PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
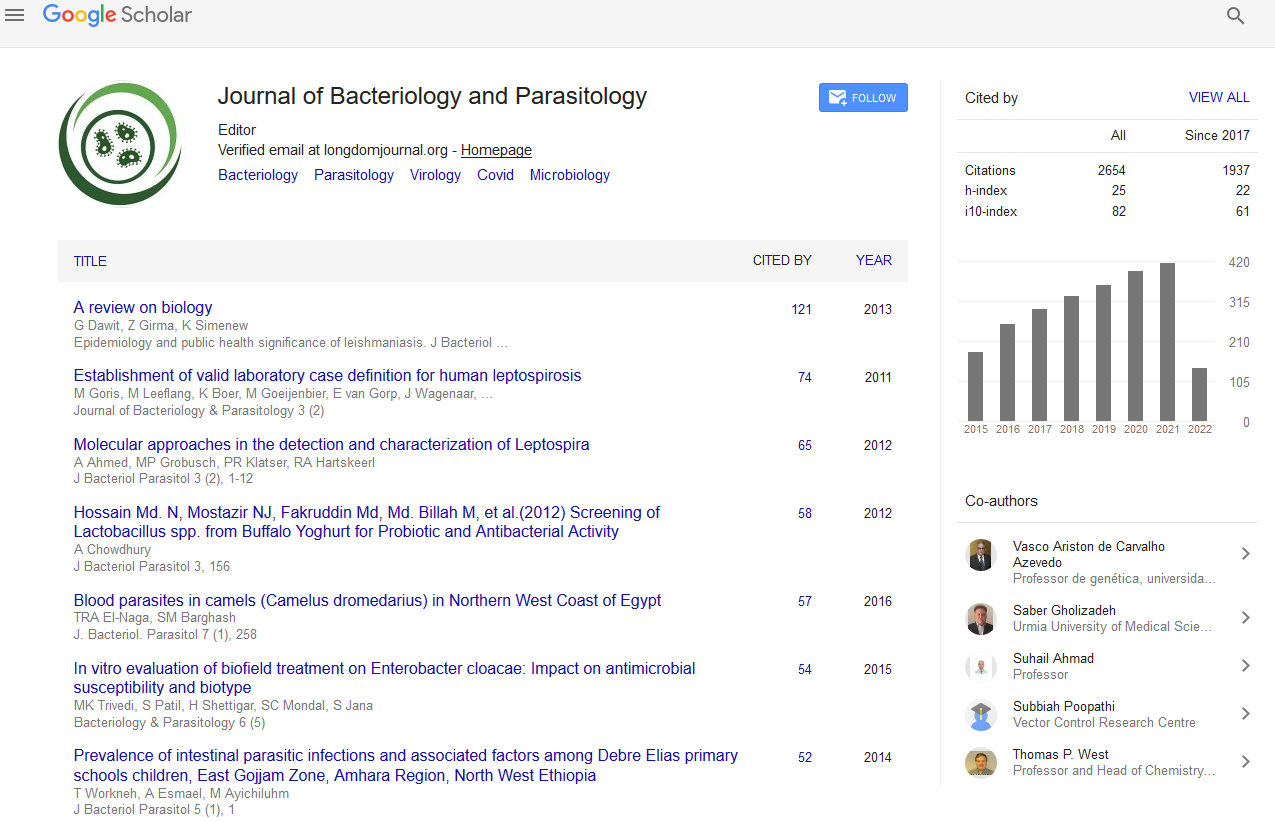
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2019) Volume 10, Issue 5
Fatal Invasive Trichosporonosis Caused by Trichosporon inkin after Allogeneic Stem Cell Transplant for very Severe Idiopathic Aplastic Anemia
Daphné Krzisch1, Vincent Camus1, Marion David2, Gilles Gargala3 and Stéphane Lepretre1*2Laboratory of Microbiology, Centre Henri Becquerel, Rouen, France
3Laboratory of Parasitology-Mycology, CHU de Rouen, Charles Nicolle Hospital, Rouen, France
Received: 01-Nov-2019 Published: 25-Nov-2019
Abstract
Invasive Trichosporon inkin fungal infections are rare and unusual, occurring nearly exclusively in immunocompromised patients experiencing prolonged neutropenia during treatment of malignant hemopathies or other immunodeficiency conditions. We report a case of a 27-year-old patient with severe aplastic anemia who developed Trichosporon inkin sepsis with skin lesions during aplasia after myeloablative allogeneic stem cell transplant. He was treated with liposomal amphotericin B but died from multiple organ failure. We then discuss the epidemiological, clinical and therapeutic features of these serious fungal infections compared to the published data.
