Citations : 2345
Dentistry received 2345 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 10, Issue 6
Evaluation of the Success of Strategic Implant® Placement for Immediate Loading Prosthesis in Edentulous Cases
Vivek Gaur1*, Anita Gala Doshi2 and Aroon K.S. Bengani32Dental Health, Mumbai, India
3Oro-Maxillofacial Surgery Department, Daswani Dental College, Kota, India
Received: 10-Aug-2020 Published: 02-Sep-2020, DOI: 10.35248/2161-1122.20.10.565
Abstract
Purpose: To compare and evaluate the efficacy of strategic implant® placement followed by immediate loading in regard to primary stability, quality of bone and survival and success of implants.
Material and Methods: This prospective cohort study included total 26 patients were selected from both sex, 19 males/7 females in age group of 40 to 70 years, were restored with strategic implant® irrespective of the quality and quantity of cancellous/alveolar bone following immediate functional loading protocols. 8 to 10 strategic implant® were placed per jaw and restored with a prosthesis within 72 hours. 447 BECES® implants, 20 BECES EX® implants, 4 KOC MICRO® implants and 2 ZDI implants were placed in the study.
Result: With the follow-up period of 22 months, results with strategic implant® were of great success with no delayed complications and failure with a success rate of ~99%. Secondary complications such as abutment screw loosening/fracture and peri-implantitis were not observed within the limitations of this study (p>0.05).
Conclusion: Regardless the bone volume, quantitively and qualitatively, functional rehabilitation of missing stomatognathic system following graft-less protocol is possible with the least traumatic and in-expensive technology thereby providing desired results benefitting the needful; secondary complications like graft resorption resulting in implant failure, abutment screw loosening, abutment screw fracture, peri-implantitis can be avoided with the technology of strategic implant®.
Keywords
Strategic implant®; Single piece implants; Immediate loading
Introduction
Dental implants currently commercially available are two piece (conventional implant, abutment and body are separate identity) or single piece (mono implant, where the abutment and body is in continuity) being surface treated of various designs, roughness and materials or smooth/machined polished implants. The loading protocols followed are either the delayed or immediate loading following various principles, school of thoughts and methodology. In immediate loading, we have non-functional or functional loading depending upon the strategic sites and bone (cancellous or cortical/basal) engaged.
Interestingly, we have different school of thoughts in implantology; Swiss, French, German and Italian school of thought. Swiss, following the delayed loading; i.e. fabricating the supra structure and prosthesis after a sufficient healing of fixture being engaged in alveolar/cancellous bone of the jaws and the Italian protocols where fixture is engaged in the cortical/basal bone and thus making it possible to immediately provide the prosthesis and fabricate the fixture in function . Here the screw design single piece rough or polished implants/fixtures were placed [1].
Pasqualini et al. [2], Ihde et al. [3], have published their work on immediate functional loading implantology with various designs like blade implants, vent implants, screw implants, diskos/boi lateral/basal implants [3]. In conventional/alveolar implantology “All on Four” is the most preferred method for immediate functional loading in atrophic jaws where the implants are placed between inter-mental foramen of lower jaw and in premaxilla region but having cantilever extension. Salama et al. [4], proposed a prerequisite for immediate functional loading which emphasizes on avoidance or reduction of cantilever, high density bone at implant site, implant design that increases mechanical retention, rough implant surface to increase primary stability, bi-cortical implant placement for increased stability, avoidance or reduction of distal cantilevers and protected occlusal scheme against overloading.
A technique in which the implant supported restoration is placed within 48 hours of implant insertion and a distinction was made between the immediate restoration for aesthetic purpose–out of occlusal contacts and true immediate loading. The demand and need of the population are to have an ideal solution for the replacement of lost tooth/teeth with minimal expenses, least traumatic, flapless, painless, quick to restore and rehabilitate with minimal time consumed/spent. Prof. Stefan Ihde with all his past experience and knowledge of bone and basal implantology redefined strategic implantology® [5].
The principles of orthopedic [6,7] and traumatology [8] follow the principles of the concept of strategic implantology® [9] that involve that if implants are initially stable but have not yet undergone biologic osseointegration, this clinical situation is similar to the surgical stabilization of mobile bone fragments by osteosynthesisplates in orthopedic surgery. Here the smooth surface screws are used, and bi-cortical anchorage is done. Non-parallel screws are used to enhance macro anchorage. Rigid splinting is done by fracture plates, similar to prosthesis/bridge in dental implantology. Stable anchorage areas for cortical engagement, infection–free cortical bone, resorption free bone areas like buttresses being low in metabolism, thin mucosal penetration, smooth surface thus virtually no peri-implantitis, an abutment preferably single piece, bending zone, avoidance of cantilever, cross arch splinting, splinting within 72 hours, before the bone remodeling starts. More the atrophy, the greater one has to splint.
