PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 11, Issue 6
Ethical Considerations for the Cancellation of Non-Urgent Surgeries during the COVID-19 Pandemic and Suggestions for Future Health Crises
Nolan J. Brown1*, Stephen Szabadi2, Cameron Quon2, Nathan A Shlobin3, Brian V Lien1, Shane Shahrestani4, Katelynn Tran5, Ali R. Tafreshi6, Seth C Ransom7, Alexander Himstead1, Celina Yang1, Ryan C Ransom8, Ronald Sahyouni9 and Aaron Kheriaty102Department of Neurosurgery, Western Michigan University Homer Stryker M.D. School of Medicine, Kalamazoo, Michigan, USA
3Department of Neurological Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
4Department of Neurosurgery, Keck School of Medicine of USC, Los Angeles, California, USA
5Department of Neurosurgery, University of Southern California, Los Angeles, California, USA
6Department of Neurological Surgery, Geisinger Commonwealth School of Medicine, Danville, PA, USA
7Department of Neurosurgery, University of Arkansas for Medical Sciences, Little Rock, Arkansas, USA
8Department of Neurologic Surgery, Mayo Clinic Alix School of Medicine, Rochester, MN, USA
9Department of Neurological Surgery, University of California, San Diego, San Diego, CA, USA
10Department of Psychiatry and Human Behavior, University of California Irvine, Irvine, California, USA
Received: 10-Nov-2020 Published: 01-Dec-2020, DOI: 10.35248/2155-9627.20.11.365
Abstract
In light of the national emergency the pandemic has spawned, hospitals across the United States made the decision to cancel non-urgent surgeries to free up resources and personnel and protect healthcare workers, patients, and the public from further spread. By one estimate, the initial wave of COVID-19 will lead to 28 million surgeries being postponed worldwide, with 343,670 projected cancellations each week in the USA alone over the course of a 12-week peak. This is an unprecedented disruption in the modern system of healthcare delivery that has the potential to produce long-lasting deleterious effects and troublesome ethical dilemmas.
Keywords
Pandemic; Non-urgent surgeries; Healthcare delivery; Ethical dilemmas
Introduction
Novel Coronavirus Disease 2019 (COVID-19) is caused by infection from the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which began in Wuhan, China, and has now reached over 2.8 million cases globally [1].
Existing literature discusses guidelines for resuming non-urgent elective surgeries, ethical considerations in rationing lifesaving resources, protocols and clinical decision flowcharts for reducing non-urgent elective surgery risk, strategies to increase surge capacity, and predictive modeling for healthcare resource usage. However, literature that considers the ethical and practical benefits and associated drawbacks of postponing non-urgent elective surgeries in the context of the four fundamental principles of medical ethics beneficence, non-maleficence, justice, and autonomy–is lacking [2-15].
We further aim to address the ethical benefits and drawbacks of proposed decision-making algorithms for non-urgent elective surgery during COVID, using as a representative example the triage protocol devised by Stahel (Figure 1). While COVID-19 specific, this scheme could be generalized to future pandemics as an algorithm that is based on surgical indications (Table 1), perioperative resource utilization (predicted blood product transfusion requirements, postoperative length of stay, the need for extended ventilation), and projections for postoperative ICU admissions. We assert that while Stahel’s triage protocol is an excellent starting point for the ethical application of non-urgent elective surgery restrictions during a pandemic, modifications which may further align decision making with the tenets of beneficence, non- maleficence, justice, and autonomy are necessary [16].
| Indication | Urgency | Case examples |
|---|---|---|
| Emergent | <1 h | • Life-threatening emergencies • Acute exsanguination/hemorrhagic shock • Trauma level 1 activations • Acute vascular injury or occlusion • Aortic dissection • Emergency C-section • Acute compartment syndrome • Necrotizing fasciitis • Peritonitis • Bowel obstruction/perforation |
| Urgent | <24 h | • Appendicitis/cholecystitis • Septic arthritis • Open fractures • Bleeding pelvic fractures • Femur shaft fractures and hip fractures • Acute nerve injuries/spinal cord injuries • Surgical infections |
| Urgent-elective | <2 weeks | • Cardiothoracic/cardiovascular procedures • Cerebral aneurysm repair • Vascular access devices • Skin grafts/flaps/wound closures • Scheduled C-section • Closed fractures • Spinal fractures and acetabular fractures |
| Elective (essential) | 1-3 months | • Cancer surgery and biopsies • Subacute cardiac valve procedures • Hernia repair • Hysterectomy • Reconstructive surgery |
| Elective (discretionary) | >3 months | • Cosmetic surgery • Bariatric surgery • Joint replacement • Sports surgery • Vasectomy/tubal ligation • Infertility procedures |
Table 1: Examples of surgical case types stratified by indication and urgency.
