PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 0, Issue 0
Granulomatous Mastitis: Is it Boon or Bane??
Satish Chaitanya K*, Prateek Sharda, Ananya Deori, Anamika Kumar, Manju Verma, Anjum Syed and Bina RaviReceived: 11-Jun-2021 Published: 01-Jul-2021, DOI: 10.35248/2329-8847.21.s6.002
Abstract
Introduction: Granulomatous mastitis (GM) is a rare benign breast disease subdivided into idiopathic and specific. The clinical and imaging diagnosis is often challenging as it can mimic malignancy. It has characteristic histological features of multinucleated giant cells, non-caseating granulomas, and necrosis. The treatment is still controversial with steroid therapy as a primary modality and surgery are avoided due to fistula formation and recurrences.
Aims and objectives: This study aims to establish the descriptive features of granulomatous mastitis and the correlation between various risk factors affecting and leading to the recurrence of the disease.
Materials and methods: This was a retrospective study carried out for a period of 12 months at IBCC (Integrated Breast Care Centre) established in AIIMS, Rishikesh, Uttarakhand. Out of 2567 patients who presented to OPD, 34 patients were diagnosed with granulomatous mastitis included in this study.
Results: Of all the 34 patients who presented with granulomatous mastitis, the mean age 38.32 yrs, all of them are females (100%) with a mean duration of 2.55 months. Breast lump noted in 82.4%, 85.3% with Pain, 17.6% had Discharge. On examination, the mean largest size is 3.41 ± 1.15 cm, 67.6% had Tenderness. We observed statistical significance (P<0.05) between pathological features, giant cells, AFB positivity, antibiotics, steroid, and antituberculosis treatment with recurrence.
Conclusion: Granulomatous mastitis is a special disease scenario that will mimic malignancy but have low rates of transformation but it has more financial burden on patients due to its chronicity resulting in poor quality of life which is a Boon and Bane for these patients.
Keywords
Granulomatous mastitis; Benign breast; Diseases and disorders; Breast carcinoma
Introduction
“Granulomatous mastitis (GM) is a rare benign breast disease first described in the literature by Kessler and Wolloch” [1]. It has mainly two subtypes Idiopathic (IGM) and Specific Granulomatous Mastitis (SGM). Idiopathic Granulomatous Mastitis (IGM) is a chronic inflammatory condition of the breast with unknown etiology, seen more commonly in women of childbearing age [2-5]. Specific Granulomatous Mastitis (SGM) is a rare secondary complication of tuberculosis, syphilis, Wegener's granulomatosis, sarcoidosis, corynebacterial infection, vasculitis, fungal and parasitic infections, foreign body reaction, etc [2-4]. The clinical and imaging diagnosis of this benign condition is often challenging as it can simulate many other conditions including malignancy.
The etiology of granulomatous mastitis includes autoimmunity, hyperprolactinemia, oral contraceptives, pregnancy and lactation, smoking, alpha 1 antitrypsin deficiency, and trauma. The most common clinical symptoms include erythema, edema, palpable unilateral/bilateral breast mass, nipple retraction, discharge, ulceration, and axillary lymphadenopathy. However, patients may also have more bizarre presentations, mainly in their subclinical forms.
The diagnosis is mainly by characteristic histological features showing multinucleated giant cells, non-caseating granulomas, and necrosis as in Figure 1. The treatment of this disease remains controversial. Medical management by antibiotics, NSAIDs, and corticosteroid therapy has been used as a primary modality. Surgical intervention should be avoided, if possible due to its autoimmune nature and high rates of complications, including recurrence and fistulas. Accurate diagnosis of this disease is essential as patients are highly concerned about the nature of diseases like malignancy.
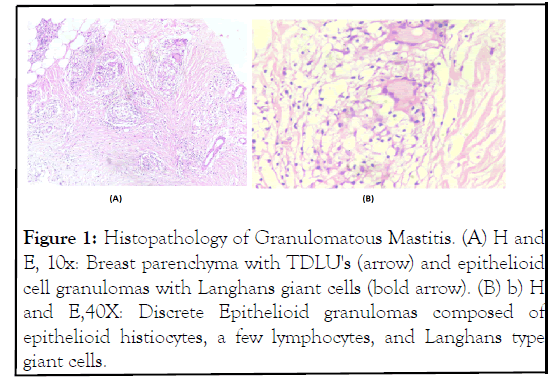
Figure 1: Histopathology of Granulomatous Mastitis. (A) H and E, 10x: Breast parenchyma with TDLU's (arrow) and epithelioid cell granulomas with Langhans giant cells (bold arrow). (B) b) H and E,40X: Discrete Epithelioid granulomas composed of epithelioid histiocytes, a few lymphocytes, and Langhans type giant cells.