The strategic implant® [10] is non-homogenous, designed following the concept of strategic implantology. They are smooth or polished surface like osteosynthesis plates used in traumatology. Self-tapping with self-cutting threads for maximum bone to implant contact and increased insertion torque. For retrievability, single piece multiunit mono implants are there. Body of the implants is thin but strong enough to sustain occlusal loading. They are bendable in order to bring the abutment to a desired prosthetic plane after engaging the buttress. Also, the desired cortical bone is mandatory to sustain occlusal function. Almost all the implants are designed to be placed flapless minimizing regional acceleratory phenomenon [11] and most atraumatic to patient. Force transmission at apical threads engaged at the intended cortices and buttress, negligible influence at the unstable crestal cortical of which all conventional implantology is been based on its support.
This study is an attempt to focus on the efficacy of strategic implant®, following immediate loading protocol as well as to compare and evaluate the efficacy of strategic implant placement followed by immediate loading in regard to primary stability, quality of bone and survival and success of implants.
Materials and Methods
Source of the data
The prospective cohort study was conducted with the patients reporting to the Department of Oral And Maxillofacial Surgery, Daswani Dental College and Research Centre, Ranpur, Kota for implant placement and immediate loading using strategic implant® as per feasibility of case. Total 26 patients were included from both genders, 19 males/7 females in age group of 40 to 70 years, who were previously restored with strategic implants® irrespective of the quality and quantity of cancellous/alveolar bone following immediate functional loading protocols. The study included 8 to 10 strategic implant® per jaw were placed and restored with prosthesis within 3 days.
Selection criteria
Inclusion criteria: Patients presented with partial or full edentulism in the upper or lower jaw. Patients having atrophied ridges were preferred.
Exclusion criteria: General: If suspected that the treatment could affect the patient’s health condition like pregnancy. If patient’s cooperation appeared questionable. If patient did not give his or her informed consent to participate. History of radiotherapy in the head and neck region for malignancies, chemotherapy for treatment of malignancy within 1 year of the procedure desired. Uncontrolled diabetic and hypertension or any systemic condition which contradict any surgical procedure. Local: The planned implant area persisting lesions, such as tumor or recent irradiation, or showed signs of chronic bone diseases.
Procedure
The overall design is a prospective, cohort study. After informed consent of all the patients was obtained, a clinical examination (Figure 1) and a detailed explanation of the study including the study procedures and required post-operative follow up visits was given to the patient. Then a surgical template was used for the assessment of the implant angulation and labio-palatal width of the dentulous/ edentulous ridges that was done previously. At the following visit, the procedure of implant placement, extraction, curettage and impression was done followed by the metal framework trial and subsequently the delivery of the prosthesis. At the follow up visit, assessment of soft and hard tissue conditions at the implant site was conducted and corrections were performed if required. At the 40th day post-operatively, 6th month and 1 year follow up assessment of soft and hard tissue conditions at the implant site was repeated and corrections were performed radiographically and clinically.
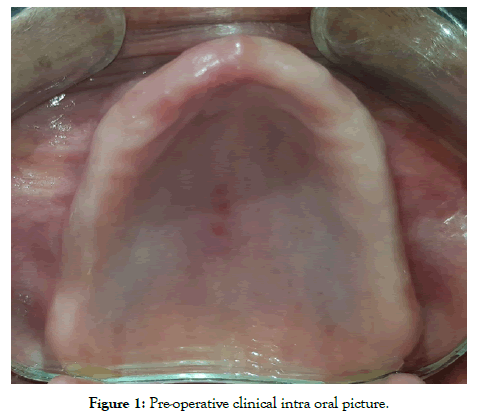
Figure 1: Pre-operative clinical intra oral picture.
Technique and protocols: Depending upon the various classifications of jaw ridges regarding available cortical and cancellous bone like Atwood [12,13], Cawood et al. [14], Lekolm et al. [15], Seibert JS [16] Paraskevic VL [17], different design of strategic implant® were chosen. With available crestal bone width and height strategic implant® designs like BECES EX, KOC MICRO, KOC PLUS or BECES implants are placed otherwise with atrophies where height and width of cancellous/ alveolar are deficient only BECES and ZDI are the only option available for successful rehabilitation with higher prognosis. The placement was done under local anesthesia and the implants were placed at strategic sites fixated with other cortical like 2nd or 3rd cortical (Figures 2 and 3). The methodology of strategic implant® placement [18] was followed. A specific terminology was created for the strategic implant® placement protocols [19]. The purchase point of the strategic implant® at 1st cortical is mostly different and away from the 2nd and 3rd cortical where the masticatory force transmission occurs. Usually the long implants are placed and bended being splinted, preferably cross arch to bring the masticatory surfaces within the “Supporting Polygon” [20]. The concept of accepted principle “Primum Nihil Nocera” i.e. limiting treatment and restorations were done in least traumatic methods following graft-less protocols.
