PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
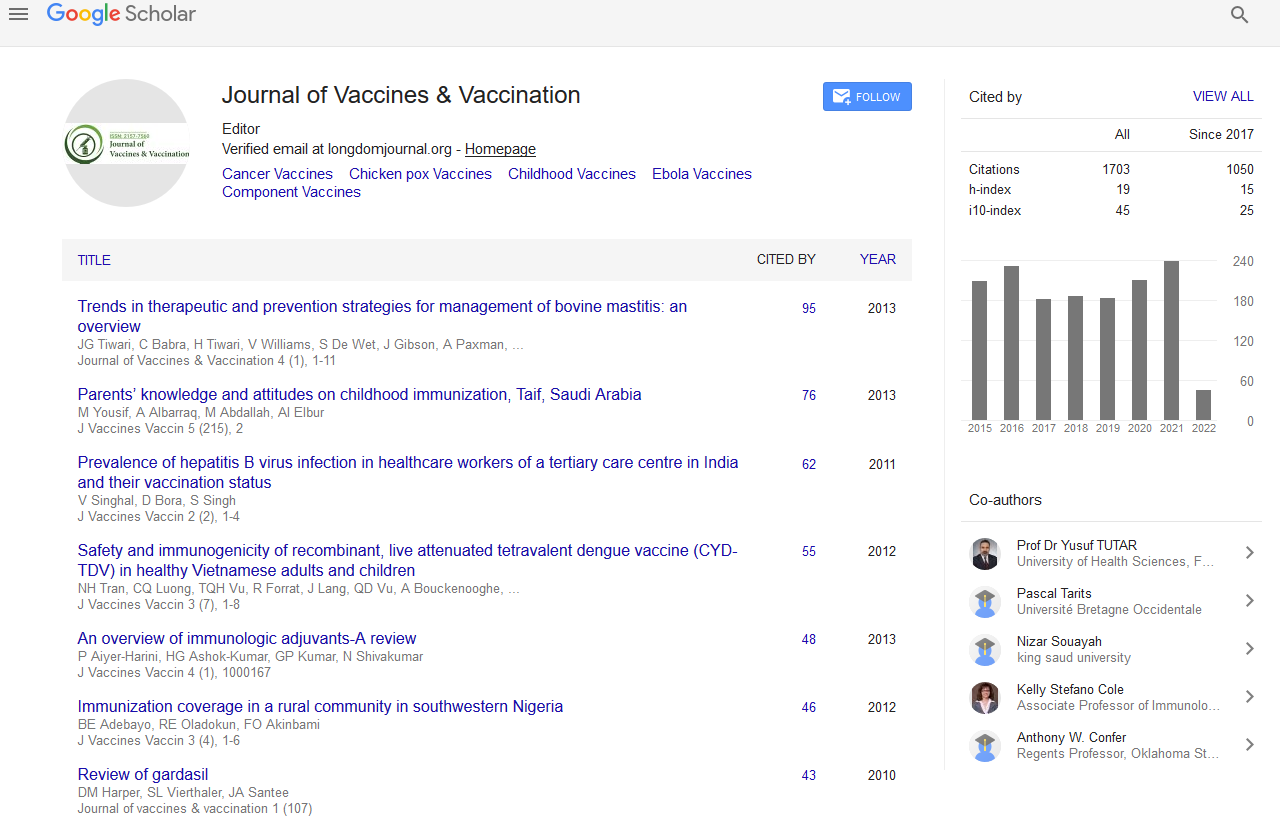
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review Article - (2020) Volume 11, Issue 7
Comparative Analysis of Emerging Viruses to Inform Development of Safe and Effective Vaccines for COVID-19
Sabiha Noor1, Shabnam Sambyal2, Saif Ismail3 and Narendra Chirmule4*2Department of Immunology, Shoolini University, Himachal Pradesh, India
3Department of Immunology, Sun Pharma Industries, Maharashtra, India
4Department of Immunology, SymphonyTech Biologics, Bangalore, Karnataka, India
Received: 01-Dec-2020 Published: 22-Dec-2020, DOI: 10.35248/2157-7560.11.7.440
Abstract
Viruses have evolved by surviving in hosts over millions of years. The human immune system has also co-evolved to counter the escape mechanisms of viruses. Each virus has a unique and specific mechanism of causing disease. SARS-COV2 has emerged as a newly mutated virus that has resulted in a world-wide pandemic. Understanding immunobiology of viruses provides information on developing diagnostics, therapeutics, and vaccines. We have reviewed and summarized the pathogenesis of four viruses that have emerged as causative agents for endemics in the past decade. Dengue, Chikungunya, Nipah and Zika viruses i) are transmitted by different intermediate animal hosts, ii) infect cells through different receptors, iii) induce a diverse range of symptoms, iv) which are treated with specific and symptomatic therapies, and v) various proteins expressed by the viruses used as antigens for diagnosis and development of vaccines. The nature of the immune response to these viruses involves innate, cell mediated and humoral immunity, and several proteins of these viruses have been implicated in protective versus pathogenic responses. We have summarized and provided recent references for the current understanding of SARS-COV2 virus and immunological immune responses, and listed similarities and difference in characteristics to these four viruses. This systematic analysis of these viruses will enable the understanding the requirements and anticipate challenges in development of novel diagnostics, therapies, and vaccines for COVID-19 pandemic.Keywords
Vaccine; Disease; Symptoms; Prevention; Epidemiology
Introduction
Humans are infected by hundreds of viruses and bacteria. The COVID-19 pandemic has forced society to re-consider access of social health for everyone. In an extremely comprehensive summary, have reported that there are vaccines approved to prevent infections against 26 pathogens, and more than 240 in development [1]. Understanding the pathogenesis of these infectious agents has not only enabled development of measures for diagnosis, treatment, and prevention, but also an in-depth understanding of the immune system. Detailed studies of functional components of the immune system have revealed immunopathogenesis of diseases such as leprosy and tuberculosis that affect monocyte macrophages, HIV, which infects CD4+ T cells, Epstein Barr Virus, which infects B cells [2]. We have reviewed the current wave of emerging viruses, namely Dengue, Chikungunya, Nipah and Zika, which cause significant pathologies to provide lessons learned using a set of questions (Table 1). These questions address a comparative analysis of similarities and differences range of serotypes, geographical distribution, cells, and receptors. The similarities of the immune responses induced by these viruses to that induced by SARS-COV2 include induction of innate, cell-mediated, and humoral immune responses. The differences in responses by these related virus include i) SARS-COV2 induces cytokine storm, ii) antibodies to dengue have the potential to induce enhancement of infection, iii) chikungunya, dengue and zika have mosquitoes as intermediate hosts, iv) all the viruses have unique and different entry and fusion receptors. In this review, we have briefly described the key parameters of the virus and host cycle, the symptoms, epidemiology, and summarized the recent studies in progress for development of vaccines. Based on responses to these viruses, we have listed criteria for the requirements of a safe and effective vaccine for COVID-19.