The present study aims to establish the descriptive features of granulomatous mastitis and correlation between various risk factors affecting and leading to recurrence of granulomatous mastitis particularly in the Indian population so that we can avoid or treat those factors for better management of this disease and reduce the psychological and financial burden to the patients.
Materials and Methods
This was a retrospective observational study conducted from September 2018 to August 2019 for 1 year in the Integrated Breast Care Centre (IBCC) established exclusively for patients related to breast diseases at AIIMS, Rishikesh in September 2018 in collaboration with other departments like Breast Imaging, Onco-Pathology and Radiation Oncology.
In these 12 months, a total of around 2567 patients were presented with various complaints related to breast, out of which 34 patients were presented with complaints related to granulomatous mastitis and have undergone further investigations to confirm the same. Inclusion criteria are all those patients who had a previous history of granulomatous mastitis and pathological diagnosis as granulomatous mastitis regardless of age. Exclusion criteria include patients who have not given consent for this study, those who have refused to undergo further assessment, and those who had lost their follow-up.
The patients included in this study presented to our OPD with various complaints regarding breast for which Triple assessment (Clinical, Radiological and Pathological assessment), Microbiological testing like CBNAAT, AFB, Pus for culture and sensitivity are done for further diagnosis and management. On confirmation of the diagnosis of granulomatous mastitis, all these patients were subjected to medical management (steroids) as an initial modality of choice, and others include antibiotics, NSIAD's, anti-tuberculosis therapy based on microbiological reports. Steroid therapy is the main mode of treatment for these cases in our institute with dosage starts with 25 mg single day for about 21 days tapered regularly based on clinical response till adequate response noted. The minimum duration of this treatment is around 2 to 3 months. These patients are on regular monthly follow up with ultrasonograms of the breast for response assessment and those non responded, progressive cases are subjected to surgical management for excisional biopsy of nodularity or fistulous tracks for establishing the diagnosis. These patients were followed up for 6 months duration for identifying the recurrence of the disease process.
Statistical analysis
Fisher's exact test was used to explore the association between 'Recurrence' and 'Pathology' as more than 20% of the total number of cells had an expected count of less than 5. A p-value of <0.05 is taken as statistically significant for this study.
Results
In these 12 months, a total of around 2567 patients were presented with various complaints related to breast, out of which 34 patients were diagnosed as granulomatous mastitis.
Of all the 34 patients who presented with granulomatous mastitis, the mean age (Years) was 38.32 ± 14.76, all of the 34 (100.0%) participants are female. The mean Duration of Illness was 2.55 ± 6.47 months. The presenting complaint is lump breast in 8 (82.4%) of the participants (Figure 2), 29(85.3%) had Pain, 6(17.6%) had Discharge, 2(5.9%) had Retracted Nipple, 5(14.7%) had Redness. The mean Largest Dimension of the Lump is around 3.41 ± 1.15 cm (Figure 2).
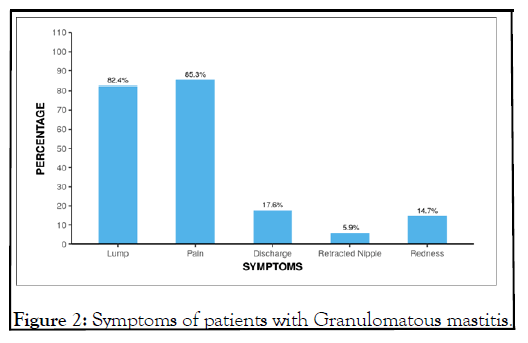
Figure 2: Symptoms of patients with Granulomatous mastitis.