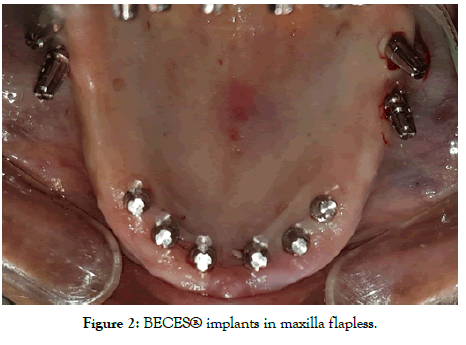
Figure 2: BECES® implants in maxilla flapless.
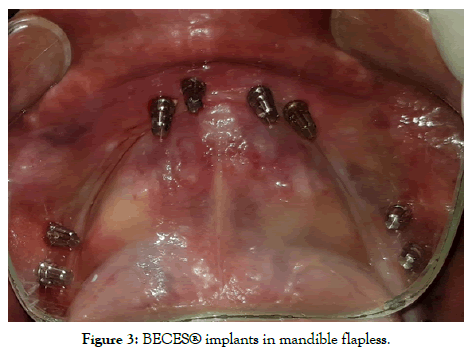
Figure 3: BECES® implants in mandible flapless.
All the procedure was performed in routine dental operatories. Procedures were mostly flapless unless extraction had to be done. Local anesthetic Lignox® (Lignocaine with 1:80000 adrenaline) was administered and nerve blocks were avoided, especially in the lower jaw. Depending upon the quality/quantity of crestal bone at site, KOC, BECES, BECES EX was chosen according to manufacturer recommendations. After implants placement impression was made by additional silicon putty (Flexeed®) with impression pick-ups supplied by manufacturer, and master cast was made with lab analogs on the same day (Figures 4-6). Next day metal cobalt-chromium trial was done to check the fit for the circular bridges, jaw relationship been made by aluminum reinforced wax (Aluwax®) (Figures 7-9). Occlusal plane is been recorded by fox bite plane. On the third day, within 72 hours the prosthesis was delivered, preferably metal to plastic/acrylic in most of the cases but also metal to ceramic. Finally, the bridge was cemented by permanent cement Fuji plus by GC. It’s imperative to complete and load the system within 72 hours before bone remodeling starts. Occlusal scheme is provided preferably lingualized occlusion or in group function when opposite arch is natural teeth. Instructions to patient explained and recall/follow up schedule explained (Figures 10-13).
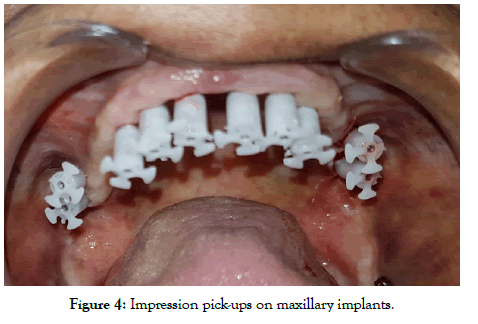
Figure 4: Impression pick-ups on maxillary implants.
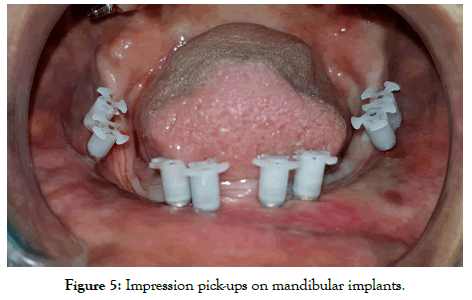
Figure 5: Impression pick-ups on mandibular implants.
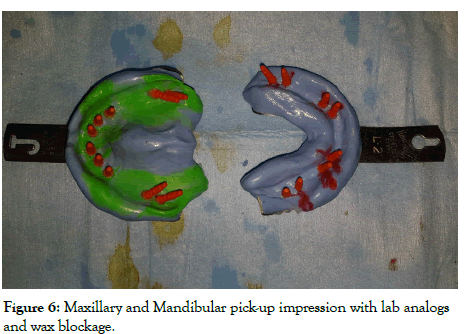
Figure 6: Maxillary and Mandibular pick-up impression with lab analogs and wax blockage.

Figure 7: Co-Cr metal framework trial on maxillary implants.
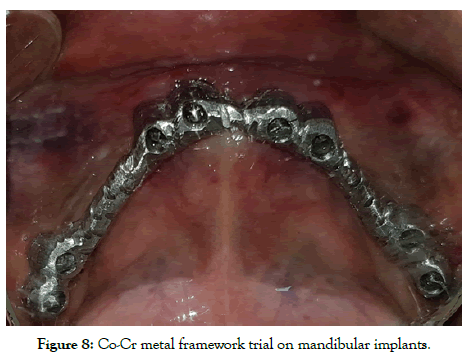
Figure 8: Co-Cr metal framework trial on mandibular implants.
