Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 18, Issue 4
Evaluation of Predictive Value of Uterine Artery Doppler Indices versus Histopathology Sampling in Detection of Abnormal Uterine Bleeding in Intrauterine Contraceptive Device Users
Mai Ahmed Gobran1*, Sabah Mohamed El Hanafy1, Walid Mohamed Elnagar2, Ahmed Mahmoud Abdou Ahmed2, Amr Ahmed Abdelrhman3, Mohamed El-Bakry Lashin3, Yasser S. Saraya3, Eman Ramadan Abd El Fattah4, Khaled Fathy Helal2, Hebatullah Abulkhair1, Abeer M Abdel Barry5 and Mohamed SH Ramadan32Department of Obstetrics and Gynaecology, Zagazig University, Ash Sharqia Governorate, Egypt
3Department of Obstetrics and Gynaecology, Zagazig University, Zagazig, Egypt
4Department of Anatomy, Zagazig University, Zagazig, Egypt
5Department of Pathology, Gonzaga University, Zagazig, Egypt
Received: 01-Mar-2021 Published: 22-Mar-2021, DOI: 10.35248/2090-7214.21.18.382
Abstract
Background: Contraceptive intrauterine device (IUD) is a successful method of contraception that has been used for more than 30 years. However, it is associated with excessive uterine bleeding, that might cause iron deficiency anaemia, making CIUD use inconvenient for many women especially those with severe menstruation.
Objective: The objective of our study was to evaluate the correlation between abnormal uterine bleeding in IUD with endometrial sampling.
Methods: Study included 120 women from the obstetrics and gynaecology departments of Zagazig University Hospitals, divided into three groups: Group I included 40 women who used intrauterine coipper (TCu-380A) and complained of menorrhagia or menometrorrhagia. Group II included 40 womenusing CIUD and not complaining of abnormal uterine bleeding. Group III included 40 women complaining of vaginal discharge or requesting CIUD insertion, and not complaining of abnormal uterine bleeding as a control group.
Results: PI and RI were significantly lower in IUD-induced irregular bleeding than in IUD-induced women who did not complain of abnormal vaginal bleeding.
Conclusion: Endometrial biopsy has no role in predicting the abnormal uterine bleeding cause. Transvaginal ultrasonography findings can be efficiently used to classify women at risk of experiencing excessive uterine bleeding following CIUD insertion and to make a preliminary diagnosis, thus, notify the pathologists.
Keywords
Endometrial thickness; Endometrial polyp; Endometrial atrophy; Endometrial stromal sarcoma; Endometrial cancer; Prediction of uterine bleeding, Doppler, Colored doppler
Introduction
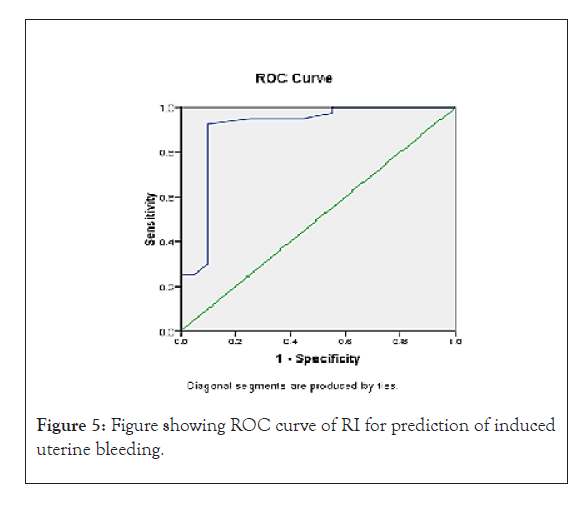
The Intrauterine Device (IUD) is the most widely used reversible form of contraception in the World [1]. Menstrual disorders are a common indication for medical visits among women of reproductive age and heavy menstrual bleeding affects up to 30% of women throughout their reproductive lifetime. AUB may be defined as any variation from the normal menstrual cycle, and includes changes in regularity and frequency of menses, in duration of flow, or in amount of blood loss [2]. Ultrasound is the imaging modality of choice for the female pelvis. It is widely available, has broad acceptance by