History of a breast abscess is in about 6(17.6%) patients, 4(11.8%) had Granulomatous Mastitis, 1(2.9%) had a history of lactation, 1(2.9%) Lumpectomy, 1(2.9%) had Lumpectomy + Tuberculosis, 4(11.8%) had Tuberculosis and 17(50.0%) of the participants had no significant history. 14(41.2%) of the participants had right side and 17(50.0%) had left and 3(8.8%) had Bilateral disease. On clinical examination 23(67.6%) of the participants had Tenderness, 3s(8.8%) are Firm inconsistency, 5(14.7%) had Nodularity. 3(8.8%) had an Inverted Nipple, 1(2.9%) had Nipple Discharge. 16(48.5%) of the participants had Axillary lymphadenopathy.
Discussion
Granulomatous mastitis (GM) is a rare benign breast disease entity, however, the diagnosis for assessment and treatment of this condition is not easy in every case [6-15]. It generally affects young women aged between 20-40yr in their reproductive age groups [16] as in Figure 1. The pathophysiology of this disease is not clearly understood but there are some studies conducted observed that the association between oral contraceptive intake, infectious processes, and autoimmunity [17].
Although the etiological factors of GM have not been clearly defined, some factors are believed to be associated with autoimmune diseases, undetected microorganisms, hyperprolactinemia, diabetes, and oral contraceptive use [18]. In addition to the clinical characteristics of the disease, defining the relation of epidemiological factors with IGM may be important in the prevention of this disease.
In the literature, the longest study was done by Al Khaffaf, et al. with 133 patients diagnosed and treated for 25 years [7]. In another study, Hee RNS, et al. reviewed 58 patients with IGM and 10 patients with TM in 10 years [8]. Peyvandi, et al. reported 54 patients, and Kok, et al. reported 43 patients with GM [9,10]. The sample size included in those studies is similar to in our study (n=34). For example, Erözgen, et al. reported 33 patients with GM, 25 with IGM, and 8 with TM [11]. Akyıldız, et al. reported 30 patients, Aksoy, et al. reported 19 patients and Gürleyik, et al. reported 19 patients with GM [12-14]. In our study, we included 34 patients with granulomatous mastitis (GM) over 12 months. This study mainly deals with a descriptive analysis of all 34 cases of granulomatous mastitis and its correlation to various risk factors like age, duration of complaint, radiological grading, microbiological and pathological analysis, and other features (fistula, necrosis, Gaint cells) and finally multimodality management with recurrence (Table 1).
| Parameters | Recurrence | p-value | |
|---|---|---|---|
| Present (n=23) | Absent (n=11) | ||
| Past history | 0.1642 | ||
| Breast abscess | 5 (21.7%) | 1 (9.1%) | |
| Granulomatous mastitis | 4 (17.4%) | 0 (0.0%) | |
| Imaging | <0.0012 | ||
| BIRADS 3 | 2 (8.7%) | 8 (72.7%) | |
| BIRADS 4 | 2 (8.7%) | 0 (0.0%) | |
| BIRADS 4a | 19 (82.6%) | 2 (18.2%) | |
| BIRADS 4c | 0 (0.0%) | 1 (9.1%) | |
| Pathology | <0.0012 | ||
| Chronic inflammation | 0 (0.0%) | 6 (54.5%) | |
| Granulomatous mastitis | 21 (91.3%) | 1 (9.1%) | |
| Giant cells (Present) | 15 (65.2%) | 2 (18.2%) | 0.0103 |
| Tuberculosis (Present) | 5 (21.7%) | 0 (0.0%) | 0.1502 |
| Fistula (Present) | 11 (47.8%) | 3 (27.3%) | 0.2952 |
| CBNAAT (Positive) | 8 (34.8%) | 0 (0.0%) | 0.0342 |
| AFB (Positive) | 8 (34.8%) | 0 (0.0%) | 0.0342 |
| Steroids | <0.0012 | ||
| Received | 23 (100.0%) | 1 (9.1%) | |
| Not received | 0 (0.0%) | 10 (90.9%) | |
| NSAIDs | <0.0012 | ||
| Received | 9 (39.1%) | 11 (100.0%) | |
| Not received | 14 (60.9%) | 0 (0.0%) | |
| ATT | 0.0342 | ||
| Received | 8 (34.8%) | 0 (0.0%) | |
| Not received | 15 (65.2%) | 11 (100.0%) | |
| Antibiotics | <0.0012 | ||
| Received | 9 (39.1%) | 11 (100.0%) | |
| Not received | 14 (60.9%) | 0 (0.0%) | |
Table 1: Parameters associated with recurrence of Granulomatous mastitis.
