Indexed In
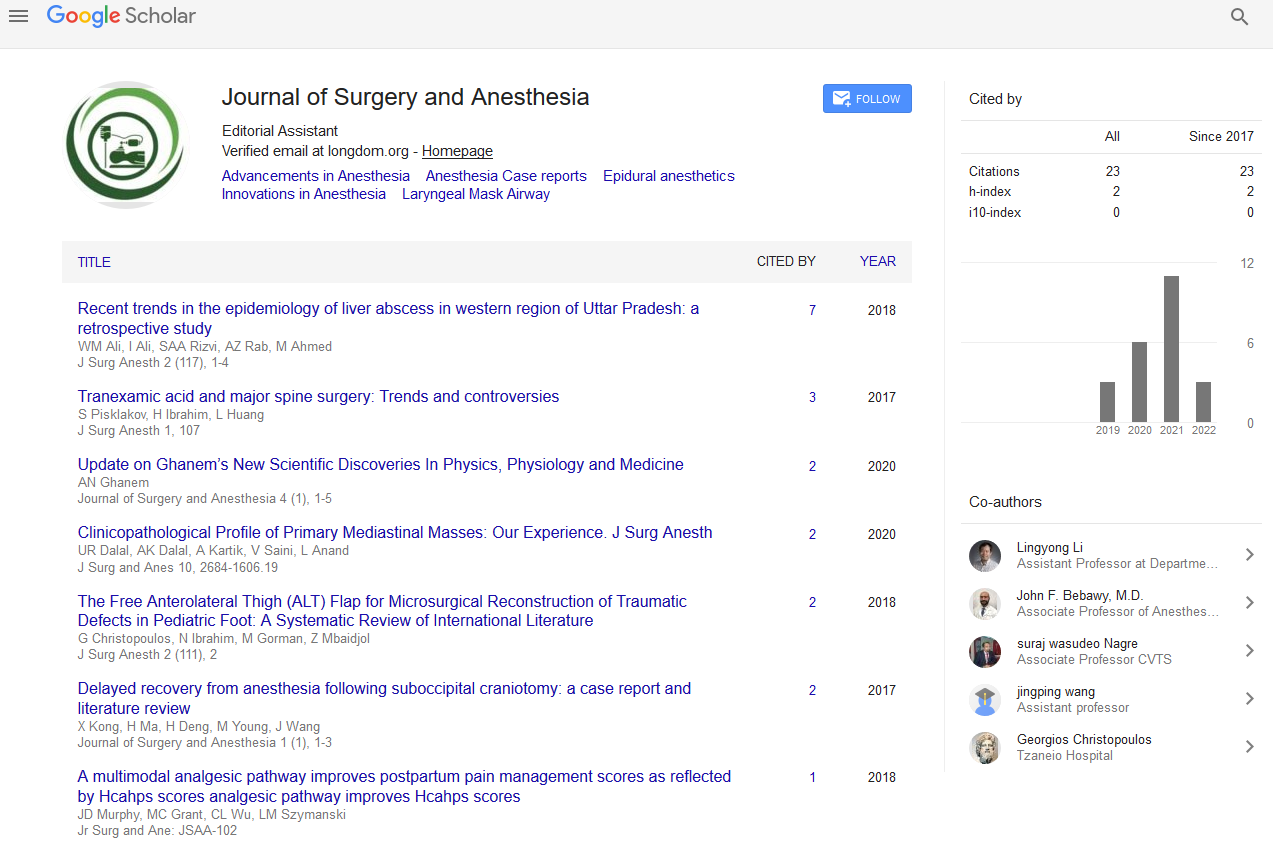
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 4, Issue 2
Differences in Opioid Prescribing Attitudes, Perceptions and Practices of Surgical Providers
Heather F Thiesset1,2*, Karen C Schliep2, Lyen C Huang1, Virginia L Valentin2, Lisa H Gren2 and Christina A Porucznik22Department of Family and Preventive Medicine, Division of Public Health, University of Utah, Salt Lake City, UT 84108, USA
Received: 08-Jul-2020 Published: 01-Aug-2020, DOI: 10.35248/2684-1606.2020.4.132
Abstract
Background: Over-prescription of opioids after surgery puts patients at high-risk for developing chronic opioid dependence. Little is known regarding the use of the Centers for Disease Control and Prevention (CDC) opioid prescribing guidelines in the post-surgical environment.
Materials and methods: This study was a descriptive cross-sectional study looking at surgical provider opioid prescribing. Descriptive statistics were performed.