| Contents | |
|---|---|
| What are the geographical areas which are affected by these viruses? | Table 2. |
| What is the variability of serotypes compared to COVID-19? | Table 3 |
| What animals are being affected by these diseases? | Table 4 |
| What the organs, cells and receptors and proteins of the virus for these viruses? | Table 5 |
| What are the approved and vaccines in development for these viruses? | Tables 6 A.B.C.D.E |
Table 1: Questions addressed in this review.
Methods
Dengue virus (DENV)
Endemic areas of DENV are underscored by near-equatorial geographies, tropic climates, and stagnant water, which enable mosquito breeding [3,4]. Aedes aegypti mosquitoes are the principal vectors for transmission of DENV reviewed in [5]. Mosquitoes usually breed in geographies below 6,500 feet, hence risks of dengue infections decrease with altitude. Severe dengue virus induced disease affects ~0.5% of individuals [3]. Several hundred million humans are infected every year (Table 2). There are four major strains of the virus, DENV1-4 (Table 3). Various cell surface receptors including glycated carbohydrates binding to the viral protein E and M, are involved in the binding and fusion of hepatocytes and other cells (Table 4) including dendritic cells, macrophages, heart and lungs. The animal species infected by DENV strains (Table 5). Upon infection of humans, there is a 4- to 10-day incubation period, which leads to symptoms that last 2-7 days. Prodomal stages of symptoms include high fever (104°F/40°C), chills, rash, erythematous mottling of the skin, facial flushing, retro-orbital headache, muscle and joint pain, nausea, lymphadenopathy, vomiting. The infection is confirmed by identification of viral NS-1 gene RNA, NS-1 protein antigen in serum, or presence of IgM and IgG antibodies [6]. Severity of disease progression is monitored by rising hematocrit ( ≥ 20%) and a falling platelet count (<100,000/mm3). Treatment for uncomplicated cases is bed rest, oral rehydration, and paracetamol as an antipyretic and analgesic. Treatment for patients with severe disease consists of immediate fluid therapy with colloids and extensive monitoring of any complications; blood transfusion is managed in extreme symptoms such as internal hemorrhage [6].
| Diseases | Worldwide numbers (infections per year) | Fatality Rate | Top geographies | References (WHO, CDC) |
|---|---|---|---|---|
| Dengue | ~ 390 million | <1% | Bangladesh, Malaysia, Philippines, Vietnam, India | [3], [42] |
| Chikungunya | ~ 100,000 | ~11% | Brazil, Caribbean, Sudan, Cambodia, Yemen, India | [8], [9] |
| Zika | ~30,000 | ~8% | Brazil,Africa,Asia, pacific | [19], [18] |
| Nipah | ~10,000 | ~40-75% | Australia, Bangladesh, Cambodia, China, India, Indonesia, Madagascar | [13], [12] |
| COVID-19 | >40 million | ~1% | Worldwide | [43], [44] |
Table 2: Geography and Epidemiology of the emerging viruses.
| Viruses | Major Serotypes infecting humans | Major Structural Genes | Antigen dependent enhancement |
|---|---|---|---|
| Dengue | DENV-1,2,3,4 | C/prM/E genes | Yes |
| Chikungunya | CHIK V | E1 and E2 genes | Low concentration |
| Zika | ZIK V | PrM,M, Envelope glycoprotein, Nucleocapsid |
Low concentration |
| Nipah | NiV | p(p,v,w,c) genes | Reported |
| Corornavirus | SARS-COV1, MERS-COV, SARS-COV2 | Spike, Membrane, Nucleocapsid | Reported |
Table 3: Variability of serotypes.
| CHIKV | DENV | ZIKV | NiV | COV | |
|---|---|---|---|---|---|
| Monkey | YES | YES | YES | YES | |
| Dog | YES | YES | YES | ||
| Cat | YES | YES | |||
| Horses | YES | YES | - | ||
| Sheep | YES | - | |||
| Mice | YES | YES | |||
| Rabbit | YES | ||||
| Hamsters | YES | ||||
| Marmosets | YES | ||||
| Tiger | YES | ||||
| Pigs | YES | ||||
| Flying foxes | YES | ||||
| Cow | YES | ||||
| Ducks | YES | ||||
| Goat | YES | ||||
| Bats | YES | YES |
Table 4: Different animal infected by emerging virus.