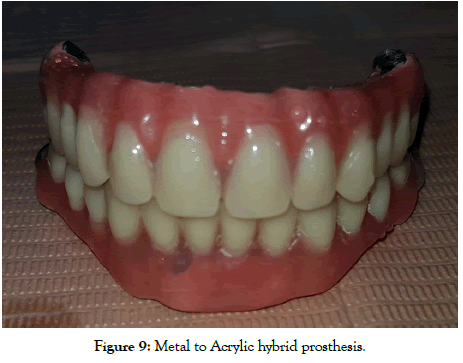
Figure 9: Metal to Acrylic hybrid prosthesis.
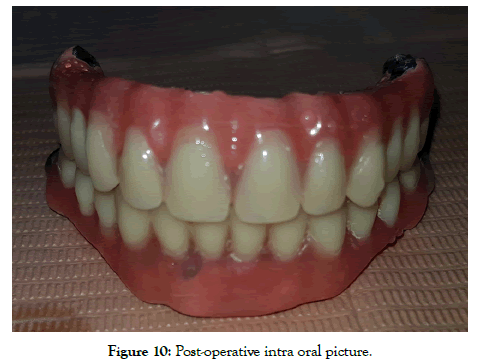
Figure 10: Post-operative intra oral picture.
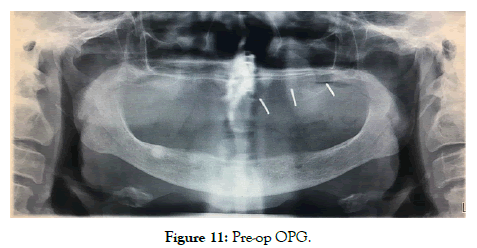
Figure 11: Pre-op OPG.
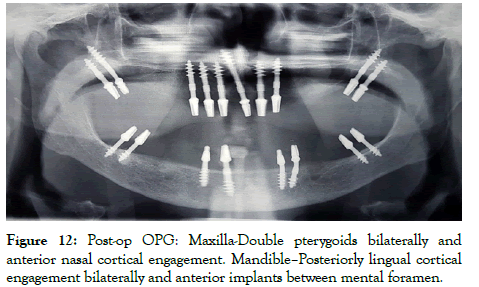
Figure 12: Post-op OPG: Maxilla-Double pterygoids bilaterally and anterior nasal cortical engagement. Mandible–Posteriorly lingual cortical engagement bilaterally and anterior implants between mental foramen.
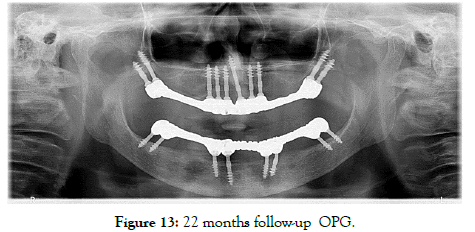
Figure 13: 22 months follow-up OPG
Figures 1 to 13 are in detail describing the procedure with followup radiograph, OPG.
Results
No patient was withdrawn from the study, and all 26 patients 19 males and 7 females (with 473 immediately loaded implants) were followed for at least 12 months. No fractures or loosening of the cemented bridges were observed during the study (Table 1). One maxillary segment and one mandibular segment on the same patient were restored with metal to ceramic prosthesis. 447 BECES® IMPLANTS, 20 BECES EX®IMPLANTS, 4 KOC MICRO® IMPLANTS AND 2 ZDI IMPLANTS were placed in the study. All the 26 patients treated were rehabilitated successfully with strategic implant® within 72 hours, according to the strategic principles, the prosthesis were fixed over implants and the desirable occlusal scheme restored (p>0.05) (Tables 2 and 3). Till the date of study done/followed, no patient complained of any mobility or fracture of the prosthesis or the implants, thus were free of pain and swelling except one patient who was restored with mandibular full arch construction complained (p>0.05). Patient satisfaction questionnaire results were extremely favorable. All prosthetic constructions (Even if they were planned for shortor medium-term temporary use) were cemented with Fuji plus (Obtained from GC EUROPE N.V, Leuven) (Handmix variant) definitive cement. This procedure is necessary to establish absolute stability (Secure splinting) between the implants and the bridges as they are required according to the principles of therapy in traumatology and orthopedic surgery (AO principles). In case of pairwise comparison the results were not statistically significant. There was no statistically significant correlation between different types of prosthetic work on BECES®implants (p>0.05). In pairwise comparison the results were not statistically significant (Tables 4-6). Only 8 BECES® implant showed signs of overload osteolysis, clinically and radiographically throughout the whole observation period. 465 (98.2%) BECES®/BECES N®/BCS® implants out of 473 were in full function, without pain, mobility or visible infection, resulting in a clinical survival rate of 99.7 % after a mean of 12 months. 8 of the BECES implants showed sign of overload osteolysis (Tables 7 and 8). Table 8 shows complications as observed during clinical check-up and according to patients report. The survival rate for BECES implants placed in the mandible in comparison to those placed in maxilla came to: 100% vs 96.1% (p>0.05). 8 of BECES implants showed radiological signs of overload osteolysis. The survival rate for all implant type placed in the mandible in comparison to those placed in maxilla was: 100% vs 96.1% since 8 implants failed in the mandibular region but all implants survived in the maxilla (p>0.05).