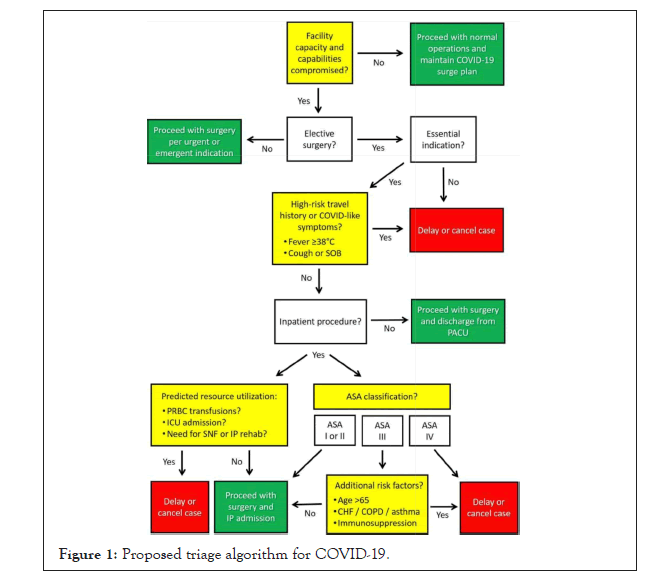
Figure 1: Proposed triage algorithm for COVID-19.
Materials and Methods
The four pillars of medical ethics
There has been no better time than the current pandemic for physicians to embrace principles such as beneficence, which reminds us that the ultimate purpose of health care is to aim for net patient benefit; non-maleficence, which reminds physicians to “do no harm”; justice, which emphasizes the need for equitable treatment of all patient groups; and, autonomy, which calls for respecting each patient and their individual rights, thoughts, and intentions. In the ethical analysis that follows, each of these tenets will be examined with respect to COVID-19 and the unique implications of deferring non-urgent surgeries. Ultimately, our hope is that this discussion will help guide responses to future pandemics [17,18].
Beneficence
In the United States, many physicians and hospitals have followed the Surgeon General’s guidelines to postpone non-essential medical, surgical, and dental procedures, which has helped make available healthcare workers who have been needed to help combat the pandemic and preserved scarce PPE supplies. In line with CNS administrator Seema Verma’s recommendations, procedures that have been deferred include Tier 1a (e.g., carpal tunnel releases and cataract surgeries) and Tier 1b (e.g., endoscopies), while Tier 2a (e.g., low risk cancer, non-urgent spine and orthopedic procedures) and Tier 2b (e.g., same as Tier 2a but with regards to unhealthy patients) have been considered on a case-by-case basis. Along these lines, the meaning of “non-urgent” has been defined by the physician but points towards “not immediately limb- or life-threatening”. Regarding the principle of beneficence, cancelling such procedures has allowed healthcare workers to provide better care of COVID-19 patients under limited resources and has supported social distancing measures, potentially curbing COVID-19 mortality [9-11].
This would seem to align with the principle of beneficence, but the matter is complicated, as delaying all or most non-urgent elective surgeries could also result in cumulative downstream effects which may seriously harm patients. Many elective surgical cases that meet the immediate criteria for non-urgency may actually involve significant morbidity if delayed, with one estimate projecting a significant negative outcome in greater than 50% such cases. For example, the Naval Medical University in China has reported the risks of delaying surgery for colorectal cancer, citing this action as a ticking time bomb. Additionally, a global predictive model for elective surgery delay estimated that it would take a median of 45 weeks to clear the backlog of elective surgical cases, assuming an optimistic 20% increase in case turnover post-pandemic. It would be reasonable to assume that a significant number of previously non-urgent surgical cases may become urgent after such a prolonged delay.
Is a blanket policy of non-urgent elective surgery delay promoting beneficence in real-world practice? Prioritizing patients with one particular ailment over another, in this case COVID-19, irrespective of total morbidity does not appear to be in line with providing the greatest net benefit for the largest number of patients. Fear surrounding the COVID-19 pandemic could also be introducing bias into clinical and ethical decision making in a misguided attempt to conserve scarce resources. When examining the rationale behind decisions to postpone or deny certain non-urgent procedures, a bias among clinicians to attribute decision making to the saving of resources has been observed, even when following established clinical guidelines would have yielded the same decision. Granted, the goal of postponing non-urgent elective surgeries is not only to save resources for the patients affected by COVID-19 themselves, but also to slow the spread and reduce risk to the general public, non-infected patients, and healthcare workers.