In literature, studies have reported an association between ethnic origin and geographic region on the disease prevalence [19,20]. The prevalence of granulomatous mastitis has been reported to be high in Turkey, Asia, and Far Eastern countries [21-24]. Granulomatous mastitis affects young reproductive women aged between 17 and 42 years but it may even affect advanced ages such as 65 or 83yrs [25,26]. The mean age observed in our study was 38.32 ± 14.76 yrs (Mean ± SD) comparable with the studies in the literature [22,25]. In a study report, no significant difference was noted between the recurrence and nonrecurrence groups according to the mean age similar to our study [27].
Fine Needle Aspiration Cytology (FNAC) has low sensitivity and specificity for the diagnosis of granulomatous mastitis. A core needle/open biopsy is routinely recommended for an accurate diagnosis [15]. In our series, the diagnosis of all patients was proven histologically by the examination of core biopsy specimens. Idiopathic granulomatous mastitis (IGM) is diagnosed only after excluding infectious (tuberculosis/fungal) and non-infectious (sarcoidosis/vasculitis) causes with the presence of non-calcified granulomas on histological sections. In our study, we included both idiopathic and secondary granulomatous mastitis.
In some studies, they reported a significant relationship between microbiological agents and granulomatous mastitis. In our study, infections observed in the patients were noted in history, and in some cases, they were observed at the time of the diagnosis of GM. In patients with a history of systemic bacterial infection, a significant relationship was observed between the GM recurrence and systemic bacterial infection as well (Figure 3).
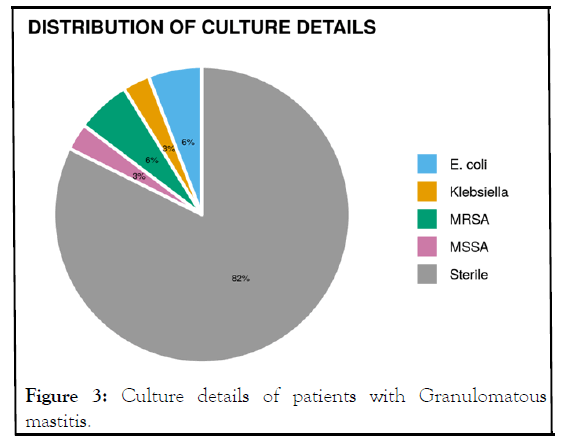
Figure 3: Culture details of patients with Granulomatous mastitis.
There is no clear consensus regarding the management protocol of granulomatous mastitis which is still unclear. Pathological confirmation with the exclusion of other causes including malignancy is important for decision making and preventing inappropriate treatments. The treatment choice and sequence of this disease are still debated. Currently, there is no universally accepted treatment protocol [28], corticosteroids and antibiotics are frequently used agents in medical management. However, successful results have been reported with some agents, such as methotrexate, azathioprine, glucocorticoids, bromocriptine, and colchicine or in combination with steroids [29,30]. The recurrence despite immunosuppressive therapy noted in some patients with GM has not rendered autoimmunity alone to be responsible in the etiology [28]. Surgical resection is to be avoided given high complications and some studies reported increased recurrence rates with broad surgical resection while some other studies reported lower recurrence rates [31]. In literature, the lifetime risk of malignancy in granulomatous mastitis is very low and none of the cases is biopsy-proven malignant in our study (0%) but some cases presented with features mimicking carcinoma [32] (Figure 4).
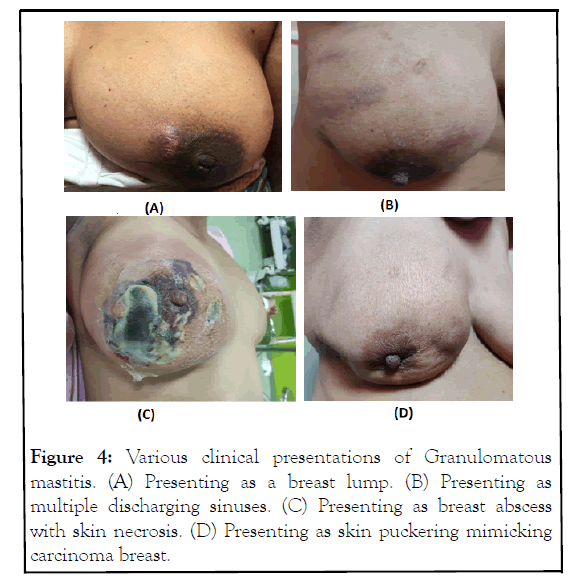
Figure 4: Various clinical presentations of Granulomatous mastitis. (A) Presenting as a breast lump. (B) Presenting as multiple discharging sinuses. (C) Presenting as breast abscess with skin necrosis. (D) Presenting as skin puckering mimicking carcinoma breast.