patients and is relatively inexpensive. High-resolution imaging of transvaginal ultrasound provides high diagnostic accuracy for pelvic pathology [3] used color Doppler ultrasonography to confirm the hypothesis that CIUD-induced bleeding is secondary to an increase in the uterine blood flow (as indicated by decreased PI and RI in uterine artery). They constructed the ROC curves for PI and RI to choose the cutoff values for discriminating between women using CIUD and complaining of menorrhagia or menometrorrhagia and women using CIUD and not complaining of abnormal uterine bleeding. These are a plot of the true positive rate (sensitivity) against the false positive rate (1-sensitivity) for the different possible cut points of a diagnostic test. In the first case (PI) they obtained a ROC area of 0.829 and we chose 2.07 as the cutoff point, the value of the area showed the accuracy of the test. In the second case (RI) we obtained a ROC area of 0.804 and we chose 0.7 as the cutoff point, the value of the area showed the accuracy of the test. PI has sensitivity 84.4% and specificity 83.3% in the detecting women with CIUD complaining of abnormal uterine bleeding and RI has sensitivity 78.1% and specificity 80% in the detecting women with CIUD complaining of abnormal uterine bleeding. So, transvaginal color Doppler can be used to identify women at risk of developing abnormal uterine bleeding after CIUD insertion [4].
Aim of the work
To determine whether transvaginal color Doppler can be used to identify women at risk of developing abnormal uterine bleeding after IUD insertion.
Patients and Methods
This study was a prospective clinical study including women who have been wearing a CIUCD, presenting to Obstetrics and Gynecology Department, Zagazig University Hospitals from May 2018 to May 2020.
HStudy populations
The study included 120 women. Sample size was calculated using Epi-Info® version 6.0 software, assuming a power of 80% and an α-error of 0.5%.
Included women were divided into three groups:
• Group I included 40 women using copper intrauterine device (TCu-380A) and complaining of menorrhagia or menometrorrhagia.
• Group II included 40 women using CIUD and not complaining of abnormal uterine bleeding.
• Group III included 40 women complaining of vaginal discharge or requesting CIUD insertion, and not complaining of abnormal uterine bleeding as a control group. Inclusion criteria
• Regularly menstruating women before CIUD insertion.
• Age between 20 and 35 years.
• Hormonal treatment not taken at least 2 months before the study.
• Non-steroidal anti-inflammatory not taken 24 hours before the examination Exclusion criteria
• Pregnancy.
• Nulligravida.
• Present or past history of pelvic inflammatory disease.
Other causes of abnormal uterine bleeding such as adenomyosis and the presence of pelvic pathology as ovarian cysts, pelvic endometriosis, endometrial polyps and uterine fibroids.
Methods
After taking verbal and written consent to participate in the study, each patient was subjected to the following: Full history taken and examination
Routine investigations
Blood group and Rh factor.Complete blood count.Random blood sugar.
