PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
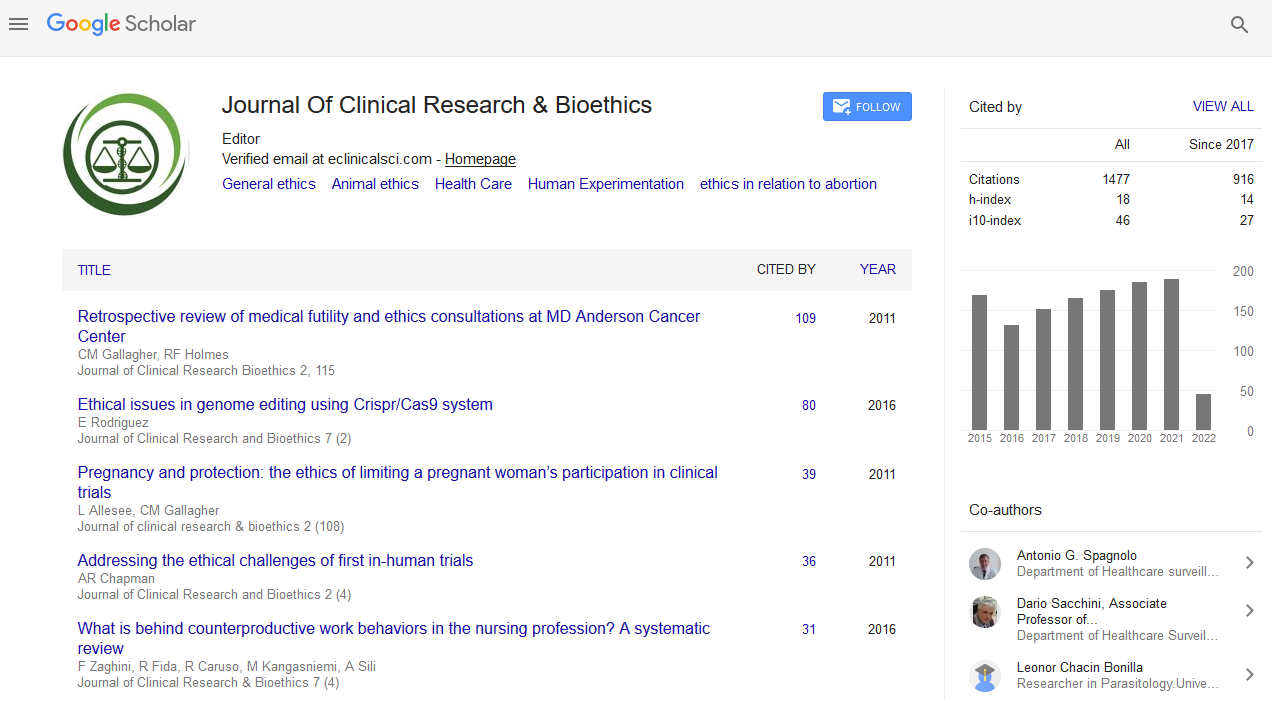
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2021) Volume 0, Issue 0
Equity and Utility in Allocating ICU Beds and Ventilators in COVID Pandemics
Jocelyne Saint-Arnaud1*, Mullins G2 and Ringuette L32Department of Health Law, Legal Counsel in Health Law and Health Management Consultant, School of Public Health, University of Montreal, Montrela, Quebec, Canada
3Department of Bioethics, School of Public Health, University of Montreal, Montrela, Quebec, Canada
Received: 13-Aug-2021 Published: 03-Sep-2021, DOI: 10.35248/2155-9627.21.s11.002
Description
The COVID-19 pandemics and the overload of hospitalization bring back the question of fair access to intensive care units and to ventilators. Doctors have long used criteria to prioritize access to treatments. The triage model used for emergencies gives priority to the sickest, those at risk of dying or those facing severe consequences, if delays in response are too long. It is the triage nurses who decide which cases will be given priority. This way of prioritizing was introduced on the battlefields by the surgeon-in-chief of Napoleon's armies, Jean Dominique de Larey, who applied the ideals of the French Revolution, by first treating the most affected, rather than those of higher rank [1,2]. This measure is fair if it meets the following two conditions: it applies the same rule to all; and it responds first to the most urgent needs [3-7]. The former condition applies impartiality and the latter specifies the content of the rule, which involves medical competence in assessing need. Non-medical criteria, for example, waiting lists, or social criteria such as age or social roles, may also be used for prioritization. These are not equitable if they do not meet health needs.
In the context of dialysis in the United States in the early 1960s, a triage protocol was used to determine who would have access to treatment, taking into account the fact that the Seattle Kidney Center had only six machines, although a large number of patients with severe kidney disease could have benefited. An initial triage was based on a medical assessment and a second triage was conducted by an independent committee that accorded priority on the basis of social criteria, such as marital status, number of dependents, education, employment, or place of residence [8]. This committee favored those most useful to society, the working man over the unemployed, the married man with one or more children over the single man, and Washington state residents over those from other American states.
