data covering both rural and urban, and about 50 crore Indian citizens
AB-NHPS will target about 10.74 crore poor, deprived rural families and. The scheme is designed to be dynamic and aspirational and it would take into account any future changes in the exclusion/ inclusion/deprivation/ occupational criteria in the SECC data.
Key features of AB-NHPS
1. It provides a cover of INR 5oo,ooo per family per year for secondary and tertiary medical care facilities.
2. Those eligible under the health insurance scheme get automatic coverage. Eligibility is based on Socio-Economic Caste Census (SECC) database.
3. In case of hospitalization, eligible beneficiary doesn’t need to pay anything under the scheme provided he/she goes to any government or empanelled private hospital. A beneficiary covered under the scheme will be allowed to take cashless benefits from any public/private empanelled hospitals across the country.
4. All kinds of diseases are covered from day one of this policy. The benefit cover includes both pre and post hospitalization expenses.
To control costs, the payments for treatment will be done on package rate (to be defined by the Government in advance) basis.
One of the core principles of this scheme is to co-operative federalism and flexibility to states.
The expenditure incurred in premium payment will be shared between Central and State Governments in specified ratio (60:40). The total expenditure will depend on actual market determined premium paid in States where AB-NHPS is implemented through insurance companies. In States where the scheme will be implemented in Trust/ Society mode, the central share of funds will be provided based on actual expenditure or premium ceiling (whichever is lower) in the predetermined ratio.
In partnership with NITI Aayog, a robust, modular, scalable and interoperable IT platform has been made operational which entails a paperless, cashless transaction.
Eligibility criteria for AB-NHPS
In rural areas:
1. Families living in only one room with “kuchcha walls and kuchcha roof"
2. Families with no adult members aged between 16 and 59
3. Female-headed family with no adult male member in the 16-59 age group
4. Families having at least one disabled member and no able-bodied adult member
5. SC/ST households
6. Landless households deriving major part of their income from manual casual labour
7. Destitute and those surviving on alms
8. Manual scavenger families
9. Primitive tribal groups
10. Legally-released bonded labourer
In urban areas:
Rag picker, beggar, domestic worker, street vendor/cobbler/ hawker/ other service provider working on streets, construction worker/plumber/mason/labour/painter/welder/security guard/coolie and other head-load workers, sweeper/sanitation worker/gardener, home-based worker/artisan/handicrafts worker/tailor, transport worker/driver/conductor/helper to drivers and conductors/ cart puller/ rickshaw puller, shop worker/assistant/peon in small establishment/ helper/delivery assistant/attendant/waiter, electrician/mechanic/ assembler/repair worker, washer-man, watchman.
Factors Necessitating Health Reform
Burden of disease
Even India is facing triple burden of disease- communicable diseases, non-communicable (lifestyle) diseases and emergent infection. Diabetes, cardiovascular diseases, chronic respiratory diseases, cancers, suicides are major public health problems leading to increased mortality during the last two decades.
According to India: Health of the Nation’s State Report, life expectancy at birth improved in India from 59.7 y in 1990 to 70.3 y in 2016 for females, and from 58.3 y to 66.9 y for males [1]. Three infants die every two minutes on an average in India mainly due to lack of access to water, sanitation, proper nutrition or basic health services for this problem. ‘Every five seconds, a child under the age of 15 dies’ [2].
As per new mortality estimates released by UNICEF, the WHO, the United Nations Population Division and the World Bank Group, an estimated 6.3 million children aged below 15 died in 2017, or 1 every 5 seconds, mostly of preventable causes. Most of these deaths - 5.4 million - occur in the first five years of life, with new-borns accounting for around half of the deaths. Without urgent action, 56 million children under five will die from now until 2030 - half of them newborns [2].
India is going through a period of epidemiological and demographic transition. Infectious diseases are still persisting as major health problems in spite of having national programmes for the control of most of these diseases for almost six decades now. There are emerging and re-emerging infectious diseases which are adding to the burden of diseases. Moreover, there is an increasing prevalence of noncommunicable diseases as a result of lifestyle changes and urbanization. These are the challenges that need an appropriate response.