Ultrasound examination
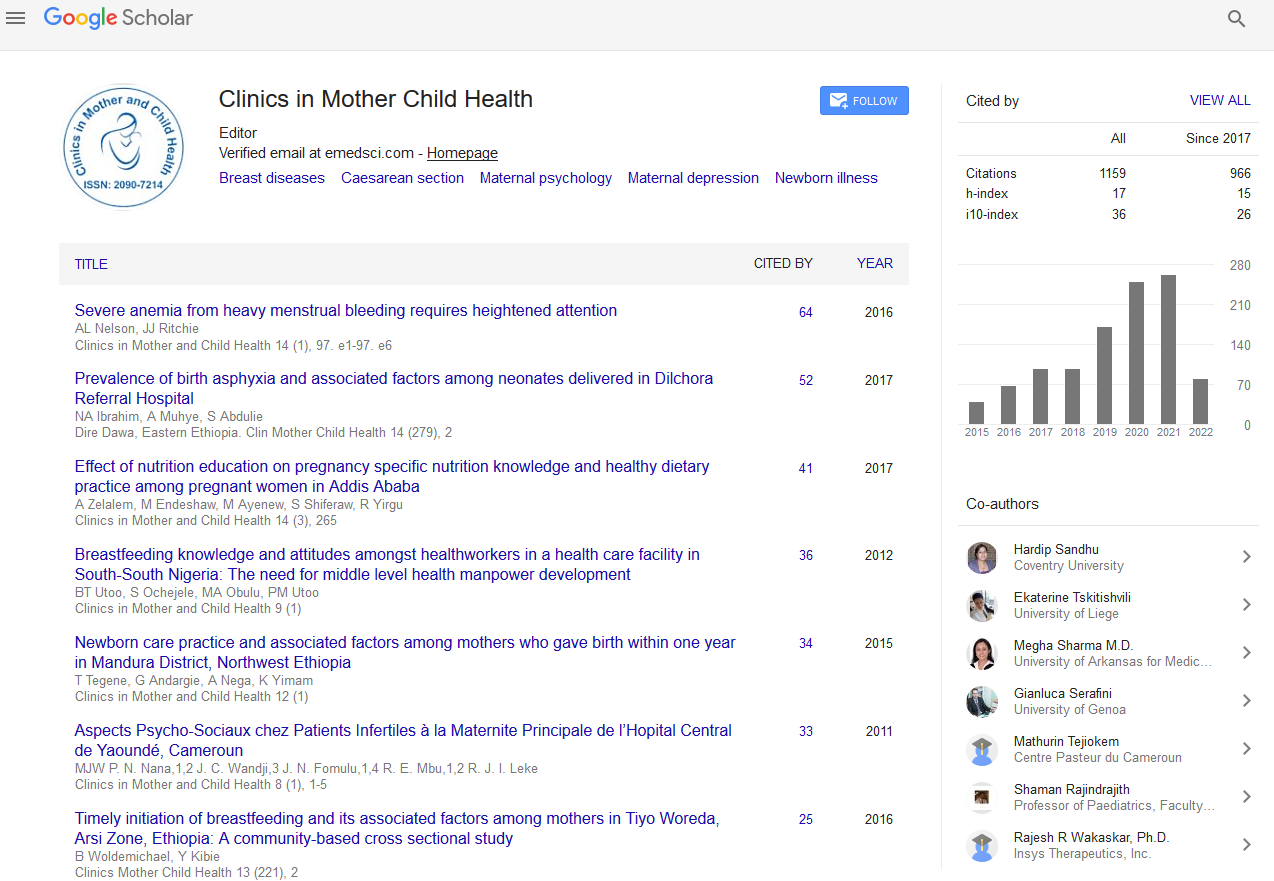
All included women had a transvaginal ultrasound performed after instructing the patient to evacuate the bladder. The ultrasound set used was (7.5 MHz transvaginal transducer with color Doppler facilities (Voluson 530-D Medison).Measurements of dimension of the uterus (sagittal, transverse) sections were performed in addition to comment on:Position.Endometrial thickness measured in sagittal section.Myometrial fibroids or adenomyosis.Endometrial polyps, thickness and irregularities. Adenexa and any abnormalities as ovarian cysts. Comment on IUCD: including site, displacement, partial expulsion, partial perforation, embedding (Figure 1).
Figure 1: Blood flow indices of the uterine artery.