| Virus | Primary Receptor | Secondary Receptor | Cells | Organs affected | Proteins |
|---|---|---|---|---|---|
| DENV | Mannose binding receptor (MR) DC -SIGN |
Laminin binding protein Tubilin binding protein |
Dendritic cells Macrophages |
Liver, heart, Lungs |
nonstructural proteins: NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5 E and M proteins |
| CHIKV | Mxra8 Mxra8 | Fibroblasts and epithelial and endothelial cells |
Liver, joints muscle | Glycosylated E1 and E2, nonglycosylated nucleocapsid protein, capsid protein (C), two major envelope glycoproteins (E1, E2), (E3, 6K, and the transframe protein TF). | |
| NiV | Ephrin B2 Ephrin B3 |
Neuronal Cells | Brain | nucleoprotein (N), phosphoprotein (P), the interferon antagonists W and V, the viral C protein, a matrix protein (M), glycoproteins (F and G, respectively | |
| ZIKV | AXL, Tyro3, TIM1,TLR3,TLR8 | Endothelial cells, monocytes, skin keratinocytes, dentritic cells and NPCs. | Placenta | Capsid(C), membrane precursor (prM) , envelope protein(E) and seven non structural proteins (NS1, NS2A, NS3, NS4A, NS4B, NS5) | |
| COV2 | ACE2, CD147 | TMPRSS2 | Lung Epithelial cells | Lung, Hearts | Spike, M, E. NC protein |
Table 5: Cellular receptors, cells, organs, and Proteins of the viruses.
The study was submitted to the hospital’s ethics committee and approved. Since the study was retrospective and observational, no informed consent was required.
Chikungunya (CHIKV)
CHIKV is transmitted by Aedes aegypti and Aedes albopictus mosquitoes [7]. The virus infects mice, monkeys and pigs. The numbers of humans infected by this debilitating disease, which affects the joints, are listed from the WHO and CDC websites in Table 2 [8,9]. The acute phase of the infection results in an incubation period of 3–7 days, which results in symptoms such as fever, headache, rash, and debilitating polyarthralgia [10]. The chronic phase of disease can result in recurrent joint pain, which can last for years in some cases, is experienced by 30%–40% of those infected. .The primary receptor is Mxra8 Mxra8. CHIKV binds to the E2 domain B and overlaps with Mxra8 receptor binding site and affects organs like liver and joint muscles. The E1/ E2 proteins of virus also binds to glycosaminoglycans, DC-SIGN, TIM-1 and infects cells through clathrin-mediated fusion and entry. In humans, the virus replicates in the skin and disseminates systemically to the liver and joints. Viral loads of 1 x 108 particles/ mL in blood, and inflammatory cytokines such as type I interferons (IFNs) ranging from 0.5–2 ng/mL have been reported. The precise mechanism of CHIKV infection induced-severe musculoskeletal complication is not completely elucidated. Currently, there is no Chikungunya-virus specific anti-viral treatment; symptoms such as fever and joint pain are treated with anti-inflammatory and steroid drugs [9].
Nipah (NiV)
Human NiV was first identified Sungai Nipah (Nipah River village) in Malaysia [11]. Pteropus bats are reservoirs found in Malaysia and Bangladesh. There is evidence of Nipah infection among several species of domestic animals including dogs, cats, goats, sheep and horses. The virus enters its host through the oro-nasal route and causes infection. Several strains of NiV have been reported by the WHO and CDC from different geographies [12,13]. NiV proteins involved in binding, fusion and entry are listed in Table 4. Surface glycoproteins G and F have been demonstrated to bind and pH dependent fusion through cellular ephrin-B2 or ephrin-B3 receptors, while matrix (M) protein has been implicated in virus assembly and budding [14]. The cellular receptors for the virus are expressed on endothelium and smooth muscle cells in high levels in the brain, lungs, placenta and prostate, blood vessels in various other tissues [15], underscoring the involvement of these organs in the pathogenesis of this infectious disease. Symptoms include fever, headache, and myalgia, and followed altered mental status, alexia, hypotonia, segmental myoclonus, gaze palsy and limb weakness. Patients deteriorate rapidly and coma and death follow within a few days [12,13]. Ribavirin and monoclonal antibodies to G protein have been shown to be effective against NiV [16]. Severe conditions such as encephalopathy and other organ dysfunctions are treatment by addressing specific symptoms.
Zika virus (ZIKV).
First identified in 1947 [17], ZIKV was only known to cause sporadic mild disease in Africa and Asia. Nonhuman primates, horses, cows, carabaos (water buffaloes), goats, ducks, and bats have been reported to be infected by Zika virus. The transmission of the virus through the mosquito vector results in symptoms such as fever,rash,headache, joint pain, conjunctivitis, muscle pain. The 2007 outbreak in Yap Island, 2015 in French Polynesia, 2015 in Brazil, and 2017 in Rajasthan and Tamil Nadu, India, has brought about awareness of this virus as an emerging virus with significant threat to pandemic potential [18,19]. This flavivirus infects cells by binding of glycoprotein E through clathrin-mediated endocytosis and fusion through acidic pH-dependent entry into endosome, from which the genomic RNA escapes into the cytoplasm. The RNA expresses three proteins, membrane (M), Envelope (E) and Capsid (C), and seven non-structural proteins NS1, NS2a, NS2b, NS3, NS4A and NS5). The receptor for the virus implicated is TAM (Tyro3, Axl, Mer) receptor tyrosine kinase Axl, which is required for cellular entry [20]. The virus infects fetal neural progenitor and neural retinal cells, resulting in inflammation, reduced cellular proliferation, and apoptosis. Due to this mechanism of infection, ZIKV infections results in fetal abnormalities, such as blindness, dramatic loss of brain parenchyma, ventriculomegaly, and microcephaly. Diagnosis is confirmed my measuring viral RNA from serum, urine, and saliva. RT-PCR has been developed to detect live virus, viral proteins and ZIKV RNA, respectively. ZIKV RNA can be detected in serum, urine and saliva samples obtained at the acute phase of the infection using RT-PCR with more specificity, and have low sensitivity out comes. There are no specific treatments; symptoms are treated as required [21].