Both postponing and not postponing non-urgent elective surgeries involve hard to calculate long term risks to public health. Such risks must be weighed carefully against one another in real time, using a framework that is adaptable to local healthcare resource strain, infection rates, patterns of transmission, and the unique needs of regional patient populations. Existing triage schemes, like the one proposed by Stahel, primarily focus on proper patient selection in regard to COVID-19 infection risk and surgical severity to arrive at a go/no-go decision. We contend that to better guarantee beneficence the decision matrix should be scaled up and down using predictive demand modeling in order to better adapt to local conditions. Researchers at the University of Pennsylvania have developed a predictive algorithm called CHIME (COVID-19 Hospital Impact Model for Epidemics) which uses several measures of population size, hospital resource availability, and community viral transmission to make short-term local predictions for healthcare strain. Using predictive models such as CHIME in the implementation of Stahel’s triage scheme could increase beneficence by basing the criteria for elective surgery postponement on real-time actionable measures of health system burden and local risk of viral spread rather than more nebulous assumptions of system-wide risk [19].
However, the usefulness of predictive algorithms like CHIME are inherently limited by the rapid pace at which local regulations and physical distancing requirements change. Other measures of the ability of healthcare systems to accommodate non-urgent elective surgeries have been proposed, with the FACS offering as a heuristic the decrease in COVID-19 incidence for 14 days before resuming surgeries. By increasing the flexibility of decision algorithms, fewer non-urgent elective surgeries could be postponed unnecessarily, and vice versa, perhaps even a greater number of non-urgent elective surgeries could be postponed when real-time measures of healthcare strain deem it necessary. Could some of these non- urgent elective surgeries lead to adverse outcomes directly related to COVID-19? We reiterate that this is not ideal, but the value of ethics is to provide guidance in non-ideal situations, that is to say, under conditions of uncertainty [20,21].
Results and Discussion
Non-maleficence
Bringing patients into a health care facility for the purpose of surgery is a means by which they may become infected or expose those around them to COVID-19. The principle of non- maleficence, often referred to as the “do no harm” principle, argues that any procedure whose anticipated harms outweigh the anticipated benefits should not be performed. With respect to COVID-19, suspending non-urgent elective procedures can certainly minimize iatrogenic transmission; in fact, a recent study found that 41% of COVID-19 infections in China were hospital acquired. Furthermore, when Sierra Leone’s Connaught hospital cancelled non-urgent procedures during the 2014 Ebola outbreak, it never experienced as high a rate of worker deaths as it did before the cancellations.
However, in the context of a pandemic, the principle of non- maleficence extends well beyond a singular patient, as the premature lifting of restrictions (including restrictions on non-urgent elective surgery) can spur subsequent waves of infection. We must also consider harm as it applies to healthcare workers, the public at large, and other patients, both in the present and future. When viewed in a more global system-wide context, harm may be delayed and difficult to trace. For example, a direct relationship between a ventilator made available for a person undergoing a non-urgent elective surgery and the death of a COVID-19 patient because a ventilator wasn’t available may be hard to establish. Additionally, haphazardly performing non-urgent elective surgeries may not only harm patients directly, but also may harm healthcare workers themselves, potentially remove hard to replace workers from our health infrastructure which would lead to a significantly greater number of patient deaths in the future [21-26].
Stahel’s triage protocol attempts to reduce harm to all groups involved by stratifying known risks, both of the potential harm to the prospective elective-surgery recipient by stratifying clinical urgency, and to other patients, healthcare workers, and the public health infrastructure as a whole by evaluating viral transmission risk and anticipated resource utilization. We contend that Stahel’s protocol is an excellent starting point to ensuring non-maleficence, to which could be added additional measures of risk and strategies to prevent harm, such as telehealth prescreening, tailoring surgical techniques to prevent viral spread through minimizing the production of aerosols, regimented testing protocols before surgery, alternative anesthesia protocols to reduce healthcare worker exposure, and protocols to reduce post-operative coughing and nausea which may further viral spread. Underlying all of these preventative measures is the necessary assumption that every patient is potentially Sars- CoV-2 positive. We find that in the scope of non-maleficence, delaying non-urgent elective procedures is often an ethically sound decision, though perhaps not invariably [2-4].