In 1990, India’s per capita income was $380 (Rs 24,867), rising 340 percent to $1,670 (Rs 1,09,000) in 2016, as per data from the World Bank. Over the same period, the number of diabetes cases increased by more than 123 percent. Currently, one in every four people under 25 has adult-onset diabetes, a condition more usually seen in 40-50-yearolds, according to the Indian Council of Medical Research’s youth diabetes registry [3].
Out of pocket (OOP) expenditure for treatment of noncommunicable diseases is the highest, followed by that of other diseases and disability, then reproductive health related diseases and the least is for communicable diseases. OOP expenditures for maternal healthcare in private health facilities are much higher than in public health facilities regardless of types of disease. Women from households having insurance of any member spent less than that of women from households not having health insurance [4].
India contributed almost one-fifth (18.6%) of the global cardiovascular disease (CVD) burden, as measured by disabilityadjusted life years, in 2016 [5]. Although this proportion is only slightly above the share of the world’s population that lives in India (17.7% in 2015) [6]. It is likely to increase in the future for 3 main reasons. First, India is expected to make the greatest contribution to global population growth of any country until at least 2050 [7]. Second, India’s population is aging and urbanizing: the share of people aged more than 60 years is estimated to double from 8.9% to 19.4% between 2015 and 2050 and the percentage of Indians living in cities is projected to grow from 30.9% in 2010 to 50.3% in 2050 [8]. Third, the rise in living standards and socio-cultural transitions in India are likely to lead to more obesogenic lifestyles [9].
Given the detrimental effects of CVD on health outcomes, financial risk protection and economic growth, the course of India’s CVD epidemic will directly impact several Sustainable Development Goals (SDGs) [10-12]. These include SDG 1 (“End poverty in all its forms everywhere”) and SDG 3 (“Ensure healthy lives and promote well-being for all at all ages”) as well as their corresponding targets SDG 3.4 (“By 2030, reduce by one-third premature mortality from noncommunicable diseases”) and SDG 3.8 on achieving universal health coverage. Considering the size and growth of India’s population, the development of its CVD epidemic over the next decade will also have a decisive impact on the world’s ability to achieve the SDGs [7,13].
CVDs have now become the leading cause of death in India. A quarter of all mortality is attributable to CVD. An accelerated buildup, the early age of disease onset in the population, and the high case fatality rate is a serious concern. Premature mortality in terms of years of life lost because of CVD in India is gradually increasing [14].
Diabetes is India’s fastest growing disease, 72 million cases recorded in 2017, the figure expected to nearly double to 134 million by 2025. India currently represents 49 percent of the world’s diabetes burden. Currently, one in every four people under 25 has adult-onset diabetes, a condition more usually seen in 40-50-year-old [3].
Death due to cardiovascular disease is on the rise in India, causing more than one quarter of all deaths in the country in 2015 and affecting rural populations and young adults the most [15]. The rates of dying from ischaemic heart disease in populations aged 30 to 69 increased rapidly in rural areas of India and surpassed those in urban areas between the year 2000 and 2015. The younger adults, especially those born after 1970, have the highest rate of death due to heart problems caused by narrowing of the heart's arteries. Making progress in fighting the leading cause of death in India is necessary for making progress at the global level [15].
In a country of 1•34 billion people with cultural and lifestyle diversities, there is varied epidemiological transition among the states of India from 1990 to 2016 [16].
Demographic transition
India, with a total of 1,349,985,632 (1.34 billion) individuals is the second most populous country in the world, while China is the foremost with over 1,415,489,506 (1.41 billion) people. India represents almost 17.85% of the global population, implying one out of six people on this planet is of Indian origin. With the population growth rate at 1.2%, India is predicted to cross 1.53 billion in population by the end of 2030 [17].
More than 50% of India's population at present is below 25 years, while over 65% are under 35 years of age. About 72.2% of the population occupy around 638,000 villages while the remaining 27.8% reside in about 5,480 towns and urban agglomerations. The birth rate (childbirths per 1,000 people per year) is 22.22 births/1,000 populations (2009 estimated), while the death rate (deaths per 1000 individuals per year) is 6.4 deaths/1,000 populations [18-20].
