PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
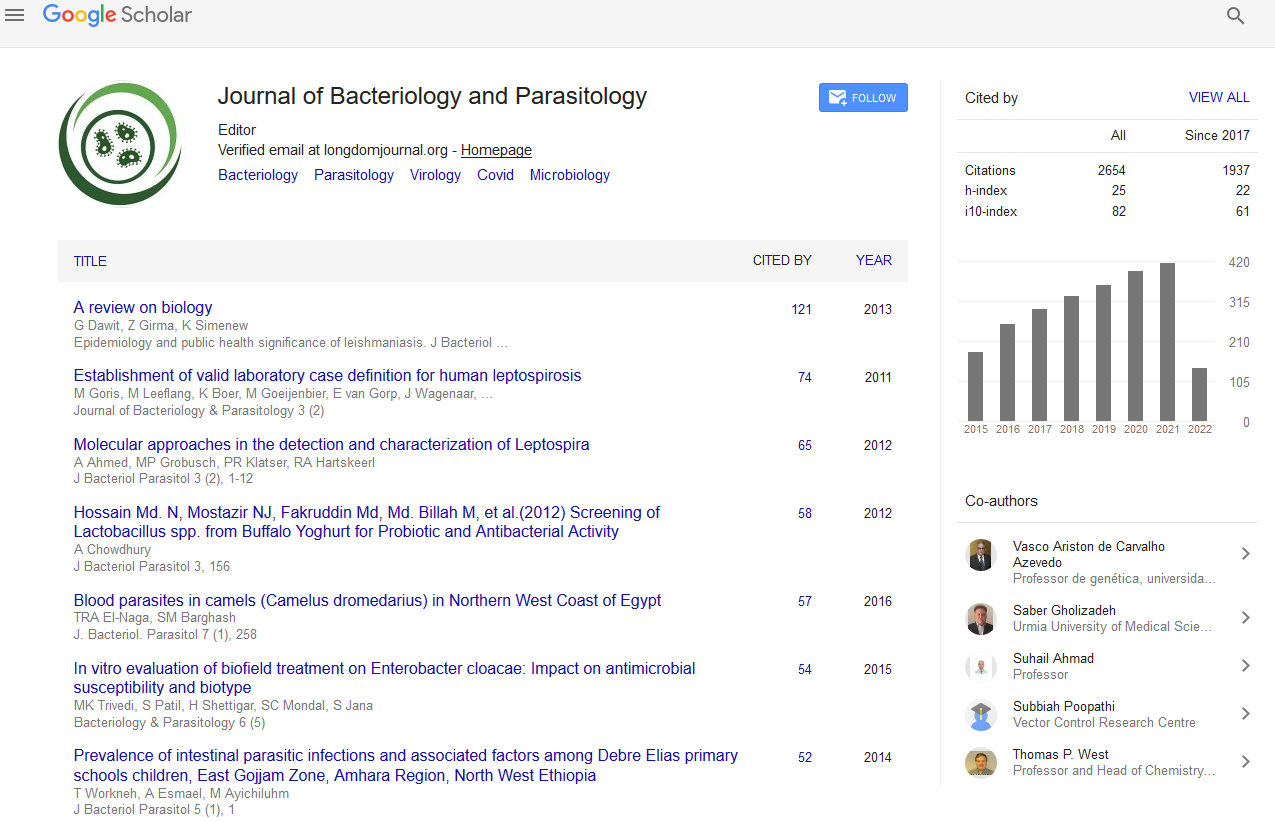
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2019) Volume 10, Issue 5
Mycoplasma genitalium in Senegalese Patients Attending a Private Laboratory in Dakar
Diop-Ndiaye H1*, Jaber R2, Macondo E2, Diagne R3, Ndiaye AJS2, Diakhaby EB4, Sow-Ndoye A1, Camara M1, Ba-Diallo A1, Dieng A1, Siby T2, Boye CSB1 and Toure-Kane C22Biologist Pharmacist, Laboratory BIO 24, Dakar, Senegal
3Department of Health Sciences, University of Thies, Thies, Senegal
4Department of Bacteriology and Virology, CHNU Dalal Jam, Dakar, Senegal
Received: 18-Oct-2019 Published: 11-Nov-2019
Abstract
Introduction: The contribution of M. genitalium in genital infections in Senegal is poorly understood due to a limited access to molecular biology platforms. The aim of this study is to document the place of M. genitalium infection in men and women attending a private laboratory and to document its association with other STI pathogens.