Justice
In late-March 2020, medical centers near each other in California were operating on different protocols in regards to the decision to perform non-urgent elective procedures. This situation requires us to ask: how can physicians deny non-urgent elective procedures to patients at one facility when they are accepted at another? This does not appear to comply with the principle of justice, which demands equitable treatment across patient groups. Standardized triage protocols such as Stahel’s attempt to promote justice by adding an objective criteria of risks to make decisions more uniform and avoid such discrepancies in care.
Vital to maintaining justice in the formulation and implementation of triage protocols is that the criteria are transparent, responsive to the general will of the public, and first and foremost based on medical merit17, not solely on the conservation of resources. Transparency is fundamental in ensuring public trust in the healthcare system; it minimizes harm to those patients who may be denied elective surgery and reduces moral injury to physicians who might otherwise need to make hasty clinical decisions based on vague guidelines from governmental and professional entities. Triage algorithms are effective at differentiating between groups of patients, but inevitably, when resource availability is significantly impacted, there will be less resources than needed even for those patients who are not screened out using available triage schemes.
This creates its own unique dilemma. For example, how can justice be maintained in performing only 7 knee arthroscopies when 35 need to be performed? Existing literature on medical ethics contains many different methods of making the difficult task of rationing care between patients with similar clinical need more objective, for example by adopting a first-come-first-served model, prioritizing social usefulness, or using a lottery system29. Ultimately whatever criteria are employed must reflect the will of the people to be legitimate and just16. However, there are times when adhering to public perception may not promote justice.
When COVID-19 made waves in late-March, some institutions were continuing with what many laypeople would consider undeniably non-urgent operations, such as cosmetic surgeries. However, with a few notable exceptions, cosmetic surgeries are generally considered safer than many other non-urgent elective procedures because they are fairly low complexity, short in duration, and are usually performed on healthy patients22. With the use of appropriate patient selection controls, free-standing ambulatory surgical centers30, and additional measures during surgery to prevent viral transmission such as avoiding invasive intubation when possible21, is it not unjust to arbitrarily delay such surgeries across the board simply because of perceived unimportance? Such procedures would not be performed across all institutions if a protocol akin to Stahel’s was strictly implemented across the entire healthcare system. Proponents of such an approach point to the lack of immediate harm from postponement; according to the surgery department chair at Brigham and Women’s Hospital, Dr. Gerard Doherty, 25% of surgeries are non-urgent and could be postponed without harm. This alone could make a significant difference during a pandemic in curbing transmission. According to Doherty, for the 50% of operations that fall in the grey area (cancer-related procedures), they can proceed as determined by a standard protocol [13].
Indeed, some measure of uniformity and equal implementation across systems is necessary to maintain justice and public legitimacy. Even the definition of what is considered “elective” varies highly between areas of the country, with Alaska determining it as simply something that is not planned in advance. Similarly, enforcement of non-urgent elective surgery guidelines can vary widely between threats of large fines and criminal conviction (e.g., Maryland) and non-regulatory guidance. Ambiguity between institutions and geographical areas has brought about public scrutiny.
However, the principle of justice is not absolute, and must be balanced against the other principles of medical ethics, especially beneficence. Substantial differences in the clinical criteria for surgery postponement between institutions or geographical areas might lead to less surgeries being postponed, but also introduces a injustices. Simply performing more elective surgeries in locations with lower viral spread may be inherently unjust because individuals with the same medical need will receive different levels of care only based on factors outside of their control, such as where they reside. Even though local variances in healthcare capacity should be considered, patient populations do not exist in a vacuum. Ultimately, a global view of resource allocation is also needed; one patient’s actions affect another’s. Indeed, the increase in population growth, ease of movement, interdependence of modern society, and use of advanced medical technology has limited what medical resources one individual can rightfully call their own17.
We contend that justice need not entail a blanket application of restrictions which unduly restrict certain patient groups from elective surgeries, but rather promote a more equal opportunity to receive those surgeries where they may safely be performed. Stahel’s triage scheme does not account for the status of regional health infrastructure resource utilization. Perhaps a state or county wide authority could organize the secure transfer of patients who need non-urgent elective surgery to institutions that are not as heavily affected, or with enhanced screening create a COVID-free surgery pipeline using available ambulatory surgery centers to avoid strain on traditional hospitals14. Adopting this approach introduces a level of control that lies between local and system-wide attempts to balance the differing availability of resources with the need for equal standards of treatment. However, we argue that some aspects of decision making surrounding non-urgent elective surgery delay, such as the very definition of what is “elective”, should be standardized across the entire system. Guidelines that are too vague cause concern among doctors who are required to interpret them32, as well as diminish the legitimacy of the healthcare system as a whole in the eyes of the public. To create a standardized system of elective surgery patient transfer to less impacted institutions, the limitations of individual insurance networks, contractual agreements between payers, and regional variances in healthcare policy would have to be overcome. But this might prove to be a worthwhile effort in promoting justice in surgical resource allocation during COVID-19 and in future pandemics.