To respond to the challenge, India decided to transform its health system by introducing an innovative and path breaking scheme - the Ayushman Bharat-National Health Protection Mission - during its 2018-2019 budgets. This scheme is effective from September 25, 2018, offers free health insurance benefits cover for over 40% of the total population and is already making huge waves globally.
Universal Health Coverage
Good health is the foundation of any country’s human capital. The health of a nation can be raised by establishing massive rural health infrastructure, with human resources. This requires over 500,000 trained doctors, over 700,000 nurses and other health care workers, 25,000 primary and community health centres, 1,600,000 sub-centres, complemented by 22,000 dispensaries, and 2,800 hospitals practicing the Indian system of medicine and homeopathy. This infrastructure, however, faces deficiencies like the lack of equipment, financial constraints etc. Other inadequacies include lack of access to essential drugs (only 35% have access, compared to the UMI reference level of above 82%); immunization below 12 years is 60% compared to the UMI level of over 90%.
A responsive and effective health system demands universal access and availability of good quality health care without financial burden, as well as the fair distribution of financial costs for the access and impartial distribution of the burden in rational care and capacity. Disease prevention and health promotion are pressing needs. Health insurance can definitely refine the health care system.
The public health system today has drawbacks of low quality care, corruption, dissatisfaction with the system, lack of accountability, unethical care, overcrowded clinics, poor cooperation between the public and private spheres, barriers to access health services and medicines, ignorance regarding public health, and low affordability [21,22]. Therefore, the wealthier Indians utilize the private health care system, which the low-income families cannot avail of, thus creating the inequality between the classes for medical treatment [23].
Currently, the private sector provides nearly 80% of outpatient and 60% of inpatient care [23]. The private-sector health care remains unaffordable for most Indians. As the prevailing weak regulatory systems have neither set nor enforced standards of quality and cost, many patients receive inadequate, inappropriate, or even unethical care. About 70% of the health care expenditures involve out of pocket spending, impoverishing many [23,24].
The perceived problems with the access, affordability, and quality of care have catalysed reforms over the past decade. Government has recognized that health is essential to economic development, and that country's healthy young population offers a demographic window of opportunity for accelerated economic growth. Moreover, the civil society organizations are advocating legislated “right to health”. The policy discourse on universal health coverage picked up momentum and prompted the government for transformation of healthcare.
‘The World Bank estimated that over 30 crore people, or above 25% of the population, had acquired at least some form of health insurance by 2010. Over 18 crore individuals of this group included people below the poverty line’. India’s public financing for health care is less than 1% of the world’s total health expenditure, although it supports over 17% of the global population. Families meet almost 70% of their health expenses out of pocket, a heavy burden on poor households, often forcing them deeper into poverty [25].
With general elections in India (to be held in April-May 2019) in mind, the present government has launched AB-NHPS as a goodwill measure.
Human development indicators
The per capita expenditure in India on health care is among lowest in the world, with the spending as low as INR 3 per day, per citizen [18,26]. The public health per capita per year costs the government INR 1,112, which is less than the cost of a single consultation at the country’s top private hospitals or approximately the cost of a single pizza (equal to INR 93 per month or INR 3 per day) [17].
The National Health Policy (NHP) 2017 reiterated that public health spending must be raised to 2.5% of the GDP by 2025, but India has not yet fulfilled even the 2010 target of spending 2%. Indians rank sixth in the low-middle income group of 50 nations, for out of pocket (OOP) health spending. These costs drive between 32 to 39 million Indians below the poverty line every year [20].
Without substantially raising in its health care budget, India will find it hard to achieve its health targets by 2025. India’s $16 (INR 1,112) per capita expenditure on health is the fourth lowest in South East Asia [20,27]. In terms of human development, population health is crucial for the economic growth and stability of any country. Good health involves disease control, balanced nutrition, and an efficient medical care system [28].
Globally, 100 million people are pushed into poverty every year because they have to pay directly for their health care. WHO recommends moving away from direct, out-of-pocket payments to using prepaid mechanisms to raise funds for health? ‘In 2011, US $ 6.9 trillion was spent on health. Typically, between 20–40% of health spending is wasted. A minimum of US$ 44 is needed per person per year to provide basic’ [29].
