Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Euro Pub
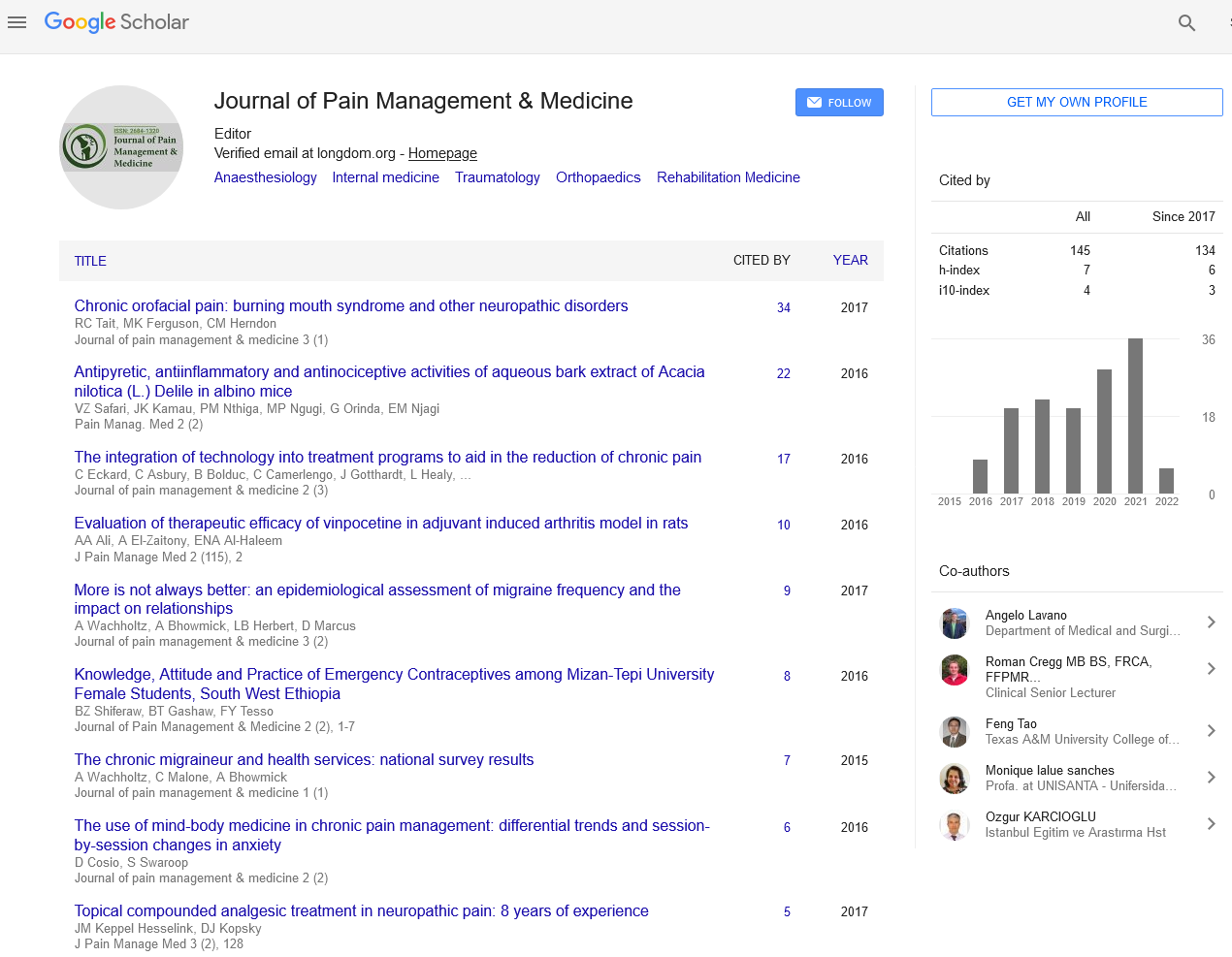
- Google Scholar
- Quality Open Access Market
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Mini Review - (2021) Volume 7, Issue 3
Discussion of Targeted Drug Delivery Article
David Schultz1*, Jonathan M. Hagedorn2, Scott Stayner3 and Caitlin Bakke42Department of Anesthesiology and Perioperative Medicine, Division of Pain Medicine, Mayo Clinic, Rochester, MN, USA
3Department of Anesthesiology and pain management, Ambulatory Surgery Center, Nura Pain Clinic, Minneapolis MN, USA
4Department of Anesthesiology, Des Moines University of Osteopathic Medical School, USA
Received: 17-May-2021 Published: 07-Jun-2021, DOI: 10.35248/2684-1320.21.7.152
Abstract
Targeted Drug Delivery (TDD) is commonly used for the management of patients with intractable pain. Past studies have proven efficacy in pain relief and reduction in opioid use and cost-effectiveness in long-term pain management. There are few studies investigating satisfaction amongst patients with implanted pain pumps that are managed with targeted intrathecal medications. We published a study in Neuromodulation in April of 2020 describing patient satisfaction with TDD in single medical practice for patients implanted with pain pumps for relief of intractable chronic benign pain. Six hundred and ten active TDD patients were identified, and an anonymous 18-question survey was administered to determine satisfaction with TDD therapy. Four hundred and forty-three patients (74% of the active pump population) completed the survey. Most patients reported improvement in pain, improvement of physical function, improvement in quality of life and reduction in opioid use. Complete discontinuation of oral opioid intake was reported in 38.9% of patients. Most patients had a 40cc reservoir implanted in an upper buttock pocket site and overall, 91% of patients were happy with pump pocket location. We concluded that intrathecal TDD therapy can relieve pain and improve quality of life in patients with intractable pain and offers a reasonable alternative to long-term oral or skin patch opioid management. Patients utilizing TDD therapy reported high degrees of satisfaction. This follow-up article is a general discussion of TDD and our satisfaction survey article.
Keywords
Opioid; Intrathecal medications; Neuromodulation; Neurostimulation
Introduction
Our recent article titled Patient Satisfaction Following Intrathecal Drug Delivery for Chronic Benign Pain: Results of a Single-Center Survey Study, revealed remarkably high patient satisfaction with targeted spinal drug delivery (TDD), confirming what previous studies have also reported [1]. Nonetheless, TDD continues to be a misunderstood and perhaps underutilized therapy. In view of the ongoing opioid crisis in the United States, TDD offers a viable alternative to systemic opioids for the treatment of intractable chronic benign pain, providing better analgesia with fewer mental side effects [2].