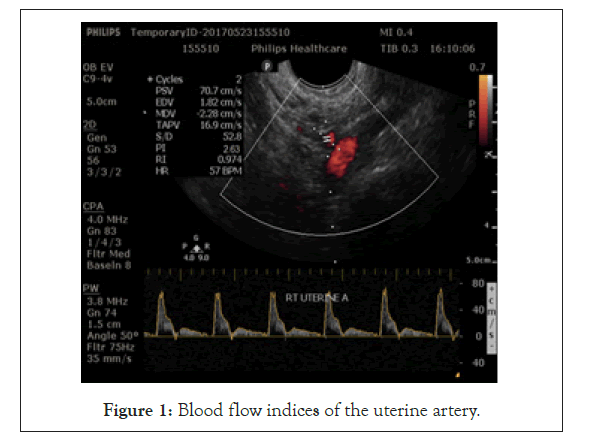
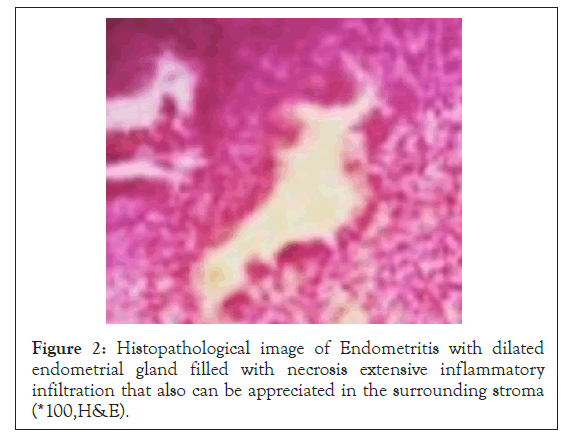
The IUCD was detected by its echogenicity compared to the normal endometrium. The sonographic appearance of an IUCD is determined by its shape and composition. Intrauterine contraceptive devices are made of a combination of plastic and metal (copper). The metal causes a “reverberation artifact” a series of parallel lines that become progressively weaker posterior, when the IUCD is parallel to the ultrasound beam Plastic tubing is displayed as 2 parallel lines representing an entrance and an exit shadow. A normally positioned IUCD lies in the midline of the endometrial canal, equidistant from the uterine margins (Figures 2 and 3).
Figure 2: Histopathological image of Endometritis with dilated endometrial gland filled with necrosis extensive inflammatory infiltration that also can be appreciated in the surrounding stroma (*100,H&E).
Figure 3: Histopathological image of Endometroid type of endometrial adenocarcinoma composed of malignant epithelial cell infiltrating the stroma and showing pleomorphic hyperchromatic nuclei with mitosis and extensive necrosis(x 400,H&E).
After identification of the IUCD within the uterine cavity the distance between the top of the vertical arm of the device to the endo-myometrial junction (IUCD myometrium) was measured.
Blood flow indices of the uterine artery
Transvaginal probe is placed in the anterior fornix , moved laterally to visualize the paracervical vascular plexus, Color Doppler is turned on and the uterine artery is identified as it turns cranially to make its ascent to the uterine body. Measurements are taken at this point, before the uterine artery branches into the arcuate arteries. The same process is repeated on the contralateral side (Figure 4).
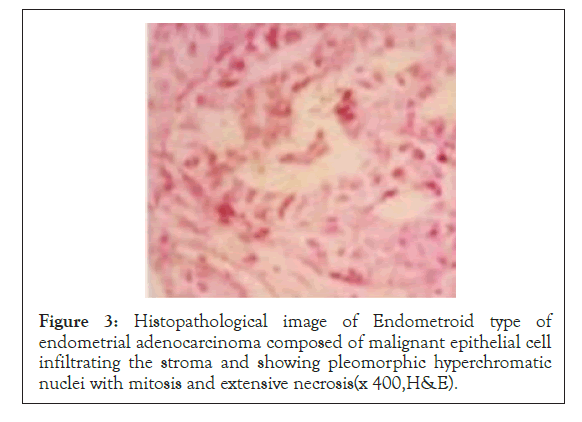
Figure 4: Histopathological image of low grade Endometrial Stromal sarcoma composed of atypical stromal cell proliferation of atypical spindle cells with pleomorphic hyperchromatic nuclei with mitosis and necrosis(*×400,H&E).