Autonomy
Patient autonomy and the trust it fosters is crucial to the delicate physician-patient relationship. Although some hospital systems may not be limited on resources, others are experiencing resource shortages which could have life-or-death implications for those suffering from COVID-19. The pandemic has changed many standard practices relating to patient autonomy, including the privacy of patient medical records and the principle of informed consent. For example, pre-procedure informed consent counseling before non-urgent elective surgeries performed during the COVID-19 pandemic has changed to include the unique risks patients may face, including possible exposure to COVID-19, in order to fulfill the principle of autonomy. At the outset, the decision to continue with non-urgent elective procedures maintains patient autonomy. However, respect for autonomy alone is never a definitive reason to make a medical decision; it is merely a constraint on the means by which physicians may operate, and a principle which preserves informed consent and shared decision making. Patient autonomy as it relates to shared decision making has taken on particular importance in the COVID-19 pandemic, where some patients have requested popular but unproven treatments, like hydroxychloroquineCITE, which may cause significant harm. Ultimately, autonomy is not absolute and must be balanced against the broader needs of public health [27-29].
Therefore, physicians can justifiably postpone a non-urgent elective procedure, especially those of the Tier 1a and 1b categories considering the COVID-19 pandemic. Patient autonomy alone does not demand that such procedures be performed, especially when doing so could significantly increase adverse outcomes, such as exposing patients to infections, draining limited resources and PPE, and requiring the time of healthcare workers who could otherwise assist in combating COVID-19. Stahel’s criteria helps make these decisions more transparent and ethically sound by removing bias from decision making and promoting a more ethical distribution of available surgical resources, providing a clear framework for evaluating when a patient’s right to autonomy does or does not trump the needs of public health, and vice versa.
As we previously discussed, allowing for more flexibility based on regional strain may increase patient autonomy, which may be made possible by making such guidelines non-regulatory in nature. This preserves the autonomy of physicians to work with regional experts to tailor those guidelines more specifically to the unique needs of their patient population, which in the end increases the autonomy of the patient. It is important to mention that increasing patient autonomy may in some cases actually lead to decreased strain on the healthcare system. Notably, for cases which have been more difficult to classify as urgent or non-urgent (Tier 2a and 2b procedures), voluntary cancellations by patients have served as a self-regulating mechanism that has reduced the number of operations during COVID-19. That is, when a valid triage protocol is followed and the outcome is that the decision is placed in the patients’ hands, the number of operations conducted will likely be less than the number offered. This self-regulatory mechanism does not violate any autonomy principles and further validates the use of standardized triage protocols like those developed by Stahel, although in a non-regulatory manner [30-32].
Conclusion
After carefully considering each of the four ethical principles of medicine, we find justification for the temporary postponement of non-urgent elective procedures during pandemics while also acknowledging the unanticipated harms of doing so. In times of major healthcare crises, it is key to balance the allocation of resources towards the prevention of possible widespread mortality through the spready of infection, but also towards diminishing morbidity regardless of the causative factor, which may include performing non-urgent elective surgeries. Although such unilateral cancellations are not unprecedented, such as the case with both the 2009 H1N1 pandemic and 2014 Ebola epidemic, the global nature of healthcare disruption during COVID-19, especially in regards to the postponement of non-urgent elective surgeries, presents particular challenges that healthcare systems might not be able to manage, leading to significant harm to patients downstream. We contend that to be truly ethical, the decision to postpone non-urgent elective surgeries should involve an established triage algorithm which can be implemented across the healthcare system and that can be scaled up or down in response to local variances in resource availability and disease burden. We encourage political leaders and health officials to strongly consider enacting policies that remove regulatory and commercial roadblocks to the more efficient sharing of resources between areas to address the ethical discrepancies we have discussed.
REFERENCES
- WHO. Coronavirus disease (COVID-19) situation report. 2020.