| Observed parameters | n (%)/(X ± SD; (Med; min-max) |
|---|---|
| Number of patients | 26 |
| Number of implants | 473 |
| Number of implants in full function | 473 (100%) |
| Age | 40-80 |
| Gender: Male/Female | 19 (73.07)/7 (26.92), p>0.05 |
| Hypertension: Yes/No | 12 (53.84)/14 (46.15), p>0.05 |
| Diabetes mellitus: Yes/No | 5 (19.23)/21 (80.76) |
| Smokers: Yes/No | 10 (38.46)/16 (61.53) |
p>0.05 Indicates no significant difference between the groups with regard to gender and hypertension distribution
Table 1: Patient characteristics.
| Target corticals | N (%) |
|---|---|
| Nasal cortical | 159 (33.61) |
| Sinus floor | 4 (0.84) |
| Palatal cortical | 3 (0.63) |
| Zygoma | 2 (0.42) |
| Pterygoid | 99 (20.93) |
| Mandibular inter-foraminal anchorage | 104 (21.98) |
| Distal mandible anchorage without cortical engagement | 4 (0.84) |
| Distal cortical mandible engagement | 98 (20.71) |
| Significance | p<0.05* |
*Indicates a significant difference in the number of corticals engaged by the implants in regard to the various regions
Table 2: Types of corticals engaged by implants.
| Different prosthetic constructions | No of implants |
|---|---|
| Full bridge upper | 267 (56.44) |
| Full bridge lower | 200 (42.28) |
| Segment upper | 0 (0) |
| Segment lower | 6 (1.26) |
Table 3: Types of prosthetic constructions and number of implants.
| Implant and placement characteristics | n (%) | Follow-up | |
|---|---|---|---|
| Type of implant | BECES | 447 (94.50) | 98.20% |
| KOC MICRO | 4 (0.84) | 100% | |
| ZDI | 2 (0.422) | 100% | |
| BECES EX | 20 (4.22) | 100% | |
| Implant location (jaw) | Maxilla | 26 | 100% |
| Mandible | 26 | 96.10% | |
| Significance | p>0.05 | p>0.05 | |
p>0.05 Indicates no significant difference between the implant location groups
Table 4: Types of implants and placement locations.
| Full jaw | Maxilla | Radiological follow-up 100% | |
| Mandible | 25 | 96% | |
| Segment | Maxilla | 0 | 100% |
| Mandible | 1 | 100% | |
| Significance | p>0.05 | ||
p>0.05=No significant difference
Table 5: Extent of reconstruction
| Metal to plastic | Maxilla | 25 |
| Mandible | 25 | |
| Metal to ceramic | Maxilla | 1 |
| Mandible | 1 | |
Table 6: Type of prosthesis.
| Place of anchorage in the 2nd cortical (Different target corticals) | Radiological follow up | Clinical Inspection as follow up | Patient report as follow up |
|---|---|---|---|
| Floor of nose | 100% | 100% | 100% |
| Palatal engagement (for anteriors and premolars only) | 100% | 100% | 100% |
| Tubero-pterygoid | 100% | 100% | 100% |
| Mandible inter-foraminal anchorage | 96.50% | 96.50% | 96.50% |
| Distal mandible anchorage without cortical engagement (for KOS implants) | 100% | 100% | 100% |
| Cortical engagement distal mandible (for BCS implants) | 95.10% | 95.10% | 95.10% |
| Significance | p>0.05 | p>0.05 | p>0.05 |
Table 7: Implant survival under different aspects.
| Mobility | Yes/No | 8/465 |
| Local soft tissue | Yes/No | 8/465 |
| Infection | Yes/No | 8/465 |
| Pain | Yes/No | 8/465 |
| Bone loss | Yes/No | 8/465 |
| Significance | p>0.05 | |
Table 8: Implants: failures and remedies-clinical and radiological signs and symptoms of ailing or failing implants.
Discussion
Immediate functional loading on dental implants has become an established protocol and was first discussed/proposed by Schnitman et al. [21]. Both the cortical and cancellous bone adapts favorably following frost ‘Mechanostat’ theory [22]. With bone in function, the favorable trabecular arrangement leading to high mineralization locally. Bone optimizes weight of performance– Wolff’s law [22]. There is a need to have high insertion torque, depending upon the design of the implants and rigid splinting/ cross arch splinting for the success.