Catastrophic expenditure
Nearly 55 million Indians were driven to poverty in a single year because of having to pay for their own health care and 38 million of them dropped below the poverty line due to expenditure incurred for medicines alone. According to this study, non-communicable diseases like cancer, heart diseases and diabetes are responsible for the biggest slab of spending on health by the households called “catastrophic expenditure” [30]. Health expenditure is termed catastrophic if it consumes 10% or more of the overall household expenditure.
Responding to the Challenge
The NHPS has been launched to meet the challenge. It aims at providing coverage for hospitalization at the secondary and tertiary health care levels. The NHPS focuses on hospitalization (including pre- and post-hospitalization charges). However, most of the out of the pocket expenditure borne by the consumers goes towards the purchase of medicines (52%). Most often, these purchases are incurred for patients not requiring hospitalization [31].
The NHPS will provide a cover of INR 5,00,000 per family, per year, to about 10.7 crore families from poor and vulnerable populations. The insurance coverage is targeted for hospitalization at the secondary and tertiary health care levels.
Under the NHPS, four in ten Indians will be able to avail of secondary and tertiary care in government and private hospitals, within the insurance cap allotted per family. The NHPS will require an expenditure outlay of over $1,000 billion.
Besides the NHPS, the government plans to set up 150,000 Health and Wellness Centers under the Ayushman Bharat program, to provide treatment for non-communicable diseases and disburse primary care to young mothers and children. Free supply of essential medication and diagnostics is also in the pipeline.
The NHPS will cover nearly 1354 packages that have been finalized by the Health Ministry. Around 23 specialties from Cardiology to Oncology to Ophthalmology, Orthopedics and Urology, are cited for inclusion in this package. Some even include special treatment for complex diseases akin to cancer.
Impact and Implications
Certain treatments can produce an outcome which requires nearly INR 50,000. A total knee replacement surgery, for example, will cost INR 80,000 while a C-section will cost INR 9,000. Furthermore, the cost of a vertebral angioplasty with a single stent will cost INR 50,000 and the one involving a double stent will cost INR 65,000. The list includes even mental disorders and pediatric surgeries.
For a better picture of the costs, some prices that private hospitals may levy, is as follows: INR 1.5 lakh for a C-section, INR 1,500,000- 200,000 for angioplasty, and INR 3,500,000 for a total knee replacement surgery.
Private hospitals too will benefit. Those certified at an entry level by the National Accreditation Board for Hospitals & Health care Providers (NABH) will acquire 10% more, while those certified at an advanced level will receive an extra 15% as an incentive. Hospitals in the underdeveloped regions too will gain an extra 10%.
The poorest and the most vulnerable sections of the country will enjoy the benefit of increased coverage which actually extends to almost 40% of the population.
This scheme is expected to have major impact on reduction of Out of Pocket expenditure on ground of: increased benefit cover to nearly 40% of the population, (the poorest and the vulnerable), and covering almost all secondary and many tertiary hospitalizations.
AB-NHPS will lead to increased access to quality health and medication. In addition, the unmet needs of the population which remained hidden due to lack of financial resources will be catered to. It will also lead to timely treatments, improvements in health outcomes, patient satisfaction, improvement in productivity and efficiency, job creation thus leading to improvement in quality of life.
The threats include enrolment of ghost beneficiaries, impersonation in connivance with cardholders and hospital, conversion of OPD patient to IPD patient, deliberate blocking of higher priced package, treatment of diseases which a hospital is not equipped for, doctors performing unnecessary procedures, and hospitals charging fees even though it is a cashless scheme.
Financing NHPS
The Central and State Governments will share the total expenses accrued in the premium payment, according to the ratio specified by the trending guidelines of the Ministry of Finance
The total expenditure is dependent upon the actual marketdetermined premium paid in the States/UTs where the AB-NHPM will be implemented through the insurance companies [32].
Partnering with the NITI Aayog, a robust, modular, scalable and inter-operable IT Platform, which will involve a paperless and cashless transaction, will become operational.
