Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Geneva Foundation for Medical Education and Research
- Euro Pub
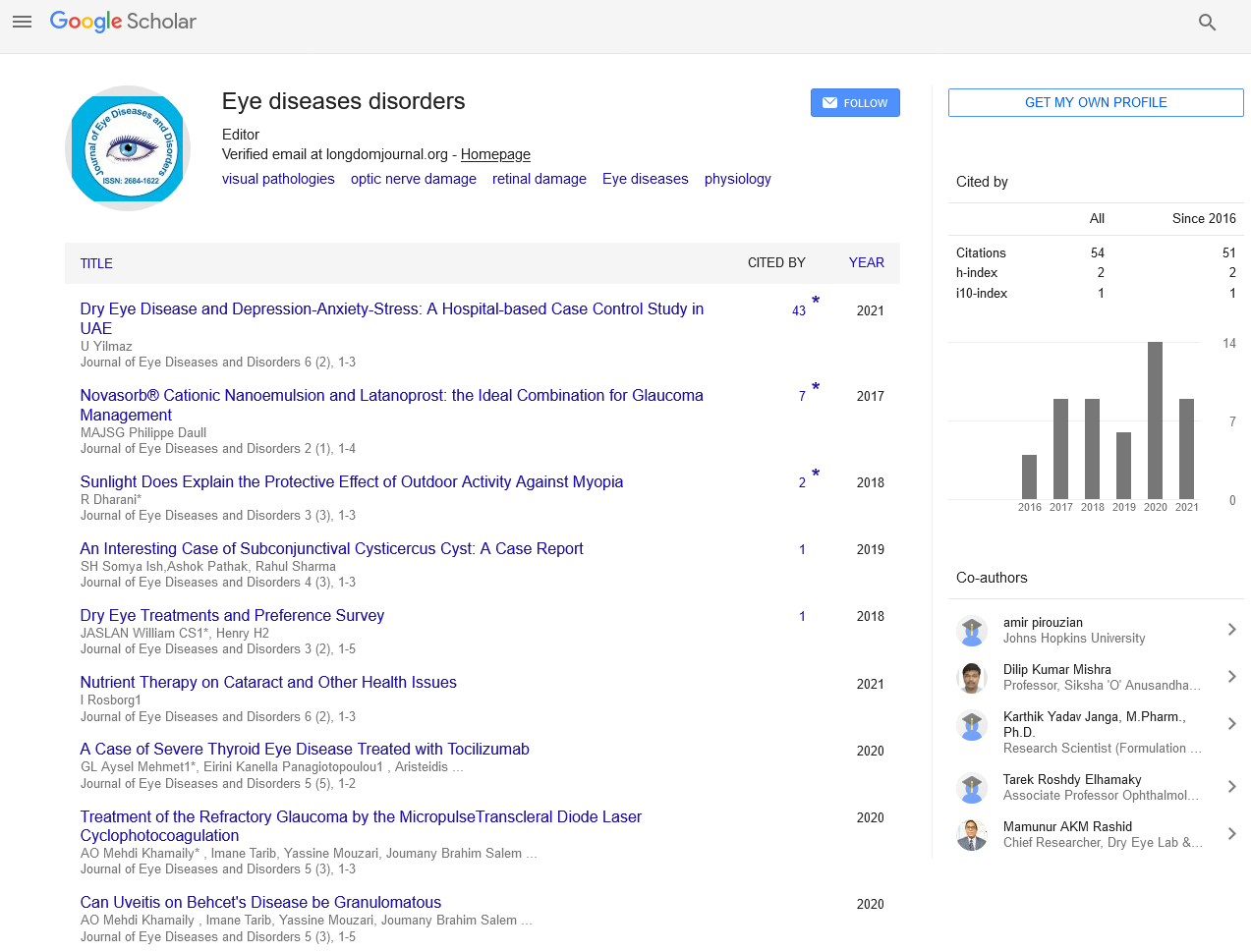
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2018) Volume 3, Issue 2
Dry Eye Treatments and Preference Survey
William CS1*, Henry H2, Jeanette AS1 and Lindsay AN12Allysta Pharmaceuticals, Inc., Hillsborough, USA
Received: 25-Apr-2018 Published: 19-May-2018, DOI: 10.35248/2684-1622.18.3.118
Abstract
Purpose: To survey ophthalmologists regarding their current therapy preferences and desires for future treatment to help guide providers in choosing treatments and pharmaceutical startups in developing future therapies.