Blood flow indices of the uterine artery; the Pulsatility Index (PI) and the Resistance Index (RI) were calculated according to the following equations: PI=(A–B)/mean, and RI=(A–B)/A, where A is the peak systolic, B is the end-diastolic Doppler shift, and mean is the mean maximum Doppler shift frequency taken over the cardiac cycle. The mean PI and RI were calculated by combining three waveforms of the left and right uterine artery and were used for subsequent statistical analysis.
Statistical analysis
Data were entered checked and analyzed using Epi-Info version 6 and SPP for Windows version 8.
Results
This prospective clinical study included 120 women who have been wearing an IUD for at least 6 months, presenting to Outpatient Gynecologic Clinic at Zagazig University Hospital. The study included 120 women, divided into three groups.
• Group I included 40 women using copper intrauterine device (TCu-380A) and complaining of menorrhagia or menometrorrhagia.
• Group II included 40 women using CIUD and not complaining of abnormal uterine bleeding.
• Group III included 40 women complaining of vaginal discharge or requesting CIUD insertion, and not complaining of abnormal uterine bleeding as a control group.
In our study, there were no significant statistical differences between the studied groups concerning age, parity ,duration and timingof IUD insertion (Tables 1 and 2). There were no statistically significant differences between groups concerning uterus dimensions and endometrial thickness measure by TVS (Table 3). RI was significantly lower in women of group I than in women of groups II and III (p<0.001) ,PI was significantly lower in women of group I than in women of groups II and III (p<0.001) (Table 4). At a cutoff value of 2, PI has a sensitivity of 90% and specificity of 92.5% and RI at a cutoff value of 0.7 has a sensitivity of 80% and specificity of 87.5% in predicting induced uterine bleeding (Tables 5 and 6).
| Age (Years) | Group I (n=40) | Group II (n=40) | Control (n=40) | F | p | |||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | 29.1 ± 4.9 | 28.4 ± 4.4 | 28.8 ± 6.1 | 0.07 | 0.9 (NS) | |||
| Range | 20-35 | 23-35 | 20-35 | |||||
| Parity | Group I (n=40) | Group II (n=40) | Control (n=40) | X2 | p | |||
| No | % | No | % | No | % | |||
| ≤ 2 | 15 | 75 | 16 | 80 | 13 | 65 | 0.48 | 0.7 (NS) |
| > 2 | 5 | 25 | 4 | 20 | 7 | 35 | ||
| Duration of IUD use (months) | Group I (n=40) | Group II (n=40) | Control (n=40) | F | p | |||
| Mean ± SD | 49.9 ± 22 | 44.1 ± 18.6 | 48.8 ± 18 | 0.4 | 0.62 (NS) | |||
| Range | 6 to 80 | 6 to 80 | 6 to 80 | |||||
Table 1: Difference between the studied groups concerning mean age, parity and duration of IUD insertion.
| Postpartum | Post-abortion | Postmenstrual | X2 | p | ||||
|---|---|---|---|---|---|---|---|---|
| No | % | No | % | No | % | |||
| Group I | 20 | 50 | 4 | 10 | 16 | 40 | 0.39 | 0.82 (NS) |
| Group II | 22 | 55 | 2 | 5 | 16 | 40 | 0.11 | 0.94 (NS) |
| Control | 20 | 50 | 2 | 5 | 18 | 45 | - | - |
Table 2: Difference between the studied groups concerning timing of IUD insertion (analysis using Chi-square test).