As anesthesiology pain specialists, we have collectively performed several thousand trials and implants of implantable pain control systems to treat chronic benign pain. In our pain clinic medical practices, we follow an interventional algorithm from simple (epidural steroid injection) to advanced (implantable pain control) therapies to relieve pain, improve function, and reduce dependence on systemic opioids. We consider TDD to be the last stop in this pathway and reserve it as a last resort option for the most complex and refractory pain problems. We typically trial neurostimulation prior to TDD because we consider neurostimulation to be less drastic and overall lower risk. Regardless, some patients will not respond to the neurostimulation trial, and over time neurostimulation has been reported to have a failure rate approaching 50% [3]. Our TDD trials, on the other hand, have a success rate over 90%, undoubtedly because we use bupivacaine/fentanyl bolus dosing for our trials, which has the potential to create surgical anesthesia at higher doses. We choose bupivacaine/fentanyl for our trials because we use bupivacaine/fentanyl with continuous infusion plus bolus dosing for pump maintenance and we want the trial to mimic what the pump will do after implant.
When a patient comes to the end of our interventional treatment path and undergoes a trial and subsequent surgical implantation of either a neurostimulation system or a pain pump, we typically interact with this patient regularly in the pain clinic for years (sometimes decades) after implant to optimize therapy and manage chronic pain. We have long been in the habit of asking patients who have implanted neurostimulators or pain pumps about their experience and satisfaction with their implanted system. Over the years we have been impressed by the differing responses we hear from neurostimulation patients compared to patients with an implanted pain pump for targeted spinal drug delivery. The neurostimulation patients typically tell us their system is “OK” and moderately helpful, whereas the pain pump patients often rave about their pump with statements like “the best thing I ever did”, “could not live without it”, and “wish I had done it sooner”. Elated feedback from patients treated for chronic benign pain is quite rare in the pain clinic and we do not often hear it with any other therapy. Of course, a minority of patients with either implanted system is dissatisfied with their therapy.