Krekmanov et al. [23], states that strain gauge measurements in vivo, showed no difference in the bending movements on the tilted implants. Bending movements measured rarely above 20 Ncm. Rigidity of the prosthesis counteracts the relatively small bending movements applied to tilted implants. Cross arch splinting allows enough micromotion for the patient to function but not enough to prohibit osseointegration. Off axis loading goes hand in hand with cross arch splinting.
Pilliar et al. [24], suggest micromotion greater than 150 microns will lead to failure having fibrous encapsulation greater than 1 Angstrom but 25 to 50 Microns movement is desirable for the bone contact with implants leading to essential and initial foreign body response by bone–protein adsorption, platelet activation, coagulation and inflammation. The term pressure necrosis is generally used for any bone resorption because of high insertion torque but there is sufficient literature to support bone apposition and favorable healing with fixtures placed of high insertion torque [25,26]. Routinely when in discussion of graft-less solution for rehabilitation of non-atrophic to moderate atrophic jaws in conventional/alveolar implantology the “All on Four” treatment protocols is been explained and implemented. All on four protocols is a modified treatment modality of all on six by Prof. Branemark where the most distal implant is tilted 15 degree bilaterally to reduce anterio-posterio span of the cantilever with great success. The current concept proposes to have 4 implants between intermental foramen and in premaxilla, where the distal is tilted up-to 45 degree. However, presently, we have insufficient evidence in literature to support as there is violation of biomechanics when used with long cantilever [27,28].
Another debatable issue is implants being rough surface , no doubt because of adhesion of clot and its minimal retraction and enhance coagulation we have additive benefit of contact osteogenesis with secondary distant osteogenesis regarding bone bonding with foreign object like implants [24] but there is high risk of the surface getting secondary infected by pathogens and bacteria [29] leading to the current disease of millennium “Peri-implantitis’’ which is not the case with smooth/machined surface implants [30]. Smooth surface titanium is most accepted to oral mucosa and attached mucosa is not mandatory around the smooth surface Titanium [31]. Thin but strong body of implants resist bone resorption at crestal level where-as there is continuous bone loss at crestal level with conventional design [32].
With following the principles of strategic implantology® with strategic implant® immediate functional loading implantology has become most predictable and getting accepted globally. Design of implants being used are smooth surface self-tapping threaded design [33,34] meant to engage and transfer masticatory load in the basal bone, buttresses like Pterygomaxillary, Zygomaticomaxillary, Frontomaxillary [35] and the other cortical that have been previously mentioned. Here the cancellous or alveolar bone is of least significant unlike conventional implantology, woven bone is not desirable at the implant vicinity and aim is to restrict or delay remodeling [36,37]. Long polished surface implants are used to reach the most load resisting high mineralized bone with minimal metabolism, the cortical, buttresses and basal bone. The insertion point at 1st cortical level doesn’t fall in axis with the site engaging the masticatory load transmission threads [19] but when splinted preferably cross arch resist the load better and more suitably then the load transmission on parallel implants. Here implants are bent along the long body of implant [38]. Longer the implants, easier to bent without disturbing the crystal structure of titanium alloy, to bring the abutments for the desirable prosthetic plane inside “SUPPORTING POLYGON’’ [20]. According to the law of physics the long arm/body of the implant resist the forces and transmit inside bone, where load is transferred by short abutment open to oral environment. As force is inversely proportional to area, in the long end-osseous body of implant, force transmission is minimized. There is need to splint the implants within 72 hours before the remodeling sequence Activation-Resorption-Formation (ARF); kicks in [39]. Here the most preferred implant placed is BECES® then the BECES EX®and then the KOC® MICRO implants [40]. BECES® implants works on the principle of osteosynthesis screws used in orthopedics and traumatology. BECES EX® and KOC MICRO®being root form taper in design, former being smooth surface and later with modified NOITIS® surface. KOC implants compresses the cancellous bone to achieve high primary stability, their mode of function is termed “corticallization of cancellous bone’’ [39]. All the implants are single piece, mono implants [40]. Thus, the chances of screw loosening and micro motion at 1st cortical leading to crestal bone loss are second to none. In-fact post bone remodeling bone apposition is appreciated at buttress sites.
As its widely known circular bridges are not accepted in the lower jaw because of mandibular flexion but the sufficient evidences also exist supporting the horse shoe bridges in the mandible provided the fixtures engaging the strategic position and implant design being isoelastic compatible with mandibular flexion [34,41]. The ideal prosthesis material preferred is cobalt-chromium alloy framework with chewing table of acrylic or indirect composite, ceramic can also be used in ideal condition but to be rigidly splinted by permanent cement [42,43]. Concept is to have modulus of elasticity as close to bone as possible [44]. Cases are completed ideally with lingualized occlusion and when opposite arch consist of natural teeth group function is the most desired occlusal scheme with shallow guidance and compensatory curves, existence of ideal freeway space most mandatory for the survival of system [45-48]. Prosthesis is completed as cement retained; but the single piece multiunit strategic implants with retrievability are also available [49].