| Group I Mean ± SD | Group II Mean ± SD | Control (Mean ± SD) | F | P | |
|---|---|---|---|---|---|
| Uterus length (mm) | 76.4 ± 9.6 | 81.7 ± 14.1 | 82.6 ± 12.6 | 1.49 | 0.23 (NS) |
| Width (mm) | 48.5 ± 13.8 | 49.1 ± 12.7 | 46.9 ±11.68 | 0.15 | 0.85 (NS) |
| Endometrial thickness (mm) | 8.1 ± 1.1 | 7.9 ± 1.6 | 7.6 ± 2 | 0.48 | 0.61 (NS) |
Table 3: Difference between the studied groups concerning uterus dimensions and endometrial thickness measured by TVS (analysis using one-way anova test).
| RI | Group I Mean ± SD | Group II Mean ± SD | Control (Mean ± SD) | F | P |
|---|---|---|---|---|---|
| Mean ± SD | 0.69 ± 0.07 | 0.79 ± 0.1 | 0.82 ± 0.12 |
15.69 |
<0.001 (HS) |
| Range | 0.59-0.8 | 0.6-0.89 | 0.61-0.9 | ||
| PI | Group I Mean ± SD | Group II Mean ± SD | Control (Mean ± SD) | F | P |
| Mean ± SD | 1.9 ± 0.05 | 2.2 ± 0.269 | 2.3 ± 0.25 |
13.7 |
<0.001 (HS) |
| Range | 1.65-2.42 | 1.87-2.63 | 1.89-2.65 |
Table 4: Comparison between the RI of the women of the three groups.
| Cutoff | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | |
|---|---|---|---|---|---|---|
| PI | 2 | 90 | 92.5 | 85.7 | 94.9 | 91.7 |
| RI | 0.7 | 80 | 87.5 | 76.2 | 89.7 | 85 |
Table 5: Validity of PI and RI in prediction of induced uterine bleeding.
| Area | Std. Errora | Asymptotic Sig.b | Asymptotic 95% Confidence interval | |
|---|---|---|---|---|
| Lower bound | Upper bound | |||
| 0.903 | 0.051 | 0 | 0.802 | 1.004 |
Table 6: ROC curve of PI for prediction of induced uterine bleeding.
Discussion
The objectives of our study were to evaluate the prediction between abnormal uterine bleeding in IUD users and uterine artery Doppler [Pulsitility Index (PI); Resistant Index (RI)] using transvaginal ultrasound and Doppler. We found in our study that RI and PI were significantly lower in women using CIUD and complaining of abnormal uterine bleeding (indicating increase in the uterine blood flow) than in women using CIUD and not complaining of abnormal uterine bleeding and women not using CIUD. In our study, there were no significant statistical differences between the studied groups concerning age, parity and duration of IUD use. Our results are in agreement with Vercellini, et al. stated during his work on the levonorgestrel IUD that there is no correlation between endometrial thickness and days of bleeding or spotting observed in both groups [5] (Figure 5).
Figure 5: Figure showing ROC curve of RI for prediction of induced uterine bleeding.
On the other hand in our study, RI and PI were significantly lower in women of group I (women using CIUD and complaining of abnormal uterine bleeding) than in women of group II(women using CIUD and not complaining of abnormal uterine bleeding) and group III (control group) (p<0.001).Our results are correlated with Momtaz et al. They measured the PI and RI of uterine arteries in 68 women, including 44 using intrauterine contraceptive device and 24 control women who were not using a method of contraception. Both the PI and RI were significantly lower in women with CIUD-induced bleeding than in those using CIUD and not complaining of abnormal vaginal bleeding. In addition, there were no statistically significant differences in PI and RI between women using CIUD without complaining of abnormal vaginal bleeding and women in the control group.