Methods: A prospective survey developed internally and sent twice to ophthalmologists.
Results: There were 76 responses. Approximately 30% of respondents stated they examined a few cases of DED patients a day and 20% noted DED was a majority of their practice. Almost all physicians recommended tear replacement drops (95%) for their patients while 80% prescribed cyclosporine. Importantly, 40% started prescribing lifitegrast and the same percent prescribe tetracycline. When asked what new mechanisms of action physicians preferred, about 70% indicated improved tear film stability, while 50% desired greater lacrimal gland tear production. Further, 70% of physicians noted they would prescribe a product that increased tear film stability as first line. With two anti-inflammatory DED products currently available 55% of participants noted a third product should have a different mechanism of action while 25% desired better anti-inflammatory activity. In evaluating the available DED medications specifically, participants believed cyclosporine and lifitegrast had similar moderate levels of efficacy; with lifitegrast being slightly better tolerated than cyclosporine.
Conclusions: The survey showed that DED patients are an important part of the ophthalmic practice. Multiple different therapeutic techniques are used and there is desire for new products that especially would treat tear film stability and corneal surface disease.
Keywords
Dry eye disease; Startups; Development; Therapies; Treatments
Introduction
Dry eye disease (DED) continues to be an important part of ophthalmic related pathology as well as a target for new treatment products. DED afflicts a significant part of the adult population (6%-34%) [1-4]. Symptoms can be irritating, causing reduced quality of life, visual disturbance and pain [5].
Treatment modalities are multiple with no precise standard of care although helpful guidelines are available [5]. Two anti-inflammatory topical medications, cyclosporine (Restasis™) and lifitegrast (Xiidra™), as well as tear replacement drops are effective and commonly used. However, none of the available treatments are completely curative or prevent symptoms. Accordingly, at least 77 DED related products have been under development over the last number of years that have publicly available information including 12 active compounds with new mechanisms of action that is not currently available as well as a variety of tear replacement formulations and delivery systems [6]. Despite so many DED patients in the population, and diverse treatments available, little information exists on physician attitudes in treating DED both in terms of current practices and future treatment.
The purpose of this study was to survey ophthalmologists regarding their current therapy preferences and desires for future treatment. It is hoped this information would help guide providers in choosing current treatments and pharmaceutical startups in developing future therapies.
Methods
The design was a prospective survey of ophthalmologists. We used an existing internal, proprietary diverse database of ophthalmic physicians (n=1837). The survey was sent to each physician in the database. Invitations were sent October 25, 2016 and reminders were sent November 10, 2016. Survey questions were developed internally, and the survey was linked through Survey Monkey (www.surveymonkey.com). A copy of the survey questions can be found online (supplemental).
Results
Of 1837 surveys sent, 76 (4.2%) responded. Please see the full survey online (supplemental material). Approximately 70% of the respondents had been in practice for 20 or more years. About 50% were in a private group practice and 24% at a university. The most common subspecialty was glaucoma at 40% while 25% indicated they were anterior segment. Of the total, around 40% practiced comprehensive ophthalmology.
Approximately 30% of respondents stated they examined a few cases of DED patients a day while 25% indicated it was an important minority of their practice. However, 20% noted DED was a majority of their practice.
Almost all physicians recommended tear replacement drops (95%) for their patients while almost 80% prescribed cyclosporine. Three quarters of physicians use punctal occlusion and separately corticosteroids while 55% prescribe eyelid therapy. Importantly, 40% have started prescribing lifitegrast and the same percent prescribe tetracycline. Other treatment methods are less commonly used (Table 1).
| Responses | Percentage |
|---|---|
| Tear replacement drops | 96% |
| Cyclosporine | 78% |
| Punctal occlusion | 66% |
| Corticosteroids/other anti-inflammatory agents | 64% |
| Eyelid therapy | 55% |
| Lifitegrast | 41% |
| Tetracycline | 38% |
| Serum | 28% |
| Contact lenses | 12% |
| Surgery | 12% |
| Systemic immunosuppressant | 7% |
| Pilocarpine | 5% |
| Other | 3% |
Table 1: Treatment options considered for DED patients (respondents could choose all that apply)
When asked what new mechanisms of action participants preferred, about 70% indicated improved tear film stability, while 50% desired greater lacrimal gland tear production. Also, about 40% each wanted augmented anti-cytokine activity, overall better anti-inflammatory activity and improved epithelial surface healing (Table 2).