Literature Review
Interestingly, those dissatisfied patients with neurostimulation systems often want the system removed, which is apparent from the 20%-30% removal rate for neurostimulators [4,5].With dissatisfied pain pump patients however, very few will agree to have their systems removed, and this is consistent with the recently published 99% elective re-implant rate for pain pump patients with expiring pumps [6].
As anesthesiologists, we have always been impressed with the power of spinal local anesthetic to stop the pain of labor (epidural) and to provide surgical anesthesia (epidural or intrathecal). The problem with using epidural local anesthetic for chronic pain management is that a single injection will last only for a few hours and the system must run at a continuous high volume (5-15cc per hour) to provide ongoing pain relief. This means that any patient with an epidural pain control system must have an external pump and bag of fluid to maintain long-term pain relief, a burden that makes epidural analgesia impractical for most outpatient pain management.
Although the quality of analgesia is somewhat different with intrathecal local anesthetic (less regional, more diffuse), it is effective at much lower dosages compared to epidural administration since medication is deposited directly onto the spinal cord rather than into the epidural space. Therefore, local anesthetic in a TDD pain pump is effective with flow rates of less than Ice per 24 hours, making intrathecal local anesthetic suitable for chronic pain management.
Regarding our recently published study, we felt compelled to study the pain pump patient experience in a more scientific fashion after years of positive feedback from pain pump patients. We therefore developed a 20-question, anonymous patient survey which we administered to pump patients during one of their return management visits to our pain clinic (Nura Pain Clinic, Minneapolis). The survey was completely voluntary and was provided to our 600 managed pump patients with a response rate of 74% (443 patients elected to complete the questionnaire). We found that our anecdotal experience of positive feedback from pump patients was mirrored in the patient questionnaire responses. 96% of patients reported significant benefit from TDD and over 85% reported improvement in quality of life. 94% reported improved pain relief and 60% reported good to excellent pain relief with TDD. 78% of respondents reported improved physical functioning after pump implant. 77% had not been to the hospital or ER at all since implant and another 15% reported seeking hospital care less often. Almost 90% of patients reported taking less systemic opioids after implant and nearly 40% had stopped systemic opioids completely (DS standard practice is to reduce systemic opioids over time to a maximum of one opioid pill per day for breakthrough pain). Regarding side effects, 93% of patients reported no or manageable side effects from TDD. In addition to our questions, we provided a free text box in the survey and asked respondents to supply any additional feedback in their own words. Although there were a few negative comments, the majority were similar to what patients had been telling us for years:
“I can honestly say that I would not be alive without the pump.”
“The pump is the best thing I ever did.”
“My pump literally saved my life.”
“Best thing I ever did for myself and my family.”
Discussion
From the survey results we confirmed what we already knew - most of our pump patients found targeted drug delivery to be a beneficial, life-enhancing therapy. What we failed to determine was which particulars of the therapy correlated with satisfaction. Since the survey was entirely anonymous, we could not relate the diagnosis for implant, doses of pump medications, catheter tip location, or any other variable to degree of patient satisfaction.
Despite the lack of randomized, controlled scientific data, as experienced implanters with many years of experience, we have come to believe that certain approaches to pump management result in better outcomes and increased patient satisfaction. For instance, we believe that medication admixtures allow for better pain relief at lower drug dosages and that bupivacaine is an equally important medication to opioid in the pump. The synergy of intrathecal opioids which bind to spinal mu receptors and local anesthetics which block nerve conduction is very powerful. We believe that adding low dose baclofen (100 mcg per 24 hours or less) is helpful for selected chronic pain patients with chronic muscle spasm. We have found that giving the patient more control with the liberal use of patient-administered bolus dosing results in higher satisfaction. We also believe that trialing TDD before implant does not improve outcomes, a belief which is supported by current scientific literature [7].