Keywords
Trichosporon inkin; Aplastic anemia; Invasive fungal infection; Trichosporonosis; Hemopathy; Immunodeficiency; Antifungal therapy basidiomycetes
Introduction
Fungal infections are an important cause of death in immunocompromised patients, and particularly with hematologic disease. The most common fungal infections are invasive aspergillosis and invasive candidiasis [1,2] but mucormycosis are one of the most dreaded disease. Here, we want to approach about Trichosporoniose, least well-known, but which have devastating effects. Currently, no standard recommendations for Trichosporon spp antifungal prophylaxis and treatment exist.
Clinical Evolution
We report medical history of a 27 years old man of Turkish origin with no relevant medical history, who has been admitted to our haematology unit for a severe idiopathic aplastic anemia, according to standard diagnostic and severity criteria [3-5], (Thrombopenia 6 Giga/L; Hb 12 g/dL, Reticulocyte 12 G/L–bone marrow hypocellularity<15%, absolute neutrophile count 1.3 G/L).
An induction by cyclosporine 2 mg/kg twice daily associated with daily granulocyte colony-stimulating factors (lenograstim, G-CSF) is started, but the course has been unfavourable, with a persistance of medullary depression and quick appearance of very severe aplastic anemia criteria: Hb 8 g/dL, reticulocytes 3 G/L, platelets 20 G/L, absolute neutrophil count 0 G/L) on October 2012.
The patient presented with fever and development of herpetic gingivostomatisis. The patient’s room was located in the leukaemia unit and was a positive pressure ventilation clean room. The explorations fund no documentation. The patient was treated with broad spectrum antibiotherapy (piperacillin/tazobactam) with absence of bacteriological documentation.
At day 14, an anal cellulitis appeared with perineal pains and persistence of fever. The evolution is complicated with several bacteraemia documented with Stenotrophomonas maltophilia and Staphylococcus epidermidis Meticilline-resistant. Unfortunately, there was no possibility of surgical management of this perineal cellulitis, nore surgical indication, because of the thrombocytopenia and uncollected skin damage. The patient received different antiinfectious therapies (Figure 1).

Figure 1. Response of Antibiotics, Antiviral, Antifungal drugs with respective of time and dose.
At day 18, the patient presented a pneumonitis characterised by an interstitial syndrome. Because of a suspicious positive aspergillosis antigenemy we treated the patient by VORICONAZOLE 4 mg/ kg twice a day switched for CASPOFUNGINE 50 mg per day (hepatitis toxicity), No broncho-alveolar lavage was performed at this time. The evolution was favourable under this treatment.
Because of persistent medullary abnormalities and multiple infectious complications, an pheno-identical 10/10 allogeneic stem cell transplant was performed 20 days after the initial ciclosporin-based therapy; the conditioning was non-myeloablative, with Cyclophosphamide 300 mg/m2/d and horse anti-thymocyte globulin 40 mg per kg per day.
At day 20, the patient has presented a new infectious pneumonitis, characterized by bilateral interstitial and micro nodular infiltrates and an apical predominance. The broncho-alveolar lavage revealed a small lymphocytosis, and the bacteriological and mycological cultures remained negative. The CASPOFUNGINE was switched to VORICONAZOLE 4 mg/kg twice a day (after loading dose 6 mg/kg twice a day once) in ad of the antibiotics.
Then, at day 43, the patients developed skin nodules on the left foot, then an extension until the left thigh. At this time, the patient benefited from a large anti-infectious therapy (Figure 1). The multiple positivity of samples proved the disseminated Trichosporiniose: The skin biopsy fund a fibrinous necrosis associated with histiocytes and septate and budding fungal structures, arguments for alternariose or trichosporiniose. One blood culture (at day 66) was positive to Trichosporon inkin, which was identified by mass spectrometry (MALDI-TOF), as well as an anal sample. The transthoracic echography did not find argument for endocarditis or myocarditis. We added AMBISOME 3 mg/kg/ day to VORICONAZOLE at day 52 to broaden the spectrum and used in dual therapy.
Alternatively, the patient developed a CMV viremia, probably due to a reactivation (positive CMV serologic status of the recipient). It was treated in the first place by GANCICLOVIR 10 mg/kg twice a day, switched by Foscavir because of the persistence of the significant viral load. Before the transplant, the initial CMV serologic status for CMV the recipient was positive, which allowed a negotiation of the viremia.