They reported that the PI was less than 2 in women with CIUD- induced bleeding, while the mean PI in women using IUD without complications was 2.38 with the lowest PI being 1.98 [6] Frajndlich et al. measured resistance and Pulsatility indices in 101 women, 74 of whom were using an intrauterine contraceptive device, and 27 controls, who were not using any contraceptive method. The intrauterine contraceptive device users were divided into three groups: those with normal bleeding (n=34); those with abnormal uterine bleeding without medication (n=16); and those with abnormal bleeding corrected with use of prostaglandin inhibitors (n=24). The resistance and Pulsatility values were significantly lower in the group of women using intrauterine contraceptive devices who had abnormal bleeding than in all other groups. A Pulsatility index of less than 2 may be associated with a higher risk for development of intrauterine contraceptive device-induced bleeding [7]. Yigit et al. measured PI, RI, and systole/diastole ratio(S/D) in the uterine artery and its myometrial branches in 28 patients before and after the insertion of CIUD. They reported that the PI and S/D values in the uterine artery increased significantly after the insertion of the CIUD (p<0.05).`
Patients with increased bleeding scores after insertion of CIUD had significantly lower uterine artery PI compared with those without increased bleeding scores (p<0.05). They concluded that low uterine artery PI values recorded in the early phase of the menstrual cycle in patients with a CIUD were associated with an increased bleeding risk [8] In contrast to our results, Other study measured the PI and RI in 100 patients before and 30 days after the insertion of CIUD, no statistically significant changes in PI and RI values were detected [9] Jimenez et al. reported that there were no statistically significant differences in PI and RI between women with IUD-induced bleeding and women using IUD with normal menstruation [10].
There are several mechanisms explaining the association between the increase in the uterine blood flow (as indicated by decreased PI and RI in the uterine artery) and the increase in menstrual blood loss. It has been suggested that metrorrhagia, may be caused by increased uterine secretion of prostanoids leading to an increase in vascularity, vascular permeability, and inhibition of platelet activity [11].Concerning the effect of IUD on the biosynthesis of prostaglandins in the endometrium, Xin et al. found that there was overexpression of mRNA and protein of COX-2 enzyme leading to overproduction of prostaglandins in the endometrium after the insertion of CIUD [12] Other vasoactive substances may also be involved, including nitric oxide (NO) which is a potent vasodilator produced by the vascular endothelium. NO is present in the human endometrium and myometrium. There is evidence that NO may play a part in acute and chronic inflammation [13].
The introduction of an intrauterine device into the uterine cavity induces a foreign body reaction in the surrounding endometrium. NO is present in the foreign body inflammatory reaction around loosened joint replacement implants. Thus, it is possible that IUD also induces NO synthesis in the surrounding tissue. There is also a connection between NO synthesis and prostaglandin synthesis. NO directly interacts with cyclooxygenase, which is responsible for prostaglandin synthesis and causes an increase in enzymatic activity [14].There are also other possible mechanisms explaining the association of the PI of uterine artery with menstrual blood loss. Women with menorrhagia show a significant increase in endothelial cell proliferation, reflecting disturbed angiogenesis. It is possible that there are also other vascular abnormalities resulting from disturbed angiogenesis. In abnormal vessels, poor contractibility and dysfunction of the hemostatic system may cause menorrhagia and decreased impedance [15]. Xin et al. reported that the expression of vascular endothelial growth factor (VEGF) and its receptor, kinase insert domain containing receptor (KDR) and micro vessel density (MVD) were increased in the endometrium after using CIUD [16].
Jimenez et al. used power Doppler analysis as well as Resistance Index (RI) and Plasticity Index (PI) to quantify the Sub endometrial micro vascularization and uterine artery blood flow in patients with IUD-induced side effects (LNG-IUS and TCu 380A). They concluded that Sub endometrial vascularization was increased in patients with IUD-induced side effects, controlling for IUD type, age and parity. This method could be used as a prognostic factor to better evaluate those patients at risk of developing severe dysmenorrhea and/or excessive bleeding after IUD insertion [10] On the basis of these observations and our present study, it is possible that CIUD induces changes in the production of prostaglandins and stimulates angiogenesis in the endometrium leading to an increase in the uterine blood-flow.
Conclusion
The results of our study confirm the hypothesis that there is an increase in the uterine blood flow (indicated by decreased PI and RI in the uterine artery) in patients with CIUD-induced abnormal uterine bleeding. The uterine artery Doppler could be used to identify patients at risk of developing excessive bleeding after copper IUD insertion.