Results: APCs (70%) were more likely to report use of CDC guidelines in surgery than surgeons (39%) and trainees (32%). Only 14% of surgeons, 22% of trainees, and 8% of APCs identified themselves as having the responsibility to counsel patients on opioid disposal.
Conclusions: Exposure to surgery and thereby opioid narcotics comes with a substantial public health burden and peril to the communities in which the hospitals are located. Therefore, understanding provider perceptions can guide training and affords an opportunity for practice improvement efforts.
Keywords
Opioids; Education; Prescribing providers
Introduction
Opioid misuse and dependence has reached epidemic proportions in recent years with 72,000 fatal overdoses in 2017 related to prescription pain relievers [1]. Over-prescription of opioids after surgery puts patients at high-risk for developing chronic opioid dependence. Previous studies suggest that 6-10% of previously opioid-naïve patients develop dependence in the year after surgery [2].
In 2016, the CDC developed guidelines for prescribing opioids for patients with chronic pain and subsequent management [3]. While these guidelines are targeted at primary care providers treating chronic pain, many of the principles are considered best practices in prescribing opioids. The guidelines recommend minimizing the dose and duration of exposure to opioids and encourage prescribers to counsel patients about the dangers of opioids and to provide individualized tapering plans [4]. Although other groups have published surgery-specific guidelines [4-6], the CDC has yet to do so, nor to provide a consensus document.
Studies examining prescriber attitudes, beliefs, and practices have been conducted in the primary care setting and showed that providers were unaware of CDC guidelines and other published recommendations [7-10]. However, little is known about the attitudes, beliefs, and practices of surgical providers and how they may differ by role. Previous studies suggest that advanced practice clinicians (APCs), comprised of both physician assistants (PAs) and nurse practitioners (NPs), may be more responsive to educational interventions encouraging them to change their opioid prescribing practices than surgeons or trainees (residents and fellows) [11,12].
The purpose of this study was to explore whether surgical providers (surgeons, residents/fellows (trainees), and APCs) are aware of, and applying, the CDC opioid best practice prescribing guidelines. In addition, the study examines whether there are differences between surgeons, trainees, and APCs in their beliefs and perceptions of opioid prescribing. The goal was to determine the impact the CDC guidelines have or have not had in the practice of surgery and to identify potential barriers for future interventions to reduce opioid over-prescribing after surgery.
Methods
A single institution descriptive cross-sectional study was carried out at a tertiary academic medical center between July and September 2018. The study examined differences in surgical provider opioid prescribing. The Institutional Review Board approved this study.
Survey
An anonymous, 35 question instrument including multiple choice and five-point Likert scale items was developed with an expert committee. The questionnaire was then iteratively pilot tested with four volunteer surgeons from different disciplines within the target population, who reviewed the questions for content applicability. Changes were made based on feedback received and applied to the final questionnaire. The questionnaire assessed attitudes, perceptions, and self-reported practices of surgical providers regarding opioid prescribing and concordance with practices described in the 2016 CDC prescribing guidelines for opioids, in the post-surgical patient.
During July through September 2018, an electronic link to the web-based REDCap [13] questionnaire was provided to 242 providers (surgeons, trainees, and advanced practice clinicians (APCs)) in nine surgical disciplines at a tertiary academic medical center. Disciplines included Abdominal Transplantation and Advanced Hepatobiliary Surgery, Cardiothoracic Surgery, Emergency Medicine, General Surgery, Otolaryngology, Pediatric Surgery, Plastic Surgery, Urology, and Vascular Surgery.
Statistical analysis
Univariate analyses were conducted using the chi-squared tests, student’s t-tests, or Fisher’s exact test, as appropriate. Frequency statistics compared differences in attitudes, perceptions, and practices by role, age, and time in practice. The primary outcome of interest was the provider reported variable of current use of CDC guidelines in surgery. Prevalence ratios were generated using log-binomial models with surgeons as the reference group for dichotomous variables. Covariates were adjusted on age and gender. Data analysis was completed using Stata 15.1 software (College Station, TX).
Results
A total of 153/242 participants (64% response rate) responded to the questionnaire, with 86 (56%) surgeons, 31 (20%) trainees, and 36 (24%) APCs. Most respondents were male (80%) (Table 1).
| Surgeons (n=86) | Residents/Fellows (n=31) | APCs (n=36) | |
|---|---|---|---|
| Gender | |||
| Male | 69 (80%) | 20 (65%) | 12 (34%) |
| Female | 17 (20%) | 11 (35%) | 23 (66%) |
| Age | |||
| 20-29 | 0 | 4 (13%) | 10 (29%) |
| 30-39 | 22 (26%) | 27 (87%) | 11 (31%) |
| 40-49 | 39 (44%) | 0 | 7 (20%) |
| 50-59 | 19 (21%) | 0 | 4 (11%) |
| >60 | 7 (9%) | 0 | 3 (9%) |
| Years in practice | |||
| <5 | 26 (30%) | n/a | 12 (40%) |
| 05-Sep | 16 (19%) | n/a | 9 (30%) |
| Oct-20 | 28 (32%) | n/a | 5 (17%) |
| >20 | 16 (19%) | n/a | 4 (13%) |
Table 1: Characteristics of survey respondents, by role.