| Responses | Percentage |
|---|---|
| Improved tear film stability | 72% |
| Enhanced tear production | 53% |
| Anything that helps! | 42% |
| Better anti-inflammatory CD4+T cell inhibition (i.e., better than cyclosporine, lifitegrast) | 42% |
| Anti-inflammatory cytokine inhibition | 39% |
| Epithelial healing/protection | 39% |
| Greater mucin preservation | 34% |
| Antioxidant activity | 11% |
| Unsure | 4% |
Table 2: If more medicines become available what actions would you like to see? (respondents could choose up to 3 they consider most important)
Further, 70% of physicians noted they would prescribe first line a product that increased tear film stability. In addition, for a medicine that improved epithelial healing, or augmented tear film production, they would prescribe first line such a medicine 50% and 45% of the time respectively.
With two anti-inflammatory DED products currently available 55% of participants noted a third product should have a different mechanism of action while 25% desired better anti-inflammatory activity.
In evaluating the two currently available DED medications specifically, participants believed cyclosporine and lifitegrast had similar moderate levels of efficacy. However, physicians thought lifitegrast was slightly better tolerated than cyclosporine. Regarding the new product lifitegrast, 40% of physicians stated they either already prescribed it or planned to prescribe.
Discussion
The survey showed that DED patients are generally an important part of the practice of responding physicians. They indicated they used multiple different therapeutic techniques especially including: tear replacement drops, anti-inflammatory medications, punctual occlusion and eyelid therapy.
Despite these available treatments, these ophthalmologists desired new medicines that especially would be a different mechanism of action or have greater anti-inflammatory effect than the two medicines currently available, which are viewed as modest to moderately effective.
Preferred new mechanisms of action were greater tear film stability, improved corneal surface healing and an enhanced anti-inflammatory effect. A product with such actions would be prescribed by respondents as first line therapy approximately 50% of the time or more. These study results help confirm the usage and perceived desirability of current modalities for treating dry eye. However, the survey also emphasizes the need for new treatments that would perhaps help bring resolution to the disease or at least further reduce signs and symptoms without ocular surface irritation. We are fortunate that a number of new companies are working to bring new products with novel mechanisms to further assist patients in the future.
This survey was limited by the slightly low response rate, with respondents generally having mature practices that commonly saw patients with DED, and there was a high percent of academically based physicians. Possibly a younger group of ophthalmologists in a variety of practice settings would have indicated a different treatment perspective. In addition, the new medication lifitegrast has been on the market a short period and impressions for this product might change over time.
This study provides insight to ophthalmologists’ treatment patterns in DED and preferences for future therapy. Respondents currently utilize a wide menu of techniques to treat DED. However, they desire new products that especially would treat tear film stability and corneal surface disease.
REFERENCES
- McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR (1998) The epidemiology of dry eye in Melbourne. Ophthalmology 105: 1114-1119.
- Lin PY, Tsai SY, Cheng CY, Liu J-H, Chou P, et al. (2003) Prevalence of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology 110: 1096-1101.
- Paulsen AJ, Cruickshanks KJ, Fischer ME, Huang GH, Klein BE, et al. (2014) Dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol 157: 799-806.
- Schaumberg DA, Sullivan DA, Buring JE, Dana MR (2003) Prevalence of dry eye syndrome among US women. Am J Ophthalmol 136: 318-326.
- (2007)The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop. Ocul Surf 5: 93-107.
- Sharpe RA, Austin JP, Kruft B, Nelson LA, Stewart JA, et al. (2015) Description of ophthalmic pharmaceutical and device start-up companies. Ophthalmic Res 54: 6-9.
Citation: William CS, Henry H, Jeanette AS, Lindsay AN (2018) Dry Eye Treatments and Preference Survey. J Eye Dis Disord 3:118. doi : 10.35248/2684-1622.18.3.118
Copyright: © 2018 William CS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.