Materials and methods: M. genitalium detection was performed in genital secretions using RealLine Chlamydia trachomatis/ Mycoplasma genitalium (Biosynex, France) at BIO24 biomedical laboratory in Dakar (Senegal). In parallel, other genital pathogens including N. gonorrhoeae and common Mycoplasma species were detected through culture and microscopic analysis.
Results: From March 2016 to November 2017, genital secretions from 3550 patients were analyzed. The mean age was 32 years (range: 16 to 71) with a sex-ratio of 0.13. Overall, M. genitalium, C. trachomatis, N. gonorrhoeae and U. urealyticum were detected at a frequency of 1.7%, 2.82%, 0.5% and 11.86%, respectively. In women, C. albicans, bacterial vaginosis, T. vaginalis and M. hominis were found at a frequency of 19.6%, at 22%, 0.8% and 0.9%, respectively. M. genitalium infection was significantly more prevalent in men than women and more frequently associated with C. trachomatis than N. gonorrhoeae. One third of M. genitalium infected women presented also bacterial vaginosis signs and a high pH value (>4.5) of genital secretions was observed in all infected women.
Conclusion: M. genitalium appeared as a second most common STI pathogen identified in patients attending a private laboratory, indicating the need to include its routine detection for STI suffering patients also in public health sector.
Keywords
M. genitalium; Genital infections; Private laboratory; Senegal
Introduction
Mycoplasma genitalium is a sexually transmitted pathogen that has been poorly understood because of a slow and fastidious culture. Highlighted in the early 1990s with the advent of molecular biology [1], it is now well established that it is an emerging, cosmopolitan pathogen responsible for genital infections affecting both man and woman. For instance, M. genitalium is the common cause of nongonococcal urethritis (UNG) in men after Chlamydia trachomatis [2-5]. In women, a significant association has been described in low genital tract infections such as cervicitis and urethritis and M. genitalium is to date the only mycoplasma responsible for cervicitis [6-9].
M. genitalium is also responsible for upper genital tract infections like salpingitis or endometritis and certain studies showed M. genitalium implicated in severe complications such as ectopic pregnancies and tubal sterility [3,6,10]. It would also be responsible for prematurity [11].
However, this routine etiologic diagnosis is very little carried out in resource-limited countries such as Senegal due to the weakness of technical platforms and the need of molecular technics for M. genitalium diagnosis. In Senegal, only few private laboratories perform the detection of M. genitalium from clinical specimens and only few epidemiological data are currently available regarding the prevalence of this agent, which would be more prevalent in resource-limited countries [12].
The aim of this study is to document the place of M. genitalium infection in men and women attending a private laboratory for genital infection diagnosis and, to document its association with other STI pathogens.
Materials and Methods
Study design
From March 2016 to November 2017, testing for M. genitalium was carried out on a cross sectional study in genital secretions for both men and women at BIO24 biomedical private laboratory in Dakar (Senegal) for each request of C. trachomatis detection.
Molecular testing
These 2 pathogens were identified using a multiplex real time PCR (Amplix Biosynex, France) from cervical swabs collected in women genital tract and from men urine samples. DNA extraction was performed using the Nucleic acid extractor platform ExiPrepTM16DX and real time PCR by using the RealLine Chlamydia trachomatis/Mycoplasma genitalium (Biosynex, France) on Amplix platform according to manufacturer instructions.
