Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
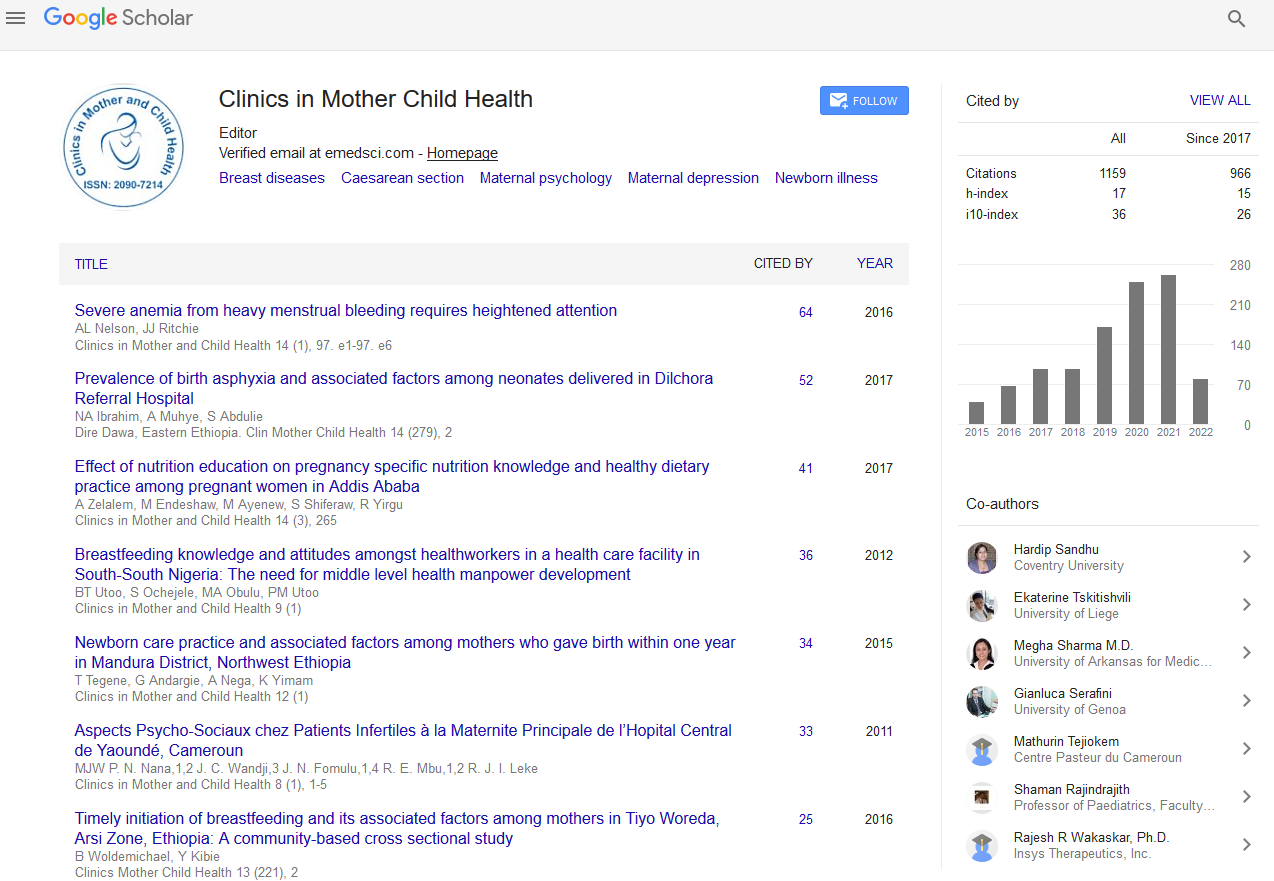
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2021) Volume 18, Issue 3
Congenital Cyanogenic Heart Disease in Children: About 420 Cases in Africa
Amadou Lamine Fall1, Djibril Boiro1, Indou Deme Ly1 and Amadou Sow2*2Abass Ndao Hospital Center, Dakar, Senegal
Received: 05-Feb-2021 Published: 26-Feb-2021, DOI: 10.35248/2090-7214.21.18.379
Abstract
Congenital Cyanogenic Heart Diseases (CCHD) is a malformation of the heart and large vessels characterized by an oxygen desaturation in the arterial blood, responsible for cyanosis. The general objective was to study the profile of CCHD in Senegalese hospitals. This is a retrospective study carried out over a period of 8 years (January 1, 2010 - December 31, 2017) and including all children aged 0 to 16 years followed for a CCHD. The hospital prevalence was 0.87% for 420 cases collected. The sex ratio was 1.44 and the average age at diagnosis was 16 months. First degree parental consanguinity was noted in 36 cases (30.78%). The main reasons for consultation were breathing difficulty in 242 cases (57.62%) and fever in 136 patients (32.36%). Apart from cyanosis, the clinical signs were dominated by the heart murmur in 313 cases (74.7%), tachycardia in 283 cases (67.38%) and digital hippocratism in 162 cases (38.57%). Cardiomegaly was found in 239 patients (83.36%). The main types of CCHD were tetralogy of Fallot and transposition of the large vessels. In biology, 206 patients (49.05%) presented polyglobulia. A complete surgical cure was carried out in 22 patients (5.24%). Complications were anoxic crisis (52 cases) and hemorrhagic syndrome (17 cases). There were 97 deaths (28.28%) during hospitalization. The diagnosis of CCHD is late in our country and surgical management is poor explaining the high mortality.