Overall, all groups (surgeons 85%, trainees 82%, and APCs 81%) of providers reported being either very comfortable or comfortable prescribing opioids (Table 2). However, when asked about provider knowledge of 2016 CDC opioid prescribing guidelines, most APCs (70%) reported that they currently use the guidelines in their practice while only 32% of surgeons and 39% of trainees reported such. APCs responded that the guidelines had applicability to their practice (11%) compared to 10% of surgeons and 19% of trainees who acknowledged their applicability, but most respondents in all groups chose the neutral category. APCs (36%) were also more likely than surgeons (15%) and trainees (6%) to implement standardized opioid taper protocols for their patients (Surgeon 15% vs. APCs (36%), PR=4.93, 95% CI 1.4-17.4), (Surgeon 15% vs. trainees (6%) PR=0.72, 95% CI 0.11-4.75) (Table 2) when controlling for age and gender.
| Attitudes/Perceptions | ||||
|---|---|---|---|---|
| Surgeons (n=86) | Residents/fellows (n=31) | APCs (n=36) | ||
| How would you describe your knowledge about CDC guidelines for opioid prescribing practices? | Currently utilize them in practice | 27 (32%) | 12 (39%) | 25 (70%) |
| Reviewed but don’t use them | 9 (11%) | 2 (6%) | 3 (8%) | |
| Know they exist, but they don’t change my practice | 29 (35%) | 8 (26%) | 5 (14%) | |
| Not aware of the guidelines | 19 (22%) | 9 (29%) | 3 (8%) | |
| How much do you feel that the CDC guidelines for opioid prescribing practices are applicable in your surgical practice? | Very applicable/ applicable | 8 (10%) | 6 (19%) | 4 (11%) |
| Neutral | 37 (45%) | 16 (52%) | 18 (50%) | |
| Somewhat applicable/ Not applicable | 17 (20%) | 5 (16%) | 10 (28%) | |
| Not sure | 21 (25%) | 4 (13%) | 4 (11%) | |
| How comfortable do you feel prescribing opioids? | Very comfortable/ comfortable | 73 (85%) | 25 (82%) | 29 (81%) |
| Neutral | 9 (10%) | 3 (9%) | 6 (17%) | |
| Slightly uncomfortable/ uncomfortable | 4 (5%) | 3 (9%) | 1 (2%) | |
| Who should be predominantly responsible for counseling patients on proper opioid disposal? | RN | 13 (15%) | 3 (9%) | 0 |
| Attending surgeon | 12 (14%) | 7 (24%) | 0 | |
| PHARMD | 42 (49%) | 16 (52%) | 14 (39%) | |
| Care coordinator | 6 (7%) | 1 (3%) | 1 (3%) | |
| APC | 4 (5%) | 1 (3%) | 3 (8%) | |
| Primary care physician | 6 (7%) | 3 (9%) | 14 (39%) | |
| Other | 3 (3%) | 0 | 4 (11%) | |
| Practices | ||||
| How often do you feel that patients receive counseling in your practice regarding the use of opioids? | Always | 33 (39%) | 6 (19%) | 21 (58%) |
| Sometimes | 38 (44%) | 16 (52%) | 11 (31%) | |
| Never | 15 (17%) | 9 (29%) | 4 (11%) | |
| How often do you or a member of your team create a taper schedule for patients after prescribing them opioids? | Almost always/ Always | 6 (7%) | 2 (6%) | 13 (36%) |
| Sometimes | 32 (38%) | 11 (36%) | 13 (36%) | |
| Almost never/ never | 46 (55%) | 18 (58%) | 10 (28%) | |
| Do you feel you have adequate time to counsel patients on proper opioid disposal? | Always | 13 (15%) | 2 (6%) | 13 (36%) |
| Sometimes | 23 (27%) | 11 (36%) | 9 (25%) | |
| Never | 50 (58%) | 18 (58%) | 14 (%) | |
| For patients with a past medical history of opioid abuse what is your standard protocol? | Give fewer with no refills | 8 (10%) | 7 (23%) | 9 (28%) |
| Consult with pain management team | 54 (68%) | 13 (42%) | 18 (56%) | |
| No difference in treatment | 18 (23%) | 11 (35%) | 5 (16%) | |
Table 2: Comparison survey respondents, by role.