To give access to critical care and ventilators, New York State (USA) and the province of Ontario (Canada) have developed their own triage protocols. In the New York State Ventilator Allocation Guidelines [9], those who would not survive intensive care treatment and ventilator use are first screened out based on medical criteria, and then the Sequential Organ Failure Assessment (SOFA) is used to assess mortality risk. This tool allows doctors to examine the status of six organs or systems, liver, kidneys, lungs, brain, blood pressure and coagulation, according to four levels of impairment. Each level is represented by a color, and it is the triage officer who grants or denies access to intensive care beds. Finally, a reassessment is made after 48 and 120 hours of intensive care, and those for whom treatment is ineffective at these points are discharged from the intensive care unit and will receive palliative care. Physicians assess the severity of impairments and effectiveness of treatments; decisions on access to or withdrawal from the ICU are made either by the triage officer or by a committee.
The Ontario Clinical Triage Protocol for Major Surge in COVID Pandemic has population-based goals of minimizing mortality and morbidity in the general population, as opposed to individual mortality and morbidity. It is, therefore, the principle of utility that dominates over an adequate response to individual needs. The protocol is applied in extreme situations of limited resources when the health system can no longer meet the demand; it occurs at three levels. At the first level, those with a probability of death ≥ 80% within one year are eliminated, followed by those with a 50% and 30% probability of death, depending on the pandemic outbreak curve and the extent of the resource gap. Elimination is done using 13 indicators that address health conditions such as severe trauma or burns, severe cognitive impairment, end stage organ failure, advanced neurocognitive disease, etc. Individuals who meet the exclusion criteria will not have access to intensive care, regardless of whether their problem is related to a critical condition. In case of a tie between candidates, randomization is used [10].
The second version of the Quebec National Prioritization Protocol, entitled Prioritization for Access to Critical Care (Adult) in the extreme pandemic context, is inspired by the Ontario Protocol and uses the same exclusion criteria with a few exceptions. However, in case of equal scores between candidates, using life cycle as a criterion, the youngest have priority, which is equivalent to using age as a social criterion; then priority is given to caregivers and finally, as a last resort, randomization is used, if necessary and according to the degree of overload of the health care system [11,12].
Conclusion
The two protocols are similar in that using a protocol provides more equal access to care than individual medical judgment. However, medical review and judgment are essential to triage patients who need and will survive intensive care. To this end, statistical references by type of impairment are factors to be considered. However, they do not replace the medical judgment that focuses on evaluating a specific individual’s health. The Ontario protocol relies more on the death statistics of individuals within one year, using exclusion criteria, whereas SOFA places greater emphasis on individual health based on inclusion criteria in a score that will ultimately eliminate individuals who are too ill to survive the disease and intensive treatments, including ventilator use. Both protocols have their limitations; the first is difficult to use in the high prioritization stages when those with a 30% chance of death within a year must be eliminated, and the second may not allow for the elimination of a sufficient number of people when resources become increasingly scarce. However, protocols that can best reconcile the response to individual needs and population goals to save more non co-morbid lives are more equitable.
REFERENCES
- Baker R, Strosberg M. Triage and Equality : An historical reassessment of utilitarian analyses of triage. Kennedy Inst Ethics J. 1992; 2(2): 103-123.
- Larrey DJ. Campaigns of Russia, Germany and France. 1982.
- Perelman Ch. Justice, in Justice and reason, Brussels: Editions of University of Brussels. 1972.
- Saint-Arnaud J. Ethical benchmarks for the health professions, Montreal: Liber. 2019:130.
- Daniels N. Is there a right to health care and, if so, what does it encompass. In: Beauchamp TL, Waters L (eds) Contemporary issues in bioethics. Thomson Wadsworth. 2003: p 46-52.
- Veatch RM. Justice the basic social contract and health care. In: Beauchamp TL, Waters L (eds) Contemporary Issues in Bioethics. Thompson Wadsworth. 2003; 53-58.
- Elster J, Herpin N. Ethics of medical choice. Dialogue La Librairie. 1992.
- Mc Cormick TR. Ethical issues in caring for patients with renal failure. ANNA J. 1993; 20 (5): 549-555.
- THC. New York State Task Force on Life and the Law Ventilator Allocation Guideline: How Our Views on Disability Evolved. 2015.
- Ontario Health. Clinical triage protocol for major surge in Covid Pandemic. 2020.
- Quebec Ministry of Health and Social Services. Prioritization for access to intensive care (adults) in the extreme context of a pandemic, General Directorate of University, Medical, Nursing and Pharmaceutical Affairs. 2020.
- Winsor S, Bensimon C, Sibald R, Anstey K, Chidwick P, Coughlin K, et al. Identifying prioritization criteria to supplement critical care triage protocols for the allocation of ventilators during a pandemic influenza, Healthc Q. 2014; 17(2): 44-51.
Citation: Saint-Arnaud J, Mullins G, Ringuette L (2021) Equity and Utility in Allocating ICU Beds and Ventilators in COVID Pandemics. J Clin Res Bioeth. S11:002.
Copyright: © 2021 Saint-Arnaud J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.