All these factors subject the patients to poor quality of life, psychological depression, and financial burden on patient's leading to loss of follow up which is the main problem encountered particularly in the Indian rural population. We observed a statistically significant correlation of recurrence (P<0.05) with factors like Pathological features (Chronic Granulomatous Inflammation, Granulomatous Mastitis, and Necrotising Granulomatous Mastitis), presence of giant cells, AFB positivity, h/o of NSAIDs, Antibiotic, Steroid, and antituberculosis treatment received.
The limitations in this study are the short follow-up duration of patients (longer follow-up is needed to establish actual recurrence rates), we included both idiopathic and specific subtypes of granulomatous mastitis which differs in etiological factors influencing recurrence rates and retrospective data collection is another limitation of our study.
Conclusion
In conclusion, Granulomatous mastitis is a special disease scenario that will clinically mimic many other diseases including malignancy but have low rates of malignant transformation but on another side of the disease spectrum, there is the poor quality of life for patients with the financial burden, with psychological depression for this chronic disease pattern which is a Boon and Bane for the patient.
REFERENCES
- Kessler E, Wolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol. 1972;58(6): 642-646.
- Diesing D, Axt-Fliedner R, Hornung D, Weiss JM, Diedrich K, Friedrich M. Granulomatous mastitis. Arch Gynecol Obstet. 2004;269(4): 233-236.
- Tse GM, Poon CS, Ramachandram K, Ma TKF, Pang L, Law BKB, et al. Granulomatous mastitis: A clinicopathological review of 26 cases. Pathology. 2004;36(3): 254-257.
- Panzacchi R, Gallo C, Fois F, Dalpiaz G, Cucchi MC, Esposti RD, et al. Primary sarcoidosis of the breast: case description and review of the literature. Pathologica. 2010;102(3): 104-107.
- Cserni G, Szajki K. Granulomatous lobular mastitis following drug-induced galactorrhea and blunt trauma. Breast J. 1999;5(6): 398-403.
- Bani-Hani KE, Yaghan RJ, Matalka II, Shatnawi NJ. Idiopathic granulomatous mastitis: Time to avoid unnecessary mastectomies. Breast J. 2004;10(4): 318-322.
- Al-Khaffaf B, Knox F, Bundred NJ. Idiopathic granulomatous mastitis: A 25-year experience. J Am Coll Surg. 2008;206(2): 267-273.
- Hee RNS, Kuk YN, Hyun EY, Kim TH, Kang DK, Oh KK, et al. Differential diagnosis in idiopathic granulomatous mastitis and tuberculous mastitis. J Breast Cancer. 2012;15(1): 111-118.
- Larsen LJH, Peyvandi LB, Klpfel N, Grant E, Lyengar G. Granulomatous lobular mastitis: Imaging, diagnosis, and treatment. AJR. 2009;193(2): 574-581.
- Kok KY, Telisinghe PU. Granulomatous mastitis: Presentation, treatment, and outcome in 43 patients. Surgeon. 2010;8(4): 197-201.
- Erözgen F, Ersoy YE, Akaydın M, Memmi N, Ceik AS, Celebi F, et al. Corticosteroid treatment and timing of surgery in idiopathic granulomatous mastitis confusing with breast carcinoma. Breast Cancer Res Treat. 2010;123(2): 447-452.
- Akyıldız EÜ, Aydoğan F, İlvan Ş, Calay Z. İdiopathic granulomatous mastitis. J Breast Health. 2010;6: 5-8.
- Aksoy Ş, Aren A, Karagöz B. Granülomatöz mastit ve cerrahi tedavi. İstanbul Tıp Dergisi. 2010;11: 164-167.
- Gürleyik G, Aktekin A, Aker F, Karagülle H, Sağlam A. Surgical treatment of idiopathic granulomatous lobulşar mastitis. J Breast Cancer. 2012;15(1): 119-123.