Only 14% of surgeons, 22% of trainees, and 8% of APC ’ s identified themselves as having the responsibility to counsel patients on opioid disposal. Surgeons (49%) and trainees (52%) were more likely to assign the responsibility to counsel patients on opioid disposal to pharmacists than APCs, who were split in their responses between pharmacists (39%) and primary care physicians (39%) having the responsibility. Furthermore, 58% of surgeons and trainees, as opposed to 39% of APCs identified as not having adequate time to counsel their patients on opioid disposal. All groups reported similar prevalence of knowledge of opioid disposal options and agreed that the patient has the primary responsibility for opioid disposal as opposed to prescribing providers.
Surgeons more frequently chose the option of consulting with a pain management team (68%) than APCs (56%) or trainees (42%) for patients with a past medical history of opioid abuse. Trainees were also more likely (23% compared to 16% for APCs, and 35% for surgeons to have no self-reported difference in treatment practice for patients with such history (Table 2).
The primary outcome of interest was the provider reported variable of current use of CDC guidelines for surgical patients. APCs were more likely to report use of CDC guidelines in surgery than surgeons and trainees when controlling for age and gender (39% vs. 70%, PR=4.89, 95% CI 1.8-13.6) (39% vs. 32%, PR=1.28, 95% CI 0.4-3.8).
Discussion
The current study investigated the beliefs and perceptions of surgeons and APCs across multiple disciplines at a single academic institution. We found that APCs (70%) were more likely to be aware of and use CDC guidelines to guide their practices than surgeons (32%) or trainees (39%). A large proportion of APCs (28%), trainees (16%) and surgeons (20%) felt that CDC guidelines were only somewhat applicable or not applicable to their practice. Surgical providers may not be aware of and deem guidelines are applicable because they are written for primary care providers. So surgical provider’s reluctance to engage with the CDC guidelines may not be unreasonable since they are not the primary audience, even though the counsel is applicable on a broader level to all prescribing providers.
Consistent with studies from the primary care literature [7,10,12,14], we found that few surgical providers were aware of CDC guidelines or used them in their prescribing practices. One explanation this study found is that less than half of surgical providers believe that the CDC opioid guidelines are applicable to their practice. Though several other groups have published recommendations for dosing on select surgical procedures [5,6], there may still be a role for the CDC to publish a consensus guideline. Providers may also be hesitant to adopt external guidelines as many feel they have the experience and knowledge to appropriately prescribe already [8].
Interestingly, our study found that APCs were more likely to be aware of and apply the CDC guidelines in their practice. One of the guidelines is creating taper protocols for patients. APCs were more likely to create taper protocols for their patients than surgeons in our study, which is consistent with other literature where providers acknowledged seeing the importance of developing specific guidelines for opioid use after discharge [12]. In many surgical practices, APCs have taken over the day-to-day management of patients and may therefore be more likely to perceive the applicability of CDC guidelines. This finding may also tie into the fact that APCs are spending more individual time with the patient due to surgeon time limitations. A system wide approach may be useful when ensuring that tapering protocols are individualized to the patient instead of a standardized order set within a care pathway. Furthermore, counseling in the pre-operative setting may potentially decrease opioid use and the risks associated with opioids in the postoperative setting [15].
Our study found that surgical providers, regardless of role, often expected others (e.g. pharmacists, primary care providers) to be responsible for counseling patients on the benefits, risks, and disposal of opioids. One explanation is that surgical providers lack the time to counsel patients on opioids, with less than half (42% surgeons, 42% trainees, and 61% APCs) reporting they always or sometimes had enough time to counsel patients. Holman, et al. found that preoperative counseling on opioid cessation significantly decreased a patient’s duration of opioid use after surgery [2,15]. Few surgical providers identified themselves as having the responsibility to counsel patients on opioid benefits, risks, and disposal. Pharmacists were the most common health care team member selected to have the responsibility to counsel patients. A future study could obtain the perspective from pharmacists and other health care team members to determine if all members feel the same way: that theirs is not the primary role to counsel patients regarding opioids. Although we did not survey pharmacists or primary care physicians in this study, there may be disconnect if each type of provider is expecting others to provide counseling and education to patients. Another potential barrier is that many surgical providers felt the responsibility for disposal lies with patients. Many of our respondents did not feel knowledgeable about appropriate disposal, which may explain placing responsibility on patients. But there may be another insidious disconnect between surgeons and patients, with each expecting the other to take responsibility for opioid disposal. While patients indeed have a responsibility to physically dispose of their prescriptions, providers should not relinquish all responsibility once they have issued a prescription. At a minimum, that responsibility could take the form of a discharge handout given to patients at the time of issuing an opioid narcotic.