At the day 80, the patient was transferred in medical reanimation for an acute respiratory distress syndrome, in relation with an acute cardiac deficiency due to a myocarditis. The viral aetiology was excluded because of the decrease of the CMV viral load. The privileged hypothesis was fungal, and potentially due to Trichosporon, because of the disseminated character, the cardiac tropism and the slowly good evolution under treatment. The patient went out of aplasia at day 110.
In front of the favourable evolution and because of persistent fever, the antibiotic and antifungal drugs, except FOSCAVIR (decreased viral load) were stopped in order to make new infectious samples. Unfortunately, the patient developed a febrile pancytopenia, without argument for a macrophage activation syndrome, and a skin rash. No microbiological documentation was found. Antibiotics PIPERACILLINE-TAZOBACTAM 4 g four times a day VANCOMYCINE 30 mg/kg in continuous and AMIKACINE are reintroduced. The new skin biopsy was in favour of a drug eruption. The VANCOMYCINE is switched by DAPTOMYCINE 4 mg/kg once a day, without improvement of the skin. The thoracic tomography showed an aggravation of pulmonary lesions, with an excavation. The patient died for a new acute respiratory distress due to an acute cardiac insufficiency, and multivisceral organ failure.
Discussion
This case shows the diagnostic difficulties of this infection and it gravity. Although a large anti-infectious therapy, the therapeutic stain ineffective. There is no consensus on the treatment of this.
Invasive fungal infections caused by Trichosporon spp are a deadly disease, with death rates of up to 80% in immunocomprised patients [6,7].
Trichosporon species are the causative agents of cutaneous infections like white piedra or hypersensitivity pneumonitis syndrome in immunocompetent patients, but they can be involved in invasive mycoses in immunodeficient patients, like haematological malignancies or solid tumours or AIDS [6-9].
Trichosporon asahii appears to be much more common in cases of systemic mycosis, while other Trichosporon species are involved in superficial skin lesions [6,7]. Ramos et al. study shows a high fungal burden in kidneys with T.asteroides than T.asahii that is in agreement with this observation [10]. However; Trichosporon inkin is the common agent of superficial trichosporonosis. But in rare cases of systemic disease, it can be isolated, and in this case, is associated with catheter infections [1,2,6,7].
1,3-Beta-D-glucan is a polysaccharide component specific to fungal cell wall. The assays have been reported to be useful for the early diagnosis and therapeutic monitoring of various invasive fungal infections, but none proves the interest in trichosporiniose.
Trichosporon belong to amorphous basidiomycetes, characterised by spores, formed by septate strands and anastomosed branches. They are found in soil, water, decomposing matter and bird and bat dropping, but also in cheese or scarab. They belong to human micro biome, especially of the skin (essentially scrotum, perianal and inguinal sites), gastrointestinal and upper respiratory tracts. The transmission mode is unknown.
51 clinical isolate strains are identified, and 16 of which are able to infect humans [9]. Morphological and biochemical methodologies were unable to differentiate among the Trichosporon species. Several methods exist to identify the samples, like the physiological patterns, sequence polymorphisms of the internal transcribe spacer (ITS), intergenic spacer regions (IGS) of the rDNA genes.
Trichosporon spp. produce a biofilm, which is consisted of masses of bastoconidia, anthroconidia, pseudohyphae and long and short hyphae, featuring multi-layer cell structures, closely associated [6].
These cells produced and secreted enzymes, like extracellular proteases [6]. Aguiar et al. hypothised that the secretory aspartic protease is responsible of the antimicrobial resistance, as well as high levels of extracellular DNA. They can produce this biofilm in blood, urine and on skin.
The study of the fungal biofilm becomes more and more important for clinicians, because of its capability to increase mortality. Several techniques are used, like the crystal violet staining method or SEM (Scanning electron microscopy) [9,11].
In another side, Trichosporon species are able to produce glucoronoxylomannan, a capsular polysaccharide, like Cryptococcus neoformans, and it seems to play a probable role in mechanism of resistance [12,13].
It is generally accepted that according to different species, the virulence and resistance mechanisms are different. Trichosporon spp. is resistant to traditional antifungal drugs like Amphotericine B, Caspofungine, Fluconazole and Itraconazole, but relatively susceptible to Voriconazole. But, in some cases, we see resistance to azoles, due to high tolerance biofilm (Table 1).
| CMI (µg/mL) | |
|---|---|
| Voriconazole | 0.032 |
| Amphotéricine B liposomale | 0.5 |
| 5 fluorocytosine | >32 |
| Posaconazole | 0.094 |
| Fluconazole | 1 |
| Itraconazole | 0.75 |
Table 1: Susceptibility to antifungals.