Culture and microscopic analysis
In parallel, other pathogens were detected through culture or microscopic analysis. N. gonorrhoeae diagnosis was performed by culture on a Thayer-Martin modified media with antibiotics (Biomerieux, France) and incubation is carried out under a CO2 atmosphere at 37°C for 24-48 hours. Candida detection used vaginal swabs seeded on chromogenic yeast agar and incubates at 30°C for 24-48 hours for. Diagnosis of Mycoplasma hominis and Ureaplasma urealyticum infection was performed using both liquid Mycoplasma IST2 media (Biomerieux, France) and Mycoplasma A7 media (Biomerieux, France). Trichomoniasis was diagnosed by detection of motile trichomonads on wet mount microscopy and disruption of the vaginal microbiota was characterized by Nugent score (0-3=normal microbiota (reference group), 4-6=intermediate microbiota disruption, and 7-10=Bacterial vaginosis).
Data analysis
Data were recorded in an excel file used as a support for results analysis. The infection rates were expressed as percentages (%) with their 95% confidence intervals. Statistical analysis included comparison of the frequencies were carried out by Chi-square test and a "p value" less than 0.05 was considered significant.
Results
Patients
From March 2016 to November 2017, 3550 analysis requests for C. trachomatis and/or M. genitalium addressed to BIO24 and were performed accordingly to manufacturer instructions. Patients were aged from 16 to 71 years (mean=32 years old) and the sex-ratio was 0.13 (428 Men versus 3122 women).
STI and other genital pathogens detected
The STI and other genital pathogens detected in the studied population were presented in Table 1. Overall, M. genitalium and C. trachomatis were detected in 60 cases (1.7% (95% CI=[1.3-2.1]) and 100 cases (2.82% (95% CI=[2.3-3.4]), respectively. N. gonorrhoeae infection was detected in 19 patients giving a proportion of 0.5% (95% CI=[0.3-0.7]). In women in particular, fungal infections with C. albicans were found at a frequency of 19.6%, bacterial vaginosis at 22% and T. vaginalis at 0.8%. U. urealyticum infection was present in 4.2% of cases in men and 12.9% of cases in women. M. hominis was found in 0.9% of the study population, exclusively in women.
| Total n (%) N=3550 | 95% CI | |
|---|---|---|
| C. trachomatis | 100 (2.82%) | 2.3-3.4 |
| M. genitalium | 60 (1.69%) | 1.3-2.1 |
| N. gonorrhoeae | 19 (0.53) | 0.3-0.8 |
| T. vaginalis | 30 (0.84) | 0.5-1.1 |
| C. albicans | 613(19.63%)* | 18.3-21 |
| G. vaginalis ± Mobilincus | 688 (22%)* | 20.5-23.5 |
| U. urealyticum | 421 (11.86%) | 10.8-12.9 |
| M. hominis | 35 (0.98%)* | 0.7-1.3 |
Table 1: Sexual transmitted pathogen and other agents detected in the genital tract.
Factors associated to M. genitalium infection
According to sex distribution, as shown in Table 2, M. genitalium infection were significantly more prevalent in male than women as well as other STI pathogens except U. urealyticum which was significantly more frequent in women. Moreover, M. genitalium infection in women appears to be significantly less common than C. trachomatis infection; furthermore these 2 pathogens were significantly more frequent than N. gonorrhoeae infection in both men and women (Table 2).
| Men n (%) | Women n (%) | p value | |
|---|---|---|---|
| N=428 | N=3122 | ||
| C. trachomatis | 37 (8.64%) | 63 (2.01%) | <0.01 |
| M. genitalium | 30 (7%) | 30 (0.96%) | <0.01 |
| N. gonorrhoeae | 14 (3.27%) | 5 (0.16%) | <0.01 |
| U. urealyticum | 18 (4.2%) | 403 (12.9%) | <0.01 |
Table 2: Pathogens detected according to sex.
