PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
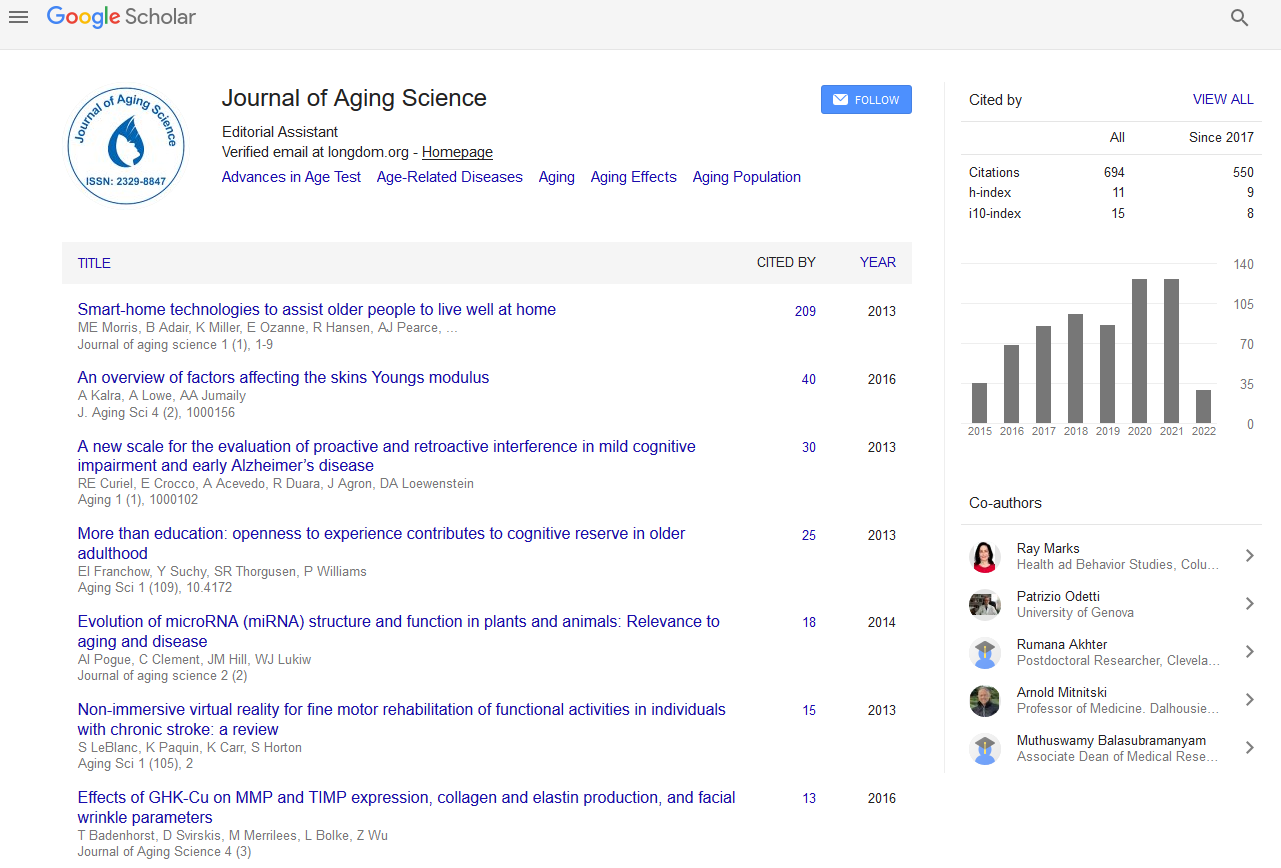
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2020) Volume 8, Issue 4
Current Status and Future of Autologous Cord Blood Stem Cell Therapy for Cerebral Palsy
Haruo Shintaku*Received: 03-Sep-2020 Published: 24-Sep-2020, DOI: 10.35248/2329-8847.20.08.239
Introduction
Human brain tissue has a limited ability to regenerate. Cerebral palsy (CP) is a disorder that results from brain injury, most notably hypoxic ischemic encephalopathy (HIE), during the neonatal period. Once the brain-damaging process has progressed to exhibit CP pathology, there is no effective treatment. Therefore, halting this progressive process is important for preventing or minimizing the severity of CP. Therapeutic hypothermia (TH) is an established method widely practiced for this purpose, and TH alone can decrease the mortality rate without increasing the risk of severe disability among survivors [1]. One recent registry study, however, suggests that nearly half of TH can result in some unwanted after- effects [2]. Stem cell therapy is a newer approach with the potential to repair damaged cells in CP lesions. In 2014, researchers in the United States reported the effectiveness of a combination of TH and autologous cord blood therapy in improving the neurodevelopmental outcome of HIE [3]. By the end of 2014, the Japan Agency for Medical Research and Development funded a clinical trial of autologous cord blood therapy for HIE.
Umbilical Cord Blood Stem Cells and Regenerative Medicine
Stem cells have self-proliferation capacity and pluripotency. Hematopoietic stem cells and mesenchymal stem cells (MSCs), which are ubiquitous in the body, are involved in the maintenance and regeneration of tissues. The use of these cells, called somatic stem cells, is safer and raises fewer ethical concerns than the use of embryonic stem cells. In the neonatal medicine, additional types of stem cells, i.e., cord blood stem cells (CBSCs) and cord-derived MSCs, can be obtained from the umbilical cord, which is usually discarded after delivery. Since the first discovery by Nakahata et al. in 1982 [4], CBSCs has been used to treat Fanconi anemia and HIE [3,5,6].