Concomitant QT interval prolonging agents during treatment were also noticed. Any premature discontinuation of the treatment regimen due to QT prolongation was extracted from medical records. HCQ was frequently associated with azithromycin, which also might lengthen the QT interval. Because of the high rate of association between these two drugs, azithromycin was analyzed separately from other concomitant QT prolonging drugs.
Five patients could not have their final QTc determined, three due to poor clinical evolution and inability to undergo an ECG or proper cardiac monitor registry, and two as a result of premature discharge. However, these patients were maintained within the report due to their clinical evolution and laboratory data as well as clinical outcomes.
Corona virus (SARS-COV2)
The World Health Organization announced that SARS-COV2 causes COVID-19 disease which has resulted in a world-wide pandemic on 11 March 2020 by the WHO [22]. ~40 million infected, and ~1.2 million deaths are documented to date (November 2020). As a comparator, influenza virus HINI, over hundred years ago, infected a third of the human population at that time and killed more than 50 million people. Severe Acute Respiratory Syndrome Coronavirus (SARS-COV) and Middle East Respiratory Syndrome Coronavirus (MERS-CoV) are from the same family; SARS-COV2 reported to be three times more infectious. A major difference in the viruses is the long incubation of asymptomatic infection by SAR- CoV2. COVID-19 has a relatively lower rate of fatality in healthy individuals, compared to elderly and patients with comorbidities [23] such as diabetes, cardiac disease, kidney disease.
SARS-Coronavirus 2 (SARS-COV-2) infects cells by binding of spike protein to the ACE2 receptor, proteolytic cleavage by membrane-associated proteolytic enzymes such as TMPRSS2, and fusion with the cell membrane [24]. The role of other proteins including membrane (M), Envelope (E), Nucleocapsid (N), remains to be clearly defined. The viral RNA enters the cells, and initiates replication to provide new viral particles, resulting in cytopathicity.
Infection with SARS-COV2 results in a dysregulated immune response, which is characteristic of the initial disease [25-27]. Greater than ten thousand reports have indicated that the immune response results in a cytokine storm, which leads to systemic pathogenesis of COVID-19. Multiple factors that contribute to the immunopathogenesis include i) health and comorbidities[28], ii) viral replication levels with leads to differential viral load[29], iii) activation of innate immune responses, iv) misfiring of IFNα, IFNβ levels during the first 4 days of infection, v) exhaustion of CD4 and CD8 T cells, vi) development of a limited antibody response, vii) which culminate to range of symptoms from asymptomatic, mild, moderate, severe and critical disease.
Vaccines
Vaccines for the viruses discussed above are in various stages of development. We have reviewed the vaccines and provided the information on the various trials for each pathogen in Tables 6a- 6e. The summary contains the vaccine platform, the immunogen, stage of development, and potential risks and adverse events. Based on the lessons learned from vaccines in development on various platforms for these emerging viruses, we have listed the criteria and potential adverse events that maybe anticipated with the ongoing clinical trials for COVID-19.
| Vaccine type | Vaccine name/Strategy | Sponsor | Clinical Trial Phase |
|---|---|---|---|
| Attenuated chimera | CYD, Denvaxia®:Yellow fever 17D vaccine virus backbone chimerized with prM and E proteins
TV003/TV005: Attenuated by deletion of 30 nucleotides from 3’ UTR of DENV-1, DENV-3 DENV-4, and a chimeric DENV-2/DENV-4 DENVax: Use attenuated DENV-2 PDK-53 as the backbone and replace with prM and E of other serotypes |
Sanofi-Pasteur
US NIH
US CDC/Inviragen/ Takeda |
Licensed, Post licensed evaluation is on-going Phase III Phase III |
| Inactivated virus | Purified formalin-inactivated virus (PIV) formulated with adjuvants | WRAIR/GSK | Phase I |
| DNA vaccine | Monovalent DENV-1 prME delivered by needle-free biojector | US NMRC | Phase I |
| Subunit vaccine | V180: 80% of N-terminal E protein produced in insect cell formulated with ISOCOMATRIX and alhydrogel |
Hawaii Biotech Inc. and Merck |
Phase I |
| Heterologous prime/boost |
TLAV-prime/PIV-boost and vice versa | US Army Medical Research and Materiel Command |
Phase I |
Table 6: DENV Vaccine table.