Keywords
Heart disease; Cyanosis; Tetralogy Fallot; Surgery, Senegal
Introduction
Congenital cyanogenic heart diseases (CCHD) are malformations of the heart and large vessels characterized by an oxygen desaturation in the arterial blood, responsible for a blue coloration of the mucous membranes and the integuments or cyanosis [1]. According to a last study in Senegal, CCHD represents 36.95% of all congenital heart diseases (CHC). Despite considerable advances in diagnosis with the contribution of cardiac ultrasound coupled with color doppler as well as progress in management with the development of pediatric cardiology and cardiovascular surgery, CCHD remains a major public health problem [2]. Studies have been carried out in our country on CHC in general but not specifically on CCHD [3,4]. Thus, we carried out this work to study the profile of CCHD in Senegalese hospitals.
Methodology
This is a retrospective and descriptive study carried out at the Albert Royer National Children's Hospital (ARNCH) which is a benchmark public hospital for pediatric care in Senegal. It houses a pediatric cardiology department where the majority of children suffering from congenital or acquired heart disease are followed. The study was carried out over an 8-year period from January 1, 2010 to December 31, 2017 and including all children aged 0 to 16 years followed for CCHD confirmed on echocardiography by a pediatric cardiologist. The epidemiological, diagnostic, therapeutic and evolutionary parameters were informed from medical records and hospital registers. The data were entered with the Epi Info version 7 software. The qualitative variables were assessed by determining the numbers, the percentages and highlighting the mode.
Results
During the study, 420 patients were collected for CCHD including 343 (81.67%) in hospital with a prevalence of 0.87% (343/39336). The sex ratio was 1.44 and the average age at diagnosis was 16 months [extreme 0 day-126 months]. No antenatal diagnosis has been made. First degree parental consanguinity was noted in 36 patients (30.78%) and second degree consanguinity in 56 patients (47.86%). The age of the mothers was between 20 and 29 years for 116 patients (49.36%). Family socioeconomic level was low for 130 patients (60.19%). Among the patients, 135 (77.59%) were of low birth weight. The main reasons for consultations were breathing difficulty for 242 patients (57.62%), fever for 136 patients (32.36%) and cough for 92 patients (21.9%). The main clinical signs are summarized in Table 1. Bronchiolitis was associated with CCHD in 84 patients (55.63%) and trisomy 21 in 15 patients (3.3%).
Radiological cardiomegaly was found in 239 patients (83.36%). The main types of CCHD found on cardiac ultrasound. In biology, 206 patients (49.05%) presented polyglobulia, 153 patients (36.4%) had anemia and 135 patients (32, 14%) hyponatremia. Therapeutically, 214 patients (58.63%) were on loop diuretics, 204 patients (55.89%) on beta-blockers, 35 patients (9.59%) on digitalis and 67 patients (18.36%) on converting enzyme inhibitors. A complete surgical cure was performed in 22 patients (5.24%) including 15 cases of Tetralogy of Fallot (T4F). The average age at surgery was 52 months [4 months -132 months]. Among the patients, 9 had undergone a Blalock and 10 others had an interventional catheterization of Rashkind. The evolution in hospitalization was favorable in 246/343 hospitalized or 71.72%. Complications were dominated by anoxic discomfort (52 cases) and hemorrhagic syndrome (17 cases). We deplored 97 deaths (28.28%) during hospitalization. Out of 420 patients, 202 were followed up remotely with 17 deaths (8.42%) at an average age of 18 months [range 3 months and 60 months]. The epidemiological, paraclinical and evolutionary features of the main types of CCHD are reported.