Treatment Of Hie With Autologous CBSCS
Cotten et al. from Duke University in the United States isolated and administered autologous CBSCs to infants who underwent TH for moderate to severe neonatal HIE [3]. Although the survival rate was similar between TH alone and TH with CBSC therapy, infants who received both TH and CBSCs were more likely to have a better one-year neurodevelopment outcome, as determined by the Bayley II Scale. Based on the results of this study, a phase I trial of autologous CBSC treatment for HIE was conducted in Japan in combination with TH [6,7]. The eligibility criteria were: gestational age of ≥ 36 weeks; birth weight of ≥ 1800 g; moderate or more severe HIE at birth; and family consent. The umbilical cord was punctured, and 40 to 100 mL of cord blood was aseptically collected. CBSCs were aseptically separated by Sepax using a pack containing the separating agent, hydroxyethyl starch. Cells were divided into three doses and intravenously administered for 3 days during TH (Figure 1).
Therapeutic Mechanisms Of CBSCs
Scientific research for neuroregenerative medicine is advancing every day. CBSCs and cord-derived MSCs have been shown to have pluripotency to differentiate into nerve cells in an in vitro experimental system. Interestingly, however, administered CBSCs do not seem to directly replace the damaged nerve cells in the brain.
Instead, CBSCs likely work by improving energy metabolism and promoting tissue repair through angiogenesis at the damaged site [8]. Cord-derived MSCs have been shown to promote regeneration of brain nerve cells by suppressing brain-damaging inflammatory reactions in the acute phase.
From Prevention To Treatment
Until now, the main focus of CP management was prevention, as it is difficult to directly treat CP lesions once they are formed. Recent clinical trials with autologous CBSCs, however, have shown promising results. Sun et al. [9] conducted a randomized placebocontrolled trial of autologous CBSCs in children with CP aged 1 to 7 years and reported that the motor function was significantly improved after 1 year in the group that received more than 2 × 107 of CBSCs. In Japan, Kochi University has started a phase I clinical trial to administer autologous CBSCs to CP children aged 2 to 7 years, and so far its safety has been confirmed in 6 cases.
Thus, the treatment of CP, once considered impossible, is now becoming a reality owing to the progress in regenerative medicine using CBSCs. The future of CBSCs is not limited to CP; for example, clinical trials of CBSCs are underway in children with idiopathic autism spectrum disorder.
Financial Support
This publication was supported by Grant Number JP15bk01040 43h0002,JP16bk0104029h0003, and JP18bk0104004h0001 from the Japan Agency for Medical Research and Development. The commentary also received support from a charity lecture “Disability Medicine and Regenerative Medicine” at the Osaka City University Graduate School of Medicine.
REFERENCES
- Shankaran S, Pappas A, McDonald SA, Vohr BR, Hintz SR, Yolton K, et al. Childhood outcomes after hypothermia for neonatal encephalopathy. N Engl J Med. 2012;366(22): 2085-2092.
- Tsuda K, Mukai T, Iwata S, Shibasaki J, Tokuhisa T, Ioroi T, et al. Therapeutic hypothermia for neonatal encephalopathy: A report from the first 3 years of the baby cooling registry of Japan. Sci Rep. 2017;7: 39508.
- Cotten CM, Murtha AP, Goldberg RN, Grotegut CA, Smith PB, Smith PB, et al. Feasibility of autologous cord blood cells for infants with hypoxic-ischemic encephalopathy. J Pediatr. 2014;164(5): 973-979.e1.
- Nakahata T, Ogawa M. Hemopoietic colony-forming cells in umbilical cord blood with extensive capability to generate mono and multipotential hemopoietic progenitors. J Clin Invest. 1982;70(6): 1324-1328.
- Gluckman E, Broxmeyer HA, Auerbach AD, Friedman HS, Douglas GW. Hematopoietic reconstitution in a patient with Fanconi's anemia by means of umbilical cord blood from an HLA-identical sibling. N Engl J Med. 1989;321(17): 1174-1178.
- Tsuji M, Sawada M, Watabe S, Sano H, Kanai M, Tanaka E, et al. Autologous cord blood cell therapy for neonatal hypoxic ischaemic encephalopathy: A pilot study for feasibility and safety. Sci Rep. 2020; 10: 4603.
- Nabetani M, Shintaku H, Hamazaki T. Future perspectives of cell therapy for neonatal hypoxic ischemic encephalopathy. Pediatr Res. 2018;83: 356-363.
- Kikuchi-Taura A, Okinaka Y, Takeuchi Y, Ogawa Y, Maeda M, Kataoka Y, et al. Bone marrow mononuclear cells activate angiogenesis via gap junction-mediated cell-cell interaction. Stroke. 2020;51(4): 1279-1289.
- Sun JM, Song AW, Case LE, Mikati MA, Gustafson KE, Simmons R, et al. Effect of autologous cord blood infusion on motor function and brain connectivity in young children with cerebral palsy: A randomized, placebo-controlled trial. Stem Cells Transl Med. 2011;6(12): 2071-2078.
Citation: Shintaku H (2020) Current Status and Future of Autologous Cord Blood Stem Cell Therapy for Cerebral Palsy. J Aging Sci. 8: 239. DOI: 10.35248/2329-8847.20.08.239
Copyright: © 2020 Shintaku H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.