In the States/UTs where the scheme will be implemented in a Trust/Society mode, the central share of funds will be supplied based on the actual expenditure or premium ceiling (whichever is lower) in the pre-fixed ratio [33].
All the public hospitals will be deemed empaneled under the scheme, while the private hospitals will be empaneled based on specific criteria. The Ministry of Health has set up a committee under the chairmanship of the Director General of Health Services which is in the process of finalizing the empanelment criteria for private hospitals [34].
The National Health Resource Repositor
The NHRR project is a map indicating the locations of approximately 2,000,000 to 2,500,000 health care facilities in the country, as well as details on their functioning, the number of patients they serve and performance of the doctors. The NHPS will depend on this mapping exercise for both implementation and monitoring.
National Health Stack
The aim of the NHS is to establish a centralized health record for all the citizens in India, and streamline the information on their health and facilitate effective management of the same.
The innovativeness of the NHS design proposed lies in its ability to leverage a shared public good by supporting a multitude of health verticals and their disparate branches - a visionary digital framework across the public and private sectors [35].
Employment generation
The AB-NHPM is expected to generate more than 100,000 ‘longterm’ skilled and semiskilled employment opportunities in the next four years, most of which will come from the anticipated expansion of private hospitals. Nearly 25,000 hospitals will be empaneled in the scheme to satisfy the health care service demands. Moreover, 80,00000 ‘short-term’ jobs will likely be created during the roll-out of the mission, for the construction of new hospitals and expansion of the existing ones.
By 2030, India will need 2.07 million doctors to reach a doctorpopulation ratio of 1:1,000. This implies a growth of 151% registered doctors in the country between 2010 and 2030, according to the study estimates. In fact, the ‘current ratio of practicing doctors to population is a mere 4.8 per 10,000. There are 14,379 government hospitals with 6,34,879 beds in the country. Rural areas have11,054 hospitals with 209,010 beds and the urban areas have 3,325 hospitals with 4,25,869 beds. As on March 2016, there are 1,55,069 sub centers, 25,354 Primary Health Centers and 5,510 Community Health Centers in India, providing care in rural areas [36].
To achieve the target of doctor-population ratio of 1:1000 an impeccable growth rate of the registered stock of doctors by 151% is essential, in the 20-year period from 2010. Given the rather insufficient growth rate of 14.41% achieved in the stock over a 5-year period between 2010 and 2014, the projected 151% appears to be an almost impossible target to achieve within the remaining 15-year period [37].
Health System Transformation
The NHPS may exert a transformative impact if it is effectively implemented in a coordinated manner. It is argued, if the NHPS, which primarily offers support to the clinical services like hospitalization, can help to fix the broken public health system prevalent in the country. Most health facilities experience a paucity of general practitioners and specialists. Massive galvanizing of the healthcare system including careful coordination with healthcare providers is the key to success. The opportunities for graft have to be addressed.
Current Issues & Future trends
Health care at its essential core is a public good. A good health care system needs more money as well as properly trained health professionals and good hospitals and clinics. Establishing more primary health facilities, distributed evenly throughout the country and within the reach of low-income families, are vital. Focus on health services research is critical. Health education must reach the out-ofreach. Medical education needs to be revamped to produce the doctors of the twenty-first century.
Health is a significant issue in justice. Politics must actively engage in health care. Zero tolerance for corruption must be ensured. Poverty should be eradicated. The management of the health care delivery system should be professionalized and strengthened. The private sector should be regulated and its role clearly defined. A sound and dependable referral system is crucial.
Conclusion
Launching of NHPS is a step in the right direction. Its success will depend on how well the plan is defined and implemented on the ground level. Primary care has to make affordable and accessible to all. It will improve the wellness of the population and reduce the overall cost to the exchequer. Innovations in health are needed to improve affordability and access. The published procedure pricing may pose a hindrance in efficiently executing the scheme. Management of the revenue cycle will be another test of their ability. The pricing mechanism must be reviewed to be reasonable for all the parties concerned, a vital necessity for providing quality care and better coverage. India requires an integrated approach to reach out to the whole population and train the various service segments providing them.