REFERENCES
- Nelson A, Grimes D, Arias R, Shulman L, Moore A. Intrauterine copper contraceptive: update and opportunities. OBG Management. 2006;12(6):1-8.
- Munro MG. Abnormal uterine bleeding. Cambridge University Press. London. United Kingdoms. 2010.
- American College of Obstetricians and Gynecologists
- Nicolaides K, Papageorghiou A. The role of uterine artery Doppler in predicting adverse pregnancy outcome. Best Practice & Research Clinical Obstetrics and Gynecology. 2004;18(3):383-396.
- .Ultrasonography. ACOG Technical Bulletin Number 191. Int J Gynaecol Obstet. 2012;45(2):175-180.
- Doppler in predicting adverse pregnancy outcome. Best Practice & Research Clinical Obstetrics and Gynecology. 2004;18(3):383-396.
- Vercellini P, Cortesi I, Oldandi S, MoschettaM, Giorgi OD, Crosignani PG, et al. The role of transvaginal ultrasonography and outpatient diagnostic hysteroscopy in the evaluation of patients with menorrhagia, Hum Reprod. 1997;12(8):1768-1771.
- Momtaz M, Zayed M, Rashid K, Idriss O. Doppler study of the uterine artery in patients using an intrauterine contraceptive device. Ultrasound Obstet Gynecol. 1994;4(6):230-231.
- Frajndlich R, von Eye Corleta H, Frantz N.Color Doppler sonographic study of the uterine artery in patients using intrauterine contraceptive devices. J Ultrasound Med.2000;19(8):577-579.
- Yigit N, Kacar M, Yigit H,Kosar P,Kosar U. The effects of copper contraceptive intrauterine device on the uterine blood flow: A prospective transvaginal Doppler study. J Clin Ultrasound. 2009;37(7):380-384.
- De Souza MA, Geber S.Doppler color flow analysis of the uterine arteries before and after intrauterine device insertion: A prospective study. J Ultrasound Med. 2006;2(6)5:150-153.
- Jimenez MF, Vetori D, Fagundes PA, Freitas FM, Joao SLCH. Subendometrial microvascularization and uterine artery blood flow in IUD-induced side effects (levonorgestrel intrauterine system and copper intrauterine device). Contraception.2008;78(4):324-327.
- Smith OP, Jabbour HN, Critchley HO. Cyclooxygenase enzyme expression and E series prostaglandin receptor signalling are enhanced in heavy menstruation. Hum Reprod. 2007;22(5): 1450-1456.
- Xin ZM, Cao LM, Xie QZ, Sin Y,Chun-Su Y, Guo YH. Effects of the copper intrauterine device on the expression of cyclooxygenase-1 and -2 in the endometrium. Int J Gynaecol Obstet. 2009; 105(2):166-1668.
- Laroux FS, Lefer DJ, Kawachi S, Scalia R, Gray L, Grisham B, et al. Role of nitric oxide in the regulation of acute and chronic inflammation. Antioxid Redox Signal. 200;2(3):391- 396.
- Xin ZM, Xie QZ, Cao LM, Sun YP, Su YC, Guo YH. Effects of intrauterine contraceptive device on expression of vascular endothelial growth factor, kinase insert domain-containing receptor and microvessel density in endometrium. Zhonghua Fu Chan Ke Za Zhi. 2004;39(11):771-775.
Citation: Gobran MA, El Hanafy SM, Elnagar WM, Ahmed AMA, Abdelrhman AA, Lashin ME, et al. (2021) Evaluation of Predictive Value of Uterine Artery Doppler Indices versus Histopathology Sampling in Detection of Abnormal Uterine Bleeding in Intrauterine Contraceptive Device Users. Clinics Mother Child Health. 18:382.
Copyright: © 2021 Gobran MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.