Dengue virus vaccines
Dengue vaccine candidates in clinical trials are shown in Table 6A. Dengvaxia vaccine (Sanofi Pasteur), approved in Mexico, Brazil, El Salvador, and Philippines, is a tetravalent dengue chimeric live- attenuated virus vaccine, based on replacement of structural genes of the licensed yellow fever vaccine 17D, with each DENV serotype [30]. Studies in macaques have demonstrated the immunodominance ranging from serotype 4 to least serotype 2 chimeric virus [31,32]. Clinical trials demonstrate the >88% subject seroconvert to all four DENV serotypes after receiving three doses of the vaccine. Thus, the tetravalent vaccine was safe and immunogenic in both dengue endemic and nonendemic areas. Phase IIb trial was conducted in 4–11-year-old school children at Ratchaburi Province, Thailand. The efficacy was highly variable between the various serotypes: 55.6% (95% CI −21.6 to 84.0) for DENV-1, 9.2% (95% CI −75.0 to 51.3) for DENV-2, 75.3% (95% CI −375.0 to 99.6) for DENV- 3, and 100% (95% CI 24.8 to 100.0) for DENV-4. Other vaccines for DENV currently in progress are listed in Table 6A. The WHO has a goal of reducing morbidity by 25% and mortality by 50% by 2020 [33]. While the vaccine trials are in progress, the major mode of prevention of DENV infection involve mosquito management in endemic areas, solid waste management, insecticide spraying, and personal clothing protection. Some of the social measures of personal protection apply to the current COVID-19 pandemic.
| Vaccine type | Strategy | Developer | Animal |
|---|---|---|---|
| Live-attenuated Virus |
DEN/DEN chimeric viruses: replacing the prM/E of recent clinical isolates with pr-M cleavage enhancing into the genetic background of attenuated DENV-2 Chin/Den: chimeric DENV based on the JE live vaccine strain SA 14-14-2 as a backbone |
Chiang Mai University, Mahidol University, NSTDA, BioNet Asia Beijing Institute of Microbiology and Epidemiology, the Chengdu Institute of Biological Products |
Rhesus macaques (Macaca mulatta) Rhesus macaques (Macaca mulatta) |
| Live-attenuated virus (Continued) |
Dengue with host range (HR) mutation: transmembrane domain I truncation to select the viruses that replicate only in insect cells KD382: attenuated by serial passages in non-natural host |
Arbovax
KAKETSUKEN and Mahidol University |
African Green monkey (genus Chlorocebus) Cynomolgus monkey |
| Inactivated virus | Purified psoralen-inactivated virus | US Naval Medical Research Center (NMRC) |
Aotus nancymaae |
| DNA vaccine | Tetravalent dengue prME: prM/E consensus sequence of each serotype delivered by electroporation |
ChulaVRC, Chiang Mai University, NSTDA |
ICR mice and NHPs (Macaca fasicularis) |
| Viral vector vaccine | VEE-Dengue VRPs: Infectious single cycle VEE expressing dengue antigens MV-DEN: A single live attenuated measles virus expressing EDIII of DEN1-DEN4 |
University of North Carolina at Chapel Hill (UNC) Themis Bioscience, the Institut Pasteur |
Rhesus macaque
Transgemic mice (susceptible to measles virus infection) |
| Virus like particles | DSV4: Chimeric VLPs using hepatitis B surface antigen to display envelope domain III of four DENV serotypes expressed in P. pastoris DENV-2 VLPs: express in mosquito cells |
NCR Biotech Science Cluster/International Centre for Genetic Engineering and Biotechnology, India and Emory University Chiang Mai University, Mahidol University, NSTDA, Thailand |
Immonogenicity: BALB/c mice and Rhesus macaqueChallenge model: AG129 mice BALB/c mice and NHPs (Macaca fascicularis) |
| Recombinant protein | Purified psoralen- inactivated virus |
US Naval Medical Research Center (NMRC) |
Aotus nancymaae |
Table 6A: Ongoing dengue vaccine candidates in preclinical phase.
| Vaccine | CHIKV strain | Challenges | Status |
|---|---|---|---|
| VRC-CHKVLP059-00-Virus-like-Particle | West African CHIKV strain 37997 | Multiple doses required; Adjuvant required for dose-reduction; Expensive manufacturing of in vitro VLP | Completed Phase 1 |
| CHIKV/IRESv2 | La Réunion | Safety concerns regarding reversion of mutation and recovering to wild type pathogenicity | Projected for Phase 1 |
| Measles Virus vector-CHIK’ Live attenuated Schwarz strain |
La Réunion | Pre-existing immunity to measles may impede or prevent immunogenicity; Phase 1: Adverse event rate 17% | Finished Phase 1 |
| TSI-GSD-218 | Clone 25/181; (SE Asian isolated strain AF15561) | Phase 2:Adverse events: 8% rate of arthralgia | Development stopped |
Table 6B: Vaccines for CHIKV.
| Vector | Antigen used | Dose of immunization | Animal model | Route of vaccination |
|---|---|---|---|---|
| Vesicular stomatitis virus (VSV) | rVSV expressing Niv G rVSV-ZEBOV-Gp-NivG Replicative defective VSV |
10^5 PFU(plaque forming unit) 10^7 PFU 10^6 infections particles | Hamsters African green monkey Female Syrian golden hamsters | Intraperitoneal Intramuscular Intramuscular |
| Canarypox virus (ALVAC) vaccine vector Adenovirus-associated virus(AAV) |
vCP2199, carrying the NIV-G and vCP2208, carrying niV F |
10^8 PFU 2.1010/1.1010 genome particles | Landrace female pigs Balb/c male mice | Intramuscular Intramuscular or intradermal |
| Vaccinia virus | NiV G and NiV F |
10^7 PFU | Balb/c female mice | Subcutaneously |
| Measles virus based vectors | NiV G | 1×10^5 TCID50 | African green monkeys | Subcutaneously |
| NewCastle disease(NDV) LaSota strains |
NiV G and NiV F |
108 EID50 2×109 EID50 | Mice Pig | Intramuscular Intramuscular |
| Nipah virus-like particles (NiV-VLPs) |
NiV G, F and M adjuvanted with Alum | 30mg VLP | Golden Syrian like hamsters | Intramuscular |
Table 6C: Vaccines in development for Nipah virus.