REFERENCES
- https://www.healthdata.org/sites/default/files/files/policy_report/2017/India_Health_of_the_Nation%27s_States_Report_2017.pdf
- Three infants die every two minutes in India: UNIGME. Times of India.
- Diabetes is India's fastest growing disease: 72 million cases recorded in 2017, figure expected to nearly double by 2025.
- Ladusingh L, Mohanty SK, Thangjam M. Triple burden of disease and out of pocket healthcare expenditure of women in India. PLoS ONE. 2018;13:e0196835.
- Pascal G, Jennifer MG, Michaela T, Justine ID, Ashish A, et al. Geographic and sociodemographic variation of cardiovascular disease risk in India: A cross-sectional study of 797,540 adults. PLoS Med. 2018;15:e1002581.
- Simon IH. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1260-1344.
- World Population Prospects: The 2017 Revision.
- The World Population Prospects: 2015 Revision.
- 2014 revision of the World Urbanization Prospects.
- https://data.worldbank.org/country/india?view=chart.
- http://ghdx.healthdata.org/gbd-results-tool
- Jaspers L, Colpani V, Chaker L, Muka T, Imo D, Shanthi M, et al. The global impact of non-communicable diseases on households and impoverishment: A systematic review. Eur J Epidemiol. 2015;30(3):163-188.
- Bloom DE, Candeias V, Adashi E, Bloom L, Gurfein L, Jane-Llopis Eet al. Economics of non-communicable diseases in India. World Economic Forum. 2014.
- https://www.un.org/sustainabledevelopment/health/
- http://www.newindianexpress.com/lifestyle/health/2018/jul/15/deaths-from-cardiovascular-disease-rising-in-india-study-1843701.html
- The changing patterns of cardiovascular diseases and their risk factors in the states of India: The Global Burden of Disease Study 1990-2016.
- India Guide. Population of India 2018.
- https://www.firstpost.com/india/indias-per-capita-expenditure-on-healthcare-among-lowest-in-the-world-govt-spends-as-little-as-rs-3-per-day-on-each-citizen-4559761.html
- World Health Organization. The world medicines situation Report. 2004.
- Anurag B, Kalantri SP. The crisis in access to essential medicines in India: Key issues which call for action. IJME. 2013;10(2):86-95.
- Twelfth Five Year Plan. Social Sectors. 2012.
- Hammer J, Aiyar Y, Samji S. Understanding Government Failure in Public Health Services. Economic and Political Weekly. 2017;42(40):4049-4057.
- Srinath Reddy K. India's Aspirations for Universal Health Coverage. N Engl J Med. 2015;373:1-5.
- Reddy KS, Patel V, Jha P, Paul VK, Kumar AKS, Dandona L, et alet al. Towards achievement of universal healthcare in India by 2020: A call to action. Lancet. 2011;377(9767):760-768.
- Gerard LF, Somil N. Government-Sponsored Health Insurance in India: Are You Covered. The World Bank. 2012.
- World Health Organization. The world medicines situation. 2004.
- http://www.cbhidghs.nic.in/WriteReadData/l892s/Before%20Chapter1.pdf
- Sinha DK. Health and Human Development Indicators in India.
- World Health organization. World Global Health Expenditure Atlas. 2004.
- Rema N. Politic and Nation. Health spending pushed 55 million into poverty in a year: Study. The Economic Times. 2018.
- https://thewire.in/health/who-is-paying-for-indias-healthcare
- http://ayushmanbharat.net
- Ayushman Bharat National Health Protection Mission.
- https://www.livemint.com/Politics/YHWz7EjkrDKVE6j3wkUxUM/Govt-is-committed-to-take-public-expenditure-on-healthcare.html
- National Health Stack: Strategy and Approach.
- http://dghs.gov.in/content/1370_1_cbhi.aspx
- Potnuru B. Aggregate availability of Doctors in India: 2014-2030. Indian J Public Health. 2017;61:182-187.
Citation: Tabish SA (2019) Health Reform as Political Instrument: Achieving Universal Health Coverage. Health Care Current Reviews 7:239. doi: 10.35248/2375-4273.19.07.239.
Copyright: © 2019 Tabish SA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.