Table 3 highlights M. genitalium association with other pathogens. Regarding dual infection by both M. genitalium and C. trachomatis, 2.8% (12/428) of men were concerned whereas only 0.5% (16/3122) of women. Comparatively, the proportion of dual infection by both M genitalium and N. gonorrheae was very low with 0.7% (3/428) and 0.03% (1/3122) in men and women, respectively.
| Men Mg pos | Women Mg pos | ||||
|---|---|---|---|---|---|
| % (n/N) | OR [95% CI] ; p value | % (n/N) | OR [95% CI]; p value | p value (men vs. women) | |
| C. trachomatis | 2.8% (12/428) | 9.9 [4.3-22]; <0.01* | 0.5% (16/3122) | 74 [34.1-160]; <0.01* | <0.01* |
| N. gonorrhoeae | 0.7% (3/428) | 3.9 [1-14]; 0.04* | 0.03% (1/3122) | 26.6 [2-245]; <0.01* | <0.01* |
| C. albicans | na | 0.16% (5/3122) | 0.8 [0.3-2.1]; 0.6 | ||
| G. vaginalis +/- Mobilincus | na | 0,3% (10/3122) | 1.8 [0.8-3.8]; 0.13 | ||
| U. urealyticum | 0,2% (1/428) | 0.7 [0.09-2]; 0.06 | 0.5% (7/3122) | 2 [0.8-4.8]; 0.08 | 0.39 |
| *p-value<0.05 | |||||
Table 3: Association of M. genitalium with other STI and genital pathogens.
Therefore, M. genitalium appeared to be significantly more frequently associated with C. trachomatis than N. gonorrhoeae (p<0.01). However, the risk of being co-infected is highest for women for both C. trachomatis (OR=74; p<0.01 vs. OR=9.9; p<0.01) and N. gonorrhoeae (OR=26.6; p<0.01 vs. OR=3.9; p<0.04). Moreover, one third of M. genitalium infected women was also infected with bacterial vaginosis pathogens and a high pH value (>4.5) of genital secretions was observed in all infected women even in absence of bacterial vaginosis; two-third (66.7%) had abundant leucorrhea and 66.7% presented also inflammation with leucocytes>5 cells per field. Regarding symptoms in women, abundant leucorrhoea was the most common symptom for both pathogens while Pelvic pain was more common in M. genitalium-infected women (14.3%) than in C. trachomatis-infected women (2.1%) (Figure 1).

Figure 1. Distribution of symptoms/reason of consultation reported in men infected with M. genitalium and/or and C. trachomatis.
Urethritis and micturition burns were the most common symptoms in men for both M. genitalium and C. trachomatis infection whereas infertility was noted in 5.4% of men infected with C. trachomatis. One case of prostatitis and one case of epididymitis were reported for patients infected by M. genitalium (Figure 2).

Figure 2. Distribution of symptoms/reason of consultation reported in women infected with M. genitalium and/or C. trachomatis.
Discussion
M. genitalium is an emerging STI pathogen; its role in genital infections has been ignored in most developing countries and still probably underestimated, due to a suboptimal diagnosis related to a lack of knowledge of the pathogen and lack of molecular biology platforms on health facilities and clinical laboratories. In Senegal, M. genitalium diagnosis is not realized in routine laboratory testing and only few private structures like BIO24 performed its detection using molecular tools. To our knowledge this is the first description of M. genitalium infection in the country. On a period of 19 months, a Mutiplex PCR was performed for the detection of both M. genitalium and C. trachomatis from a large number of cervical swabs and men’s urine specimens.
With a prevalence of 1.69%, M genitalium appeared to be the 2nd most common STI pathogen detected after C. trachomatis as in different studies [13-15]. This prevalence was lowest than those reported in many developing countries where M genitalium was found at rates ranging from 3.2% to 5.2% [12]. This low prevalence includes patients without symptoms (one third of men and about 40% of women detected positive for M. genitalium) and demonstrates that this pathogen could be identified in asymptomatic persons in a non-negligible proportion [16]. This prevalence was more related to those reported in high-income countries (HIC) like in study realized among 5628 patients consulting for STI [14], or among 1652 patients from general population [17], (or among adults (16-44 years) during the third national survey [18] with 1.9% in Netherland, 1.7% in Denmark and 1.2% in England, respectively.