- Gürleyik G, Aktekin A, Aker F, Karagülle H, Sağlam A. Medical and surgical treatment of ıdiopathic granulomatous lobular mastitis: a benign ınflammatory disease mimicking ınvasive carcinoma. J Breast Cancer. 2012;15(1): 119-123.
- Kessler E, Wolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol. 1972;58(6): 642-646.
- Bani-Hani KE, Yaghan RJ, Matalka II, Shatnawi NJ. Idiopathic granulomatous mastitis: time to avoid unnecessary mastectomies. Breast J. 2004;10(4): 318-322.
- Altintoprak F, Kivilcim T, Ozkan OV. Etiology of idiopathic granulomatous mastitis. World J Clin. Cases 2014;2(12): 852-858.
- Centers for Disease Control and Prevention (CDC). Idiopathic granulomatous mastitis in Hispanic women – Indiana, 2006–2008. MMWR Morb Mortal Wkly Rep. 2009;58: 1317-1321.
- Pandey TS, Mackinnon JC, Bressler L, Millar A, Marcus EE, Ganschow PS. Idiopathic granulomatous mastitis – a prospective study of 49 women and treatment outcomes with steroid therapy. Breast J. 2014;20(3): 258-266.
- Akcan A, Oz AB, Dogan S, Akgun H, Akyuz M, Ok E, et al. Idiopathic granulomatous mastitis: comparison of wide local excision with or without corticosteroid therapy. Breast Care (Basel). 2014;9(2): 111-115.
- Karanlik H, Ozgur I, Simsek S, Fathalizadeh A, Tukenmez M, Sahin D, et al. Can steroids plus surgery become the first-line treatment of idiopathic granulomatous mastitis? Breast Care (Basel). 2014;9(5): 338-342.
- Korkut E, Akcay MN, Karadeniz E, Subasi ID, Gursan N. Granulomatous mastitis: a ten-year experience at a University Hospital. Eurasian J Med. 2015;47: 165-173.
- Baslaim MM, Khayat HA, Al-Amoudi SA. Idiopathic granulomatous mastitis: a heterogeneous disease with variable clinical presentation. World J Surg. 2007;31(8): 1677-1681.
- Aghajanzadeh M, Hassanzadeh R, Alizadeh Sefat S, Alavi A, Hemmati H, Delshad MSE, et al. Granulomatous mastitis: presentations, diagnosis, treatment, and outcome in 206 patients from the north of Iran. Breast. 2015;24(4): 456-460.
- Lai EC, Chan WC, Ma TK, Tang AP, Poon CS, Leong HT. The role of conservative treatment in idiopathic granulomatous mastitis. Breast J. 2005;11(6): 454-456.
- Omranipour R, Mohammadi SF, Samimi P. Idiopathic granulomatous lobular mastitis – report of 43 cases from Iran; introducing a preliminary clinical practice guideline. Breast Care (Basel). 2013;8(6): 439-443.
- Akcan A, Oz AB, Dogan S, Akgun H, Akyuz, Ok E, Gok M, et al. Idiopathic granulomatous mastitis: comparison of wide local excision with or without corticosteroid therapy. Breast Care (Basel). 2014;9(2): 111-115.
- Néel A, Hello M, Cottereau A, Faucal P, Costedoat-Chaimeau N, Rondeau-Lutz M, et al. Long-term outcome in idiopathic granulomatous mastitis: a western multicentre study. QJM. 2013;106(5): 433-441.
- Akbulut S, Yilmaz D, Bakir S. Methotrexate in the management of idiopathic granulomatous mastitis: a review of 108 published cases and report of four cases. Breast J. 2011;17(6): 661-68.
- Bani-Hani KE, Yaghan RJ, Matalka II, Shatnawi NJ. Idiopathic granulomatous mastitis: time to avoid unnecessary mastectomies. Breast J. 2004;10(4): 318-322.
- Altintoprak F, Kivilcim T, Yalkin O, Uzunoglu Y, Kahyaoglu Z, Dilek ON. Topical steroids are effective in the treatment of idiopathic granulomatous mastitis. World J Surg. 2015;39(11): 2718-2723.
Citation: Chaitanya KS, Sharda P, Deori A, Anamika K, Manju V, Syed A, et al. (2021) Granulomatous Mastitis: Is it Boon or Bane? J Aging Sci. S6: 002.
Copyright: © 2021 Chaitanya KS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.