Indeed, in his article, Chagas-Neto reported the presence of resistance of all antifungal agents tested (included Voriconazole), independent of genotype or isolation site. Moreover, the serum concentrations are lower than the MIC values.
Conclusion
In conclusion, to our knowledge this is the first published case of fatal invasive fungal infection with Trichosporon inkin in an allogeneic stem cell transplant recipient that was not successfully controlled with liposomal amphotericin B and voriconazole. Trichosporon spp. seems to be an emerging, opportunistic agent in immunocompromised patients with malignant haematological disease. Further research is needed to determine the best antifungal strategy, the optimal time and posology of treatment, and to identify the mode of dissemination of this fungal agent, the incubation period and mode of transmission in immunocompromised patients, and risk factors.
REFERENCES
- Marr KA, Carter RA, Crippa F, Wald A, Corey L. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2002;34(7):909–917.
- McNeil MM, Nash SL, Hajjeh RA, Phelan MA, Conn LA, Plikaytis BD, et al. Trends in Mortality Due to Invasive Mycotic Diseases in the United States, 1980–1997. Clin Infect Dis. 2001;33(5):641-647.
- Killick SB, Bown N, Cavenagh J, Dokal I, Foukaneli T, Hill A, et al. Guidelines for the diagnosis and management of adult aplastic anaemia. Br J Haematol. 2016;172(2):187-207.
- Camitta BM, Thomas ED, Nathan DG, Santos G, Gordon-Smith EC, Gale RP, et al. Severe aplastic anemia: A prospective study of the effect of early marrow transplantation on acute mortality. Blood. 1976;48(1):63-70.
- Bacigalupo A, Hows J, Gluckman E, Nissen C, Marsh J, Van Lint MT, et al. Bone Marrow Transplantation (BMT) versus immunosuppression for the treatment of severe aplastic anaemia (SAA): a report of the EBMT SAA working party. Br J Haematol. 1988;70(2):177-182.
- de Aguiar Cordeiro R, Serpa R, Flávia Uchoa Alexandre C, de Farias Marques FJ, Vladia Silva de Melo C, da Silva Franco J, et al. Trichosporon inkin biofilms produce extracellular proteases and exhibit resistance to antifungals. J Med Microbiol. 2015;64(11):1277-1286.
- Colombo AL, Padovan ACB, Chaves GM. Current knowledge of Trichosporon spp. and Trichosporonosis. Clin Microbiol Rev. 2011;24(4):682-700.
- Miceli MH, Díaz JA, Lee SA. Emerging opportunistic yeast infections. Lancet Infect Dis. 2011;11(2):142-151.
- Iturrieta-González IA, Padovan ACB, Bizerra FC, Hahn RC, Colombo AL. Multiple species of Trichosporon produce biofilms highly resistant to triazoles and amphotericin B. PloS One. 2014;9(10):26-28.
- Ramos JM, Cuenca-Estrella M, Gutierrez F, Elia M, Rodriguez-Tudela JL. Clinical case of endocarditis due to Trichosporon inkin and antifungal susceptibility profile of the organism. J Clin Microbiol. 2004;42(5):2341-2344
- Di Bonaventura G, Pompilio A, Picciani C, Iezzi M, D'Antonio D, Piccolomini R. Biofilm formation by the emerging fungal pathogen Trichosporon asahii: Development, architecture, and antifungal resistance. Antimicrob Agents Chemother. 2006;50(10):3269-3276.
- Fonseca FL, Frases S, Casadevall A, Fischman-Gompertz O, Nimrichter L, Rodrigues ML. Structural and functional properties of the Trichosporon asahii glucuronoxylomannan. Fungal Genet Biol. 2009;46(6):496-505.
- Thien SY, Chung SJ, Tan AL, Hwang WY, Tan BH, Tan TT. Recurrent trichosporonosis with central nervous system involvement in an allogeneic hematopoietic stem cell transplant recipient. Transpl Infect Dis. 2016;18(5):768-772.
Citation: Krzisch D, Camus V, David M, Gargala G, Lepretre S (2019) Fatal Invasive Trichosporonosis Caused by Trichosporon inkin after Allogeneic Stem Cell Transplant for Very Severe Idiopathic Aplastic Anemia. J Bacteriol Parasitol. 10.364. DOI: 10.35248/2155-9597.19.10.364.
Copyright: © 2019 Krzisch D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.