However, in a multicenter study realized in France including 2652 urogenital tract specimens collected all around the country, the picture was different with 3.4% [16]. In fact, it is well established that M genitalium prevalence could varied among different risk groups; the highest rates were found in STI treatment centers [16,19], key populations such as Men having sex with men (MSM) or female sex workers [20-22], or HIV infected patients [23-25]. According to gender, M genitalium was found significantly more prevalent in men than women (7% vs. 0.96%; p<0.01). This is in line with other studies in general population or community based in other africans countries but the prevalence found in women was slightly lower than those reported with 3.2% in Tanzania [26], 2.7% at Madagascar [12], as well as in a recent study in adult women in Chad [27].
In the other hand, men appear very vulnerable to M genitalium with prevalence (7%) similar to what was found in MSM [12] or in a specific population of men with urethral discharge [2,28]. This difference could be explained by the relatively small number of samples analyzed comparing to women, the bias linked to the frequentation of clinics by men only when they have symptoms, and finally related to the specificity of M. genitalium for urethritis in men. Clinical symptoms for M. genitalium positive patients were similar to those noted by Pereyre et al. in France with urethral discharge and vaginal discharge accounted for the majority of the signs observed. However, in this French study, unlike our study, a high percentage (70%) of M. genitalium positive patients were found with no associated symptoms [16].
Regarding the other factors associated with M. genitalium infection in women, it appears that vaginal pH was greater than 4.5 (ranging from 4.6 to 6.7) in all M. genitalium infected women which corroborate Huppert et al. results who demonstrated that pH>4.5 was a predictive sign of M. genitalium infection (odds ratio 4.4, p<0.05). He showed that among women without bacterial vaginosis, and not infected with TV, 25% of those with a vaginal pH>4.5 were infected with M. genitalium, compared to 9% for those with a pH ≤ 4.5 (p=0.02) [29].
Regarding the microscopic signs of the inflammatory reaction (number of leukocytes/ microscopic field), 66.7% of women positive for M. genitalium had an important inflammation with more than 4.5 leucocytes/microscopic field. These results agreed with Anagrius et al. study, which show a strong association between M. genitalium infection and microscopic signs of urethritis and/ or cervicitis [30]. M. genitalium appears to be also associated to bacterial vaginosis that could enhance patient susceptibility to infection as described par Lokken [31].
Conclusion
This pioneering study focusing on M. genitalium detection in both men and women in a private laboratory in Senegal, showed a prevalence that place it as a second most common STI pathogen identified in both symptomatic and asymptomatic patients.
In women, M genitalium infection was often associated to bacterial vaginosis and could be suspected in case of large inflammation reaction associated to pH value greater than 5 whereas the proportions in men highlighted the need of its detection especially in men suffered for urethritis. These results showed also the risk of co-infection with others STI pathogen that could impact at long term fertility and should be considered for a better uptake of cases. Further studies in public health sector as well as advocacy for clinician’s awareness in order to increase demand of MG testing and for decision-makers to better consider this agent in STI programs are needed.
REFERENCES
- Palmer HM, Gilroy CB, Furr PM, Taylor-Robinson D. Development and evaluation of the polymerase chain reaction to detect Mycoplasma genitalium. FEMS Microbiol Lett. 1991; 61(2):199-203.
- Pépin J, Sobéla F, Deslandes S, Alary M, Wegner K, Khonde N, et al. Etiology of urethral discharge in West Africa: The role of Mycoplasma genitalium and Trichomonas vaginalis. Bull World Health Organ. 2001; 79(2): 118-126.
- Cazanave C, Manhart LE, Bébéar C. Mycoplasma genitalium, an emerging sexually transmitted pathogen. Med Mal Infect. 2012;42(9):381-392.