Conclusion
Strategic implantology® is a long proven and simplified technology for restoration/rehabilitation of stomatognathic complex following immediate functional loading protocols. The concept is based on principles of traumatology and orthopedics. Here the most complex and atrophic jaws are restored with the concept of accepted principle “Primum Nihil Nocera’’ i.e. limiting treatment. There is virtually no contraindication for the restoration/rehabilitation by strategic implant® other than the patient on intra-venous bisphosphonates. A patient who can be operated for a routine dental procedure can be treated by strategic implantology®. Here we can successfully avoid the painful, unpredictable and unwarranted expensive augmentation procedures by engaging strategic sites and thus avoiding unfavorable cantilever situations prosthetically and biomechanically. But the science demands considerable experience and thorough knowledge anatomically and prosthetically from the operator and it also has a reasonable learning curve.
Conflict of Interest
NoneFunding
No funding was obtained for this study.
Ethical Approval and Registration of Research Studies
The research was registered at Daswani Dental College, Kota, India, Rajasthan University of Health Sciences (RUHS), Jaipur, India after the approval of research ethical committee of Daswani Dental College, Kota, India.
Consent
The approval of patients included in the study were obtained for the treatment and publication.
Guarantor
Dr. Vivek Gaur
REFERENCES
- https://pubmed.ncbi.nlm.nih.gov/28125196/.
- Pasqualini ME, Tramonte SU, Linkow LI. Half a century of function a retrospective analysis of tramonte endosteal screw dental implants that lasted 50 and 36 years: a case report. J Dent Oral Health. 2016;2:1-8.
- Ihde S. Principles of BOI. Springer, Heidelberg, Berlin, Germany. 2005:27.
- Salama H, Rose LF, Salama M, Betts NJ. Immediate loading of bilaterally splinted titanium root-form implants in fixed prosthodontics–a technique reexamined: two case reports. Int J Periodont Restorative Dent. 1995;15:344-361.
- Ihde S, Ihde A. Introduction into the work with strategic implants (3rd edn), The International Implant Foundation Publishing, Munich, Germany.
- NIisson BE, Westlin NE. Bone density in athletes. Clin Orthop Relar Res. 1971;77:179-182.
- Rubin ER, Mcleod KJ, Bain SD. Functional strains and cortical bone adaptation: epigenic assurance of skeletal integrity. J Biomechania. 1990;23:43-54.
- Ruedi TP, Murphy WM. AO principles of fracture management. Thieme, Stuttgart, New York, United States.
- Ihde S, Ihde A. Immediate loading (2nd edn), 2012.
- Gupta AD, Verma A, Dubey T, Thakur S. Basal osseointegrated implants: classification and review. Int J Contemp Med Res. 2017;4:2329-2335.
- Verna C. Regional acceleratory phenomenon. Front Oral Biol. 2016;18:28-35.
- Atwood DA. Bone loss of edentulous alveolar ridges. J Periodontol. 1979;50:11-21.
- Atwood DA. The reduction of residual ridges: a major oral disease entity. J Prosthet Dent. 1971;26:266-279.
- Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17:232-236.
- Lekholm U, Zarb GA, Albrektsson T. Patient selection and preparation. Tissue integrated prostheses. Quintes-sence Publishing Co Inc, Chicago, United State.
- Seibert JS. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts. Part I. Technique and wound healing. Compend Contin Educ Dent. 1983;4:437-443.
- Paraskevich VL. Dentalnaya implantologiya, MIA Publishing, Moscow, Russia.
- International implant foundation: Konsensus on 16 methods for the placement of basal implants.
- Ihde S, Ihde A, Lysenko V, Konstantinovic V, Palka L. New systematic terminology of cortical bone areals for osseo-fixated implants in strategic oral implantology. J J Anatomy. 2016;1:007.
- Ihde S, Ihde A. Cookbook mastication (2nd edn), International Implant Foundation Publishing, Munich, Germany.
- Schnitman PA, Wöhrle PS, Rubenstein JE, DaSilva JD, Wang NH. Ten-year results for brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants. 1997;12:495-503.
- Frost HM. Wolff’s law and bone’s structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994;64:175-188.
- Krekmanov L, Kahn M, Rangert B, Lindström H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000;15:405-414.
- Pilliar RM, Lee JM, Maniatopoulos C. Observation on the effect of movement on bone ingrowth into porous surfaced implants. Clin Orthop. 1986;208:108-113.
- Doblar'e M, Garc'ıa JM, Go'mez MJ. Modelling bone tissue fracture and healing: a review. Eng Fract Mech. 2004;71:1809-1840.