| Sponson | STATUS | TYPE OF VACCINE |
|---|---|---|
| Inovio | Phase I | DNA |
| Oxford University | Pre-clinical | Chimp-Adenovirus vector |
| Bio-Manguinhos, Valneva | Pre-clinical | Purified Inactivated virus |
| Protein Science | Pre-clinical | Recombinant Envelope protein |
| VBI-Vaccine | Pre-clinical | VLP containing envelope protein |
| Moderna | Pre-clinical | Lipid-nanoparticle delivered mRNA |
| Curevax | Pre-clinical | Thermostable mRNA |
| VaxArt | Pre-clinical | Recombinant oral vaccine |
| Hawaii Biotech | Pre-clinical | Allhydrogel based protein vaccine |
| Geovax | Pre-clinical | Live modified vaccinia Ankara |
| GSK | Pre-clinical | Live modified vaccinia Ankara |
| Sanofi | Pre-Clinical | Yellow-fever 17D |
| Semintis | Pre-clinical | Live pox virus |
| Themis Biosciences | Pre-clinical | Line Measles virus |
| Mayo Clinical Vaccine Group | Pre-clinical | Zika virus peptides in nanoparticles |
| Emergent Bio-solutions | Pre-clinical | Inactivated whole virus |
| Institute Pasteur, Shanghai | Pre-clinical | Recombinant subunit |
| Takeda | Preclinical | Inactivated whole virus (alum) |
Table 6D: ZIKV Table.
| Company | Vaccine | Dose | Phase I | Phase II | Phase III | Number | Efficacy Endpoint | Risks | |
|---|---|---|---|---|---|---|---|---|---|
| Chadox1 | Oxford + AZ + Serum | ChAdOx1 nCoV-19 | 2.5, 5 x 10e10 particles | NCT04324606 | NCT04400838 | NCT04400838 | 30000 | 50% | Pre-existing immunity |
| Ad5 | CanSino | 5E10vpAd5-nCov2 | 0.5, 1.0, 1.5 x 10e11 particles | NCT04566779 | Not listed | NCT04526990 | 40000 | Not listed | Readministration efficacy |
| China | systemic inflammation | ||||||||
| Ad5+Ad26 | Sputnik V | Sputnik V | 10e11 particles | Not listed | Not listed | Not listed | 40000 | Not listed | |
| Russia | |||||||||
| Ad26 | Janssen | Ad26.COV2.S | 5, 10, 25 ug | NCT04436276 | NCT04436276 | NCT04505722 | 60000 | 50% | |
| mRNA | Pfizer/ | BNT162b2 | 25, 100, 250 ug | NCT04368728 | NCT04368728 | NCT04368728 | 43998 | 60% | Frozen Formulation |
| BioINTECH | Integration | ||||||||
| mRNA | Moderna | mRNA-1273 | 25, 100, 250 ug | NCT04405076 | NCT04405076 | NCT044704 | 30000 | 60% | Stability |
| DNA | Inovio | INO-4800 | 1 & 2 mg | NCT04447781 | |||||
| Protein | Novovax/ Takeda | NVXCoV2373 | 5, 25 ug | NCT04368988 | 10000 | 67% | Ability to induce CTL activity | ||
| Inactivated | Sinovac | CoronaVac | NCT04383574 | NCT044704 | NCT04456595 | 9000 | Not listed | Lower Level of NAB | |
| China | Ability to induce CTL activity | ||||||||
| Manufacturing (Safety) |
Table 6E: SARS-COV2–Vaccines.
CHIKV vaccines
No vaccine is available currently to prevent infection from CHIKV [34]. Several platforms have been utilized to develop vaccines against CHIKV, such as inactivated viral vaccines, live-attenuated viruses, alphavirus chimeras, recombinant viral vaccines, consensusbased DNA vaccines, recombinant subunit vaccines and Virus- Like Particle (VLP). A live-attenuated CHIKV vaccine candidate, attenuated for replication in humans by passaging strain 15561 from a patient in Thailand in 1962, in MRC-5 cells (termed strain 181/clone25) was developed at the US Army Medical Research Institute of Infectious Diseases (USAMRIID). Phase I and II studies in healthy individuals demonstrated safety; the vaccine development has been discontinued. The vaccine involving E1- E2-E3-envelope containing DNA vaccine has been tested in mice and non-human primates. VLP-based vaccine expressing the CHIKV envelope proteins produced high-tittered neutralizing antibodies in monkeys after three doses and protected them against viremia after challenge. A recent phase I study at the NIAID have reported a vaccine for CHIKV to be safe and effective in healthy volunteers [35]. 400 subjects ages 18 to 60 in Puerto Rico, Haiti, the Dominican Republic, Martinique, and Guadalupe, developed immune responses for at least 16 months. Additional studies of prevention from CHIKV infections are in progress. All the vaccines against CHIKV are currently in development [34]. Prevention of CHIKV infection currently involved similar measures as DENV, i.e. controlling mosquitos, social hygiene, and personal protection.