- Plantamura J, Bigaillon C, Bousquet A, Delaune D, Larreche S, Bugier S, et al. Mycoplasma genitalium: A mycoplasma still underestimated. Ann Biol Clin. 2017;75(2):209-214.
- Libois A, Hallin M, Crucitti T, Delforge M, De Wit S. Prevalence of Mycoplasma genitalium in men with urethritis in a large public hospital in Brussels, Belgium: An observational, cross-sectional study. PLoS One. 2018;13(4):1-6.
- Manhart LE, Critchlow CW, Holmes KK, Dutro SM, Eschenbach DA, Stevens CE, et al. Mucopurulent cervicitis and Mycoplasma genitalium. J Infect Dis. 2003; 187(4): 650-657.
- Pepin J, Labbe AC, Khonde N, Deslandes S, Alary M, Dzokoto A, et al. Mycoplasma genitalium: An organism commonly associated with cervicitis among west African sex workers. Sex Transm Infect. 2005;81(1):67–72.
- Moi H, Reinton N, Moghaddam A. Mycoplasma genitalium in women with lower genital tract inflammation. Sex Transm Infect. 2009;85(1):10-14.
- Oakeshott P, Aghaizu A, Hay P, Reid F, Kerry S, Atherton H, et al. Is Mycoplasma genitalium in women the "New Chlamydia"? A community-based prospective cohort study. Clin Infect Dis. 2010;51(10):1160-1166.
- Tsevat DG, Wiesenfeld HC, Parks C, Peipert JF. Sexually transmitted diseases and infertility. Am J Obstet Gynecol. 2017;216(1):1-9.
- Hitti J, Garcia P, Totten P, Paul K, Astete S, Holmes KK. Correlates of cervical Mycoplasma genitalium and risk of preterm birth among Peruvian women. Sex Transm Dis. 2010; 37(2): 81-85.
- Baumann L, Cina M, Egli-Gany D, Goutaki M, Halbeisen FS, Lohrer GR, et al. Prevalence of Mycoplasma genitalium in different population groups: Systematic review and meta-analysis. Sex Transm Infect. 2018; 94(4): 255-262.
- Svenstrup HF, Dave SS, Carder C, Grant P, Morris-Jones S, Kidd M, et al. A cross-sectional study of Mycoplasma genitalium infection and correlates in women undergoing population-based screening or clinic-based testing for Chlamydia infection in London. BMJ Open. 2014;4(2):1-8.
- Jenniskens ML, Veerbeek JH, Deurloo KL, van Hannen EJ, Thijsen SF. Routine testing of Mycoplasma genitalium and Trichomonas vaginalis. Infect Dis. 2017;49(6):461-465.
- Ferré VM, Ekouevi DK, Gbeasor-Komlanvi FA, Collin G, Le Hingrat Q, Tchounga B, et al. Prevalence of human papillomavirus, human immunodeficiency virus and other sexually transmitted infections among female sex workers in Togo: a national cross-sectional survey. Clin Microbiol Infect. 2019;25(12):1-5.
- Pereyre S, Nadalié CL, Bébéar C, investigator group, Mycoplasma genitalium and Trichomonas vaginalis in France: A point prevalence study in people screened for sexually transmitted diseases. Clin Microbiol Infect. 2017;23(2):3-6.
- Andersen B, Sokolowski I, Østergaard L, Møller JK, Olesen F, Jensen JS. Mycoplasma genitalium: Prevalence and behavioural risk factors in the general population. Sex Transm Infect. 2007;83(3):237–241.
- Sonnenberg P, Ison CA, Clifton S, Field N, Tanton C, Soldan K, et al. Epidemiology of Mycoplasma genitalium in British men and women aged 16–44 years: Evidence from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Int J Epidemiol. 2015;44(6):1982–1994.