Although we are not against TDD micro-dosing [8], we have not been able to make this work in his practice. Although, we certainly would like to discontinue systemic opioid use prior to TDD trial and implant, many of our patients have trouble reducing their oral or skin patch opioids even by a small percentage. We strongly encourage our patients to reduce opioids by at least 50% prior to trial and implant, but do not refuse implant for those who cannot comply. On the other hand, after permanent implant we are quite firm about tapering and discontinuing systemic opioids over time as we increase intrathecal medication dosages. We are liberal with the use of pre-programmed, patient-administered bolus doses which we encourage our patients to use in lieu of pain pills. The process of increasing pump medications and decreasing systemic opioids down to very low doses or discontinuing them altogether may take us weeks or months, but usually not years.
From our anonymous survey, the best we can deduce is that our standard approach of using bupivacaine/fentanyl as the mainstay pump infusion with liberal patient bolus dosing results in high patient satisfaction. Most of our pumps deliver an admixture of fentanyl and bupivacaine at doses ranging from 100 to 1000 meg fentanyl and 2 to 20 mg bupivacaine per 24 hours. Most patients have a continuous infusion running at relatively low dose with patient-administered bolus doses throughout the day as needed. Some of our pumps contain morphine or hydromorphone instead of fentanyl and occasionally we also add clonidine and/or low-dose baclofen to the opioid-local anesthetic mixture. Our survey results did not allow us to determine which medication combinations at which dosages resulted in best outcomes. Were higher doses correlated with higher satisfaction or more side effects? Was fentanyl better than morphine or hydromorphone? What about pumps with no bupivacaine, was pain relief worse in this group? Was the location of the catheter tip at the spinal level of pain and/or at a location anterior or posterior to the spinal cord important to outcomes? We can’t tell from our study results.
In view of the limitations of our anonymous satisfaction survey, we are currently developing a new study protocol that will involve a similar patient satisfaction survey without anonymity so that we may correlate the details of medications, dosages, catheter tip locations, pump size, pump pocket location and use of bolus dosing with outcomes of pain relief, side effects, physical functioning, health care utilization and overall satisfaction.
Conclusion
Our current opinion is that targeted drug delivery with an implanted, programmable pump and an intrathecal catheter with tip location at the site of maximum pain is the best therapy for the most difficult pain problems. We now want to prove exactly which medications, doses and methods of management work best.
REFERENCES
- Schultz MD, Orhurhu V, Khan F, Hagedorn JM, Abd-Elsayed A. Patient Satisfaction Following Intrathecal Targeted Drug Delivery for Benign Chronic Pain: Results of a Single-Center Survey Study. Neuromodulation. 2020; 23(7):1009-1017
- Smith TJ, Staats PS, Deer T, Stearns JL, Rauck LR, Boortz-Marx LR, et al. Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J Clin Oncol. 2002; 20(19):4040-4049.
- Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, Molet J, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: A multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007; 132(1-2):179-188.
- Hagedorn JM, Lam CM, D’Souza RS, Sayed D, Bendel AM, Ha TC, et al. Explantation of 10 kHz Spinal Cord Stimulation Devices: A Retrospective Review of 744 Patients Followed for at Least 12 Months. Neuromodulation. 2021; 24(3):499-506
- Hayek SM, Veizi E, Hanes M. Treatment-limiting complications of percutaneous spinal cord stimulator implants: a review of eight years of experience from an academic center database. Neuromodulation. 2015; 18:603-608, discussion 8-9.
- Schultz MD, Abd-Elsayed A, Calodney A, Stromberg K, Weaver T, Spencer JR. Targeted Drug Delivery for Chronic Nonmalignant Pain: Longitudinal Data From the Product Surveillance Registry. Neuromodulation. 2020;
- Schultz MD, Abd-Elsayed A, Calodney A, Stromberg K, Weaver T, Spencer JR. Targeted Drug Delivery for Chronic Nonmalignant Pain: Longitudinal Data From the Product Surveillance Registry. Neuromodulation. 2020;
- Sayed D, Monroe F, Orr NW, Phadnis M, Khan WT, Braun E, et al. Retrospective Analysis of Intrathecal Drug Delivery: Outcomes, Efficacy, and Risk for Cancer-Related Pain at a High Volume Academic Medical Center. Neuromodulation. 2018; 21(7):660-663.
Citation: Schultz D, Hagedorn MJ, Stayner S, Bakke C (2021) Discussion of Targeted Drug Delivery Article. J Pain Manage Med. 7:152.
Copyright: © 2021 Schultz D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.