NiV vaccines
At present, no vaccine against Nipah virus available [36]. Recent outbreaks from bats and pigs to humans in Malaysia, Singapore, Bangladesh and India [11] have underscored the requirement of a vaccine. The World Health Organization (WHO) therefore lists Nipah virus as a priority pathogen needing urgent action. Most vaccine approached for NiV target G glycoprotein(sG) of NiV through the Coalition for Epidemic Preparedness Innovations (CEPI) which is a collaborative effort between government and industry that enables conducting vaccine clinical trials. The platforms for NiV vaccines include recombinant DNA vaccines, virus-like particles, such as measles, rabies, VSV. ChAdO x 1 vector, a chimpanzee-adenovirus vector which has been tested in animal models. Prevention of Nipah virus infection involves personal protection and sequestering animal-human interactions.
ZIKV vaccines
There is no approved vaccine for prevention of ZIKV. Several platforms have been utilized to develop Zika vaccines. In this respect DNA plasmid encoding the E and PrM proteins, purified inactivated virus, DNA vaccines, virus like particles, live attenuated vaccine [37], mRNA vaccine and viral vector vaccines are in phase I and phase II trials. Some of these vaccines have been shown to activate antibody and T cell responses which result is reduced viral load and viral RNA in vivo studies. Table 6D provides a list of institutions and companies that are conducting clinical trials, and a detailed review is referenced [38]. Prevention of Zika virus infections involved mosquito control, personal protection and social hygiene.
SARS-COV2 vaccines
There are several vaccines being developed for COVID-19, which are listed in table 6E, and reviewed in [39]. Protein subunit vaccines (such as NVXCoV2373) can activate humoral immune responses; it remains to be seen if they can elicit activation of cytolytic T cell responses. Viral Vector vaccines in this respect ChAdO x 1 nCoV-19 [40] vaccine has shown an adequate safety profile and an enhanced antibody response. The trial has progressed to phase 3 for further evaluation in 30,000 individuals. Other adenovirus vaccines include Adenovirus 26 (Ad26-S.PP, and Ad-5) vectors are also in clinical trials. Nucleic acid vaccines comprise of mRNA and DNA vaccines are (mRMA-1273, and BNT162b2 mRNA vaccines and INO-4800 DNA vaccine) are being tested. These vaccines include formulation such as lipid nanoparticle-encapsulated, nucleoside-modified mRNA-encodes spike glycoprotein stabilized in its perfusion conformation. Whole inactivated vaccines (Coronovac) are currently in advanced clinical trials. Finally, live attenuated vaccines are weakened vaccine strains with limited capability of replication once administered in a host as vaccine. The live attenuated viruses are produced by adapting them to the unfavorable condition like low temperature or growing them in non-human cells. One of the major advantages of live attenuated vaccine is that they can be given intranasally via noninvasive delivery, which in turn induces mucosal immune response, necessary to prevent entry of the virus through upper respiratory tract. There are disadvantages of live attenuated vaccines including safety concerns and time consumption process of conventional development. Currently, Codagenix inc. is developing live attenuated viral vaccine using codon deoptimization process. Table 2 shows the comparisons of similarities and differences between these viruses.
Criteria for a Successful Vaccine
Based on the learnings from the emerging viruses, we have listed the parameters for success of COVID-19 vaccines:
i) Should stimulate antibody responses, of neutralizing antibodies in the titer range of ~2560, for greater than one year.
ii) Should stimulate a memory CD4 and CD8 T and B cells response.
iii) should have a large effect size in a population, that can enable herd immunity, e.g. >70%
iv) Should induce protection for children, older adults, and patients with comorbidities, all of whom may have sub-optimal immune responses.
v) Should be safe and not results in acute hypersensitivity reactions, e.g. in <0.1%.
vi) Should have a formulation that makes the vaccine stable in extreme temperature and distribution conditions.
vii) Should induce mucosal immunity, in the oral-respiratory tract.
Major Adverse Events that Could be Anticipated from a Sub-optimal Vaccine
Based on experiences with previous vaccines, we are providing the possible adverse events that could occur with a sub-optimal COVID-19 vaccine. The list below provides potential aspects about the vaccine.
i) Could elicit an acute hypersensitivity shock, due to the antigens or formulation.
ii) Could activate cross-reaction to self-proteins resulting in autoimmunity.
iii) Could induce local injection site reactions.
iv) Could results in activation of antibody dependent enhancement of SARS-COV2 [41] through interaction with Fc receptors.
v) Could induce activation of cells, that upregulate ACE-2 or TMPRSS2 receptors, which in turn may results in creating a new reservoir of highly-infectable cells [42] in vaccinated individuals.
vi) Could result in a weak immune response and not provide adequate levels of herd immunity [43], enabling spread of the virus in the community.
vii) Could exacerbate comorbidities [44] such as diabetes, heart disease etc.
Conclusion
In summary, the lessons learned from the pathogenesis of the emerging viruses include, i) viruses adapt to immune pressures very efficiently; ii) viruses utilize multi-step approaches to infect cells; iii) multiple viral proteins interact with multiple receptors on cells for entry, fusion, replication and assembly; iv) mutations occur more frequently under higher immune pressure; v) broadly acting neutralizing antibodies are induced through activation by several components of the immune system; vi) neutralizing antibodies alone may not be sufficient for a protective immunity; and vii) viruses can have different pathogenesis with every season.
REFERENCES
- Piot P, Larson HJ, O’Brien KL, N’kengasong J, Ng E, Sow S, et al. Immunization: vital progress, unfinished agenda. Nature. 2019;575(7781):119-129.
- Pulendran B, Davis MM. The science and medicine of human immunology. Science. 2020;369(6511).
- WHO. Dengue and Severe Dengue. 2020.
- Baak-Baak CM, Cigarroa-Toledo N, Pech-May A, Cruz-Escalona GA, Cetina-Trejo RC, Tzuc-Dzul JC, et al. Entomological and virological surveillance for dengue virus in churches in Merida, Mexico. Rev Inst Med Trop Sao Paulo. 2019;61.
- Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, et al. The global distribution and burden of dengue. Nature. 2013;496(7446):504-507.
- MedScape. Dengue Virus diagnosis and treatment. 2020.
- Powell JR, Gloria-Soria A, Kotsakiozi P. Recent history of Aedes aegypti: Vector genomics and epidemiology records. Bioscience. 2018;68(11):854-860.
- WHO. Chikungunya. 2020.
- CDC. Chickungunya. 2020.
- MedScape. Chikungunya Diagnosis and Treatment. 2020.
- Chatterjee P. Nipah virus outbreak in India. Lancet. 2018;391(10136):2200.
- CDC. Nipah virus. 2020.
- WHO. Nipah Virus. 2020.
- Bowden TA, Aricescu AR, Gilbert RJ, Grimes JM, Jones EY, Stuart DI. Structural basis of Nipah and Hendra virus attachment to their cell-surface receptor ephrin-B2. Nat Struct Mol Biol. 2008;15(6):567.
- Ang BSP, Lim TCC, Wang L. Nipah virus infection. J Clin Microbiol. 2018;56:e01875-01817.
- MedScape. Nipah Virus Diagnosis and Treatment. 2020.
- Bennet JE, Dolin R, Blaser M. Zika Virus. 2.
- CDC. Zika VIrus. 2020.
- WHO. Zika Virus disease. 2020.
- Nobrega GM, Samogim AP, Parise PL, Venceslau EM, Guida JP, Japecanga RR, et al. TAM and TIM receptors mRNA expression in Zika virus infected placentas. Placenta. 2020;101:204-207.
- MedScape. Zika Virus-Diagnosis and Treatment. 2020.
- Trojánek M, Grebenyuk V, Herrmannová K, Nečas T, Gregorová J, Kucbel M, et al. A novel coronavirus (SARS-CoV-2) and COVID-19. Cas Lek Cesk. 2020;159(2):55-66.
- Xie M, Chen Q. Insight into 2019 novel coronavirus: An updated in trim review and lessons from SARS-CoV and MERS-CoV. Int J Infect Dis. 2020;94:119-124.
- Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271-280.
- Azkur AK, Akdis M, Azkur D, Sokolowska M, van de Veen W, Brüggen MC, et al. Immune response to SARS‐CoV‐2 and mechanisms of immunopathological changes in COVID‐19. Allergy. 2020;75(7):1564-1581.
- Felsenstein S, Herbert JA, McNamara PS, Hedrich CM. COVID-19: immunology and treatment options. Clin Immunol. 2020;215:108448.
- Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. 2020;38(1):1-9.
- Zhou Z, Ren L, Zhang L, Zhong J, Xiao Y, Jia Z, et al. Heightened innate immune responses in the respiratory tract of COVID-19 patients. Cell Host & Microbe. 2020;27:883-890.
- To KK, Tsang OT, Leung WS, Tam AR, Wu TC, Lung DC, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20:565-574.
- Park J, Archuleta S, Oh ML, Shek LP, Jin J, Bonaparte M, et al. Immunogenicity and safety of a dengue vaccine given as a booster in Singapore: A randomized Phase II, placebo-controlled trial evaluating its effects 5–6 years after completion of the primary series. Hum Vaccin Immunother. 2020;16(3):523-529.
- Prompetchara E, Ketloy C, Thomas SJ, Ruxrungtham K. Dengue vaccine: Global development update. Asian Pac J Allergy Immunol. 2019;10:178-185.
- Redoni M, Yacoub S, Rivino L, Giacobbe DR, Luzzati R, Di Bella S. Dengue: Status of current and under‐development vaccines. Rev Med Virol. 2020;30:e2101.
- Dengue Vaccines, Immunization, Vaccines and Biologicals. 2020.
- Zhang L, Gao S, Song S. Recent progress in vaccine development against chikungunya virus. Front Microbiol. 2019;10:2881.
- Chen GL, Coates EE, Plummer SH, Carter CA, Berkowitz N, Conan-Cibotti M, et al. Effect of a Chikungunya Virus–Like Particle Vaccine on Safety and Tolerability Outcomes: A Randomized Clinical Trial. Jama. 2020;323(14):1369-1377.
- Amaya M, Broder CC. Vaccines to Emerging Viruses: Nipah and Hendra. Annu Rev Virol. 2020;7:447-473.
- NIAID - Zika Virus Vaccines. 2020.
- Mwaliko C, Nyaruaba R, Zhao L, Atoni E, Karungu S, Mwau M, et al. Zika virus pathogenesis and current therapeutic advances. Pathog Glob Health. 2020:1-9.
- Krammer F. SARS-CoV-2 vaccines in development. Nature. 2020;586(7830):516-527.
- Jackson LA, Anderson EJ, Rouphael NG, Roberts PC, Makhene M, Coler RN, et al. An mRNA vaccine against SARS-CoV-2—preliminary report. N Engl J Med. 2020;383(20):1920-1931.
- Iwasaki A, Yang Y. The potential danger of suboptimal antibody responses in COVID-19. Nat Rev Immunol. 2020:339-341.
- CDC. Dengue. 2020.
- WHO. Coronavirus. 2020.
- CDC. Coronavirus. 2020.
Citation: Noor S, Sambyal S, Ismail S, Chirmule N (2020) Comparative Analysis of Emerging Viruses to Inform Development of Safe and Effective Vaccines for COVID-19. J Vaccines Vaccin. 11: 440
Copyright: © 2020 Noor S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.