The major limitation of our study is that it was done at a single institution. Homogeneity of the institutional culture and commonalities in the health system may limit the generalizability of our findings. We do not anticipate that this single institution was intrinsically different than other institutions. Another limitation is that the survey depended on self-reporting. We were not able to compare provider responses with their actual prescribing practices as the surveys were anonymous to encourage responses. It is possible that providers may be over-estimating their awareness and application of CDC guidelines or other practices such as tapering recommendations as they view this as socially desirable. Other methods such as qualitative interviews or focus groups may be helpful in identifying potential barriers to improvement.
Conclusions
Over-prescription of opioids after surgery puts patients and their communities at risk. More research such as qualitative interviews with surgical providers is needed to guide the development of interventions such as provider education and health systems support in order to decrease the amount of opioids prescribed after surgery.
This study showed that gaps in provider workflow and responsibility for counseling exist. Furthermore, providers are likely to continue to use standardized scripts instead of individualizing and creating taper plans for their patients. In light of this, it is essential to work with providers to create interventions concordant with their perspectives, roles, and time constraints in order to improve patient safety and decrease the risks associated with misuse and abuse of opioids by patients.
REFERENCES
- National Institute on Drug Abuse. Overdose death rates. 2018.
- Holman JE, Stoddard GJ, Higgins TF. Rates of prescription opiate use before and after injury in patients with orthopaedic trauma and the risk factors for prolonged opiate use. J Bone Joint Surg Am. 2013; 95: 1075-1080.
- Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain-- United States. JAMA. 2016; 315: 1624-1645.
- Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of postoperative pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016; 17: 131-157.
- Hill MV, Stucke RS, Billmeier SE, Kelly JL, Barth RJ. Guideline for discharge opioid prescriptions after inpatient general surgical procedures. J Am Coll Surg. 2018; 226: 996-1003
- Thiels CA, Ubl DS, Yost KJ, Dowdy SC, Mabry TM, Gazelka HM, et al. Results of a prospective, multicenter initiative aimed at developing opioidprescribing guidelines after surgery. Annals of Surgery. 2018; 268: 457-468.
- Jamison SK, Scanlan E, Matthews M, Ross EL. Beliefs and attitudes about opioid prescribing and chronic pain management: survey of primary care providers. J Opioid Manag. 2014; 10: 375-382.
- Johnson SR. New CDC guidelines are unlikely to affect opioid prescribing practices. Mod Healthc. 2016; 46: 11.
- Macerollo AA, Oza R, Bennett IM, Wallace LS. Academic family medicine physicians' confidence and comfort with opioid analgesic prescribing for patients with chronic nonmalignant pain. J Opioid Manag. 2014; 10: 255-261.
- Spitz A, Moore AA, Papaleontiou M, Granieri E, Turner BJ, Reid MC. Primary care providers' perspective on prescribing opioids to older adults with chronic non-cancer pain: a qualitative study. BMC Geriatr. 2011; 11: 35.
- Franklin GM, Fulton-Keho D, Turner JA, Sullivan MD, Wickizer TM. Changes in opioid prescribing for chronic pain in Washington State. J Am Board Fam Med. 2013; 26: 394-400.
- Surmaitis RM, Amaducci A, Henry K, Jong M, Kiernan EA, Kincaid H, et al. Perception and practice among emergency medicine health care providers regarding discharging patients after opioid administration. ClinTher. 2018; 214-223.
- Harrisa PA, Taylor R, Thielkec R, Payned J, Gonzaleze N, Condee JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009; 42: 377-381.
- Wilson HD, Dansie EJ, Kim MS, Moskovitz BL, Chow W, Turk DC. Clinicians' attitudes and beliefs about opioids survey (CAOS): instrument development and results of a national physician survey. J Pain. 2013; 14: 613-627.
- Holman JE, Stoddard GJ, Higgins TF. The effect of preoperative counseling on duration of postoperative opiate use in orthopaedic trauma surgery: A surgeon-based comparative cohort study. J Orthop Trauma. 2014; 502-506.
Citation: Thiesset FH, Schliep KC, Huang LC, Valentin VL, Gren LH, Porucznik CA (2020) Oesophageal Differences in Opioid Prescribing Attitudes, Perceptions, and Practices of Surgical Providers. J Surg Anesth. 4:132.
Copyright: © 2020 Thiesset HF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.