- Gold J. Some Hospitals Continue With Elective Surgeries Despite COVID-19 Crisis. Kaiser Health News, 2020.
- AMC. Joint Statement: Roadmap for Resuming Elective Surgery after COVID-19 Pandemic.2020.
- Kaye K, Paprottka F, Escudero R. Elective, Non-urgent Procedures and Aesthetic Surgery in the Wake of SARS-COVID-19: Considerations Regarding Safety, Feasibility and Impact on Clinical Management. Aesthetic Plast Surg. 2020; 44(3): 1014-1042.
- Kim SYH, Grady C. Ethics in the time of COVID: What remains the same and what is different. Neurology. 2020; 94(23):1007-1008.
- Arora A. Ethics in the age of COVID-19. Intern Emerg Med. 2020.
- Scheunemann LP, Whites DB. The ethics and reality of rationing in medicine. Chest. 2011; 140(6): 1625-1632
- Arabi Stahel PF. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. 2020;14:8.
- Murthy S, Webb S. COVID-19: A novel coronavirus and a novel challenge for critical care. Intensive Care Med 2020.
- Services CfMM. CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures during COVID-19 Response. CMS gov. 2020.
- Mouton, C., Hirschmann, M.T., Ollivier, M. COVID-19 ESSKA guidelines and recommendations for resuming elective surgery. J Exp Ortop. 2020.
- COVID Surg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br J Surg. 2020.
- Weissman GE, Crane-Droesch A, Chivers C. Locally informed simulation to predict hospital capacity needs during the COVID-19 pandemic. Ann Intern Med. 2020; M20-1260.
- Moghadas SM, Shoukat A, Fitzpatrick M. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc Natl Acad Sci. 2020; 117(16): 9122-9126.
- Hirschmann MT, Hart A, Henckel J, Sadoghi P, Seil R, Mouton C. COVID-19 coronavirus: Recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1690-1698.
- Carenzo L, Costantini E, Greco M. Hospital surge capacity in a tertiary emergency referral center during the COVID-19 outbreak in Italy. Anaesthesia. 2020; 75(7): 928-934.
- Stahel PF. How to risk-stratify elective surgery during the COVID-19 pandemic. Patient Saf Surg. 2020; 14:1-8.
- Ethics SU. What are the Basic Principles of Medical Ethics? 2020.
- Lin CJ, Nowalk MP, Pavlik VN. Using the 4 pillars practice transformation program to increase adult influenza vaccination and reduce missed opportunities in a randomized cluster trial. BMC Infect Dis. 2016; 16(1):623.
- Yu GY, Lou Z, Zhang W. Several suggestion of operation for colorectal cancer under the outbreak of Corona Virus Disease 19 in China. J Gastrointest Surg. 2020; 23(3):9-11.
- Kramer JB, Brown DE, Kopar PK. Ethics in the time of coronavirus: Recommendations in the COVID-19 Pandemic. J Am Coll Surg. 2020; 230(6):1114-1118.
- Chime. COVID-19 Hospital Impact Model for Epidemics. 2020.
- AMS. Local Resumption of Elective Surgery Guidance. 2020.
- Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. 2020; 323(11): 1061-9.
- Bundu I, Patel A, Mansaray A, Kamara TB, Hunt LM.Surgery in the time of Ebola: How events impacted on a single surgical institution in Sierra Leone. BMJ Open Access. 2016; 162(3): 212-216.
- Prem K, Liu Y, Russell TW. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modelling study. Lancet Public Health. 2020; 5(5): e261-e270.
- Emanuel EJ, Persad G, Upshur R. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N Engl J Med. 2020; 382(21): 2049-2055.
- Bannow T. UPMC defends decision to continue with some elective surgeries. 2020.
- Zhang S. What it really means to cancel elective surgeries. 2020.
- AMS. COVID-19: Guidance for triage of non-emergent surgical procedures. 2020.
- Zink A. COVID-19 Health Mandate. Governor Mike Dunleavy. 2020.
- Diaz A, Sarac BA, Schoenbrunner AR, Janis JE, Pawlik TM. Elective surgery in the time of COVID-19. Am J Surg. 2020;219(6): 900-902.
Citation: Brown N, Szabadi S, Quon C, Shlobin NA, Lien BV, Shahrestani S, et al. (2020) Ethical Considerations for the Cancellation of Non-Urgent Surgeries During the COVID-19 Pandemic and Suggestions for Future Health Crises. J Clin Res Bioeth. 11:365.
Copyright: © 2020 Brown NJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.