- Mobley VL, Hobbs MM, Lau K, Weinbaum BS, Getman DK, Seña AC. Mycoplasma genitalium infection in women attending a sexually transmitted infection clinic: Diagnostic specimen type, coinfections, and predictors. Sex Transm Dis. 2012;39(9):706-709.
- Edlund M, Blaxhult A, Bratt G. The spread of Mycoplasma genitalium among men who have sex with men. Int J STD and AIDS. 2012;23(6):455-456.
- Vandepitte J, Muller E, Bukenya J, Nakubulwa S, Kyakuwa N, Buvé A, et al. Prevalence and correlates of Mycoplasma genitalium infection among female sex workers in Kampala, Uganda. J Infect Dis. 2012;205(2):289-296.
- Deborde M, Pereyre S, Puges M, Bébéar C, Desclaux A, Hessamfar M, et al. High prevalence of Mycoplasma genitalium infection and macrolide resistance in patients enrolled in HIV pre-exposure prophylaxis program. Med Mal Infect. 2019;49(5):347-349.
- Leutscher P, Jensen JS, Hoffmann S, Berthelsen L, Ramarakoto CE, Ramaniraka V, et al. Sexually transmitted infections in rural Madagascar at an early stage of the HIV epidemic: A 6-month community-based follow-up study. Sex Transm Dis. 2005;32(3):150-155.
- Gatski M, Martin DH, Theall K, Amedee A, Clark RA, Dumestre J, et al. Mycoplasma genitalium infection among HIV-positive women: Prevalence, risk factors and association with vaginal shedding. Int J STD and AIDS. 2011;22(3):155-159.
- Cazanave C, Lawson-Ayayi S, Hessamfar M, Neau D, Dupon M, Morlat P, et al. Prevalence of Mycoplasma genitalium among HIV-infected women, Agence Nationale de Recherches sur le SIDA et les hépatites virales CO3 Aquitaine Cohort, France. Sex Transm Dis. 2013;40(8):653-654.
- Kapiga SH, Sam NE, Mlay J, Aboud S, Ballard RC, Shao JF, et al. The epidemiology of HIV-1 infection in northern tanzania: results from a community-based study. AIDS Care. 2006;18(4):379–387.
- Nodjikouambaye ZA, Compain F, Sadjoli D, Mboumba Bouassa RS, Péré H, Veyer D, et al. Accuracy of Curable Sexually Transmitted Infections and Genital Mycoplasmas Screening by Multiplex Real-Time PCR Using a Self-Collected Veil among Adult Women in Sub-Saharan Africa. Infect Dis Obstet Gynecol. 2019;2019(1):12-15.
- Ekiel A, Aptekorz M, Kłuciński P, Smolec D, Wiechuła B, Jóźwiak J, et al. Prevalence of Urogenital Mycoplasmas Among Men with NGU in Upper Silesia, Poland. Preliminary Study. Pol J Microbiol. 2016;65(1):93-95.
- Huppert JS, Bates JR, Weber AF, Quinn N, Gaydos CA. Abnormal vaginal pH and Mycoplasma genitalium infection. J Pediatr Adolesc Gynecol. 2013;26(1):36-39.
- Anagrius C, Loré B, Jensen JS. Mycoplasma genitalium: Prevalence, clinical significance, and transmission. Sex Transm Infect. 2005;81(6):458-462.
- Lokken EM, Balkus JE, Kiarie J, Hughes JP, Jaoko W, Totten PA, et al. Association of Recent Bacterial Vaginosis With Acquisition of Mycoplasma genitalium. Am J Epidemiol. 2017;186(2):194-201.
Citation: Diop-Ndiaye H, Jaber R, Macondo E, Diagne R, Ndiaye AJS, Diakhaby EB, et al. (2019) Mycoplasma genitalium in Senegalese Patients Attending A Private Laboratory in Dakar. J Bacteriol Parasitol. 10:363. DOI: 10.35248/2155-9597.19.10.363.
Copyright: © 2019 Diop-Ndiaye H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.