Discussion
The hospital prevalence of CCHD seems to increase over the years with 0.87% in our study against 0.18% in 2011 [3]. This could be explained by the raising of the technical platform, the availability of cardiac ultrasound and the development of pediatric cardiology. The tetralogy of Fallot (T4F) remains the most frequent CCHD in our series as observed in several other studies [3, 4, 5]. The other types of CCHD most commonly found were the transposition of large vessels (TLV),the Double Issue Right Ventricle (DIRV) and Tricuspid atresia (TA).However, some severe CCHD are often lethal in the fetal or neonatal period and are underdiagnosed. The male prevalence observed in CCHD has been described in several other studies, but a direct correlation between sex and the occurrence of CCHD has not been established [6, 4]. There was a high percentage of parental consanguinity (92.12%). Studies have shown that there is a correlation between parental consanguinity and the genesis of heart defects [7, 8]. The main genetic anomaly was trisomy 21 as described in the literature [9]. The average age at diagnosis was 16 months. This delay in diagnosis is explained by the fact that in our developing countries, the discovery is often made after decompensation due to a lack of diagnostic means and limited access to patient care linked to the low socioeconomic level [6]. The age at diagnosis is later in T4F (25 months), the single ventricle (39 months) and tricuspid open septum atresia (23 months) because of the later onset of cyanosis. Unlike other types of CCHD where it appears earlier. This situation contrasts with that of developed countries where the diagnosis is often made in antenatal [10]. The main reasons for consultation were respiratory signs and the main associated pathology was bronchiolitis. Respiratory infections are frequent revealing circumstances. In biology we note a predominance of polyglobulia which is the consequence of hypoxia. This hypoxia was also at the origin of the frequent anoxic crisis in T4F. The number of patients who have undergone surgical treatment remains very low compared to Western countries. This would be linked on the one hand to the high cost of cardiac surgery and on the other hand to an insufficiency of the surgical technical platform. The medical treatment consisted mainly in the prevention of anoxic crises and in the management of associated pathologies. Surgical repair is indicated in all cases for T4F. The medical and surgical management of TLV and DIRV remains difficult due to their brutal and early revelations. Despite all the actions taken to improve care, there is a considerable gap between the number of children in need of surgical treatment and those who benefit from it. This explains the high mortality in our country. This mortality seems lower in T4F compared to other types of CCHD.
Conclusion
The diagnosis of CCHD is late in our country and surgical management is poor explaining a high mortality. This is linked to a difficulty in accessing diagnostic means and the limits of the technical platform. Improving the prognosis of CCHD requires the establishment of antenatal diagnosis, extensive neonatal screening for cardiac anomalies; the raising of technical platforms in the pediatric and maternity departments as well as the strengthening of resources in the cardiovascular surgery department.
REFERENCES
- Almalki M, Fitzgerald G, Clark M. Health care system in Saudi Arabia: an overview. East Mediterrean J. 2012;17:784-93.
- Awases MH, Bezuidenhout MC, Roos JH. Factors affecting the performance of professional nurses in Namibia. Curationis. 2013;36:8.
- Borrelli S. What is a good midwife? Insights from the literature. United Kingdom. The University of Nottingham. Queen's Medical Centre Medical School. 2013;310.
- Falconer AD. Millennium Goal 5. Obstet Gynaecol Reprod Med. 2010; 20:369-371.
- Filippi V, Chou D, Ronsmans C, Graham W, Say L. Reproductive, maternal, newborn, and child health: disease control priorities. London School of Hygiene and Tropical Medicine. 2010;2:3.
- Ministry of Health-MOH. Health first quarter 2018 report, unpublished report. PHIS, MOH, Gaza Strip, 2018.
- Ministry of Health, PHIC, Health Status, Palestine, 2018.
- Ministry of Health-MOH. Health annual report, Palestine 2016. General directorate of health policies and planning. PHIS, MOH, Ramallah, 2017.
- Mollart L, Skinner V, Newing C, Foureurc M. Factors that may influence midwives work related stress and burn out maternity services, Australia. Women and Birth. 2011;26:26-32.
- Nabirye RC, Brown KC, Pryor ER, Maples EH. Occupational stress, job satisfaction and job performance among hospital nurses in Kampala, Uganda. J Nurs Manag. 2011;19:760-768.
Citation: Fall LA, Boiro D, Deme Ly I, Sow A (2021) Congenital Cyanogenic Heart Disease in children: About 420 Cases in Africa. Clinics Mother Child Health. 18: 379
Copyright: © 2021 Sow A This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.