- Trisi P, Todisco M, Consolo U, Travaglini D. High versus low implant insertion torque: a histologic, histomorphometric, and biomechanical study in the sheep mandible. Int J Oral Maxillofac Implants. 2011;26:837-849.
- Khayat PG, Arnal HM, Tourbah BI, Sennerby L. Clinical outcome of dental implants placed with high insertion torques (up to 176 Ncm). Clin Implant Dent Relat Res. 2013;15:227-233.
- Greco GD, Jansen WC, Landre J, Seraidarian PI. Stress analysis on the free-end distal extension of an implant-supported mandibular complete denture. Bras Oral Res. 2009;23:175-181.
- Bonnet AS, Postaire M, Lipinski P. Biomechanical study of mandible bone supporting a four-implant retained bridge: Finite element analysis of the influence of bone anisotropy and foodstuff position. Med Eng Phys. 2009;31:806-815.
- Harris LG, Richards RG. Staphylococci and implant surfaces: a review. Injury. 2006;37:S3-S14.
- Esposito M, Ardebili Y, Worthington HV. Interventions for replacing missing teeth: different types of dental implants. Cochrane Database Syst Rev. 2014;22:CD003815.
- Neiva RF, Neiva KG, Oh TJ, Wang HL. Clinical and morphological aspects of the implant/soft tissue interface. Int Chin J Dent. 2002;2:151-161.
- Qutub MNAL. Radiologic evaluation of the marginal bone loss around dental implants with different neck diameters. Pak Oral Dental J. 2011;31:150-153.
- Iezzi G, Pecora G, Scarano A, Perrotti V, Piattelli A. Immediately loaded screw implant retrieved after a 12-year loading period: a histologic and histomorphometric case report. J Osseointegrat. 2009;2:54-59.
- Strecha J, Jurkovic R, Siebert T, Prachar P, Bartakova S. Fixed bicortical screw and blade implants as a non-standard .solution to an edentulous (toothless) mandible. Int J Oral Science. 2010;2:105-110.
- Sorní M, Guarinos J, Peñarrocha M. Implants in anatomical buttresses of the upper jaw. Med Oral Patol Oral Cir Bucal. 2005;10:163-168.
- Leonard G, Coelho P, Polyzois I, Stassen L, Claffey N. A study of the bone healing kinetics of plateau versus screw root design titanium dental implants. Clin Oral Impl Res. 2009;20:232-239.
- Goldmann T, Ihde S, Kuzelka J, Himmlova L. Bendable vs angulated dental implants: consideration of elastic and plastic material properties based on experimental implant material data and FEA. Biomed Pap Med Fac Univ Palacky Olomouc Czek Repub. 2008;152:309-316.
- Martin R, Burr D, Sharkey N. Skelettal tissue mechanics (1st edn). Springer, New York, United States.
- http://www.biomedimplant.com/phocadownload/casi-clinici/long_term.pdf.
- Hunter R, Alister F, Moller J, Alister JP. A new approach to modelling and designing mono-block dental implants. J Archiev Mater Manuf Eng. 2007;22:77-80.
- https://refubium.fu-berlin.de/handle/fub188/12357?show=full&locale-attribute=en.
- Shadid R, Sadaqa N. A comparison between screw- and cement-retained implant prostheses. A literature review. J Oral Implantol. 2012;38:298-307.
- Greco GD, Jansen WC, Landre Junior J, Seraidarian PI. Stress analysis on the free-end distal extension of an implant-supported mandibular complete denture. Braz Oral Res. 2009;23:175-181.
- Kamath R, Sarandha DL, Thomas S, Sachdeva B. Lingualized occlusion: an emerging treatment paradigm for complete denture therapy: a review article. J Med Dent Sci Res. 2015;2:06-09.
- Swaminathan Y. Implant protected occlusion. J Med Dent Sci. 2013;11:20-25.
- Rangarajan V, Yogesh PB, Gajapathi B, Ibrahim MM, Kumar RG, Karthik M. Concepts of occlusion in prosthodontics: a literature review, part I and II. J Indian Prosthodont Soc. 2016;16:8-14.
- Jacob SA. Occlusal principles and considerations for the osseointegrated prosthesis . IOSR J Dent Med Sci. 2013;3:47-54.
- Gaur V, Doshi A, Idhe S, Fernandes G. Immediate loading of edentulous mandible arch with screw retained final prosthesis on strategic implants® with single piece multiunit abutments heads: a case report. BAOJ Dentistry. 2018;4:0042.
Citation: Gaur V, Doshi AG, Bengani AKS (2020) Evaluation of the Success of Strategic Implant® Placement for Immediate Loading Prosthesis in Edentulous Cases. Dentistry 10: 565. doi: 10.35248/2161-1122.20.10.565
Copyright: © 2020 Gaur V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.