Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 4, Issue 1
Clinicopathological Profile of Primary Mediastinal Masses: Our Experience
Usha R Dalal, Ashwani K Dalal*, Akash Kartik, Virender Saini and Lakesh AnandReceived: 04-Jan-2020 Published: 03-Feb-2020, DOI: 10.35248/2684-1606.20.4.126
Abstract
Background: Primary mediastinal masses are uncommon lesions encountered in clinical practice and the source of origin of these masses can be an enigma for the clinicians. These masses can be neoplastic, congenital, or inflammatory in nature.
The data regarding their true incidence and the clinicopathological profile they present with is scarce due to their rarity. The clinical manifestations of these masses are usually nonspecific and protean. A standardized diagnostic workup is essential for their early detection and proper management. We retrospectively analyzed the clinicopathological profile of 29 cases of mediastinal masses diagnosed and operated in the department of General Surgery at a tertiary care hospital over a period of 11 years (2008-2019).
Aims and objectives: The study aims to assess the clinical profile of adult patients with primary mediastinal masses that presented to General Surgery department at Government Medical College and Hospital, Chandigarh (India).
Study design: This was a retrospective, descriptive and cross-sectional study of 11 years in which 29 patients of primary mediastinal masses with a definitive pathologic diagnosis after surgical resection were included. Detailed clinical profile, radiological and pathological findings along with their management outcome was noted.
Results: Maximum numbers of cases were symptomatic at presentation and presented with non-specific symptoms. Maximum numbers of cases were found to be in the 3rd decade of life. Anterior mediastinal masses are encountered more frequent as compared to middle and posterior compartments. Male to female ratio was almost equivalent and benign tumor predominated in this study. Diagnostic workup included thorough radiological assessment using Chest X-Ray and Contrast Enhanced CT scan (CECT). FNAC and/or biopsy were performed as and when required. Final histopathological analysis after surgical resection revealed 6 cases of thymoma, 6 cases of teratoma, 5 cases of neurofibroma, 3 cases of retrosternal goitre, 2 benign epithelial cyst, 2 schwannoma, 1 case each of bronchogenic cyst, ganglioneuroma and chylo-lymphatic cyst.
Conclusion: Majority of the patients of primary mediastinal masses present with non-specific chest pain and/or symptoms of compression at the time of their first visit to the hospital. Early detection is the key for prompt surgical intervention to reduce the overall morbidity associated with these masses.
Keywords
Mediastinal mass; Goitre; thymoma
Introduction
The mediastinum starts from thoracic inlet superiorly and up to the diaphragm inferiorly, bounded laterally by both the pleura. It is further divided into anterior, middle and posterior mediastinum to categorize the tumor and diseases of mediastinum according to their site and location [1]. A variety of tumor and cysts occur in the mediastinum and affect people of all ages. Primary mediastinal tumors are rare representing 3% of all tumors within the chest with an average incidence of 8 cases seen per year [2-4]. Neoplastic masses can be both benign and malignant in nature and can be primary or secondary in origin. The tissue of origin can be thymic, hematopoietic, lymphatic, germinal, neurogenic or mesenchymal. Patients may be asymptomatic altogether and the lesion may bediscovered incidentally on routine chest radiographs obtained for other reasons. Theymay present with vague chest complaints and or signs and symptoms due to compression and invasion of mediastinal structures.
We reviewed all cases of neoplastic primary mediastinal masses diagnosed over an 11 year period at a tertiary care institute in Northern India to analyse their clinical presentation, pathological profile and management outcome of these lesions.
Materials and Methods
Presented study is a retrospective study conducted at a tertiary care institute over a span of 11 years (2008-2019). In this study 29 patients with mediastinal masses who underwent surgical resection of the tumor at Government Medical College and Hospital Chandigarh(India), Department of General Surgery were included. All records of these patients were collected from the Medical Record Department of the hospital. All patients were inpatient and were treated in the past by the authors themselves. Results of all biochemical investigations and serological tests, preliminary chest radiographs, CECT scan, MRI of chest and histopathological examination were retrospectively evaluated according to age, sex, presenting symptoms, diagnostic procedures, anatomical location, surgical treatment, and histopathological diagnosis.
Primary mediastinal lesions including thymic tumor, germ cell tumor, neurogenic tumor, dermoid cysts, benign cysts, bronchogenic cysts were included in the study. Infective, inflammatory, vascular, lymphopoietic, primary lung and oesophageal pathologies and metastases from other sites were excluded from the study.
Results
A total of 29 adult patients with mediastinal masses were incorporated into the study. Of these 29 patients 15 (51.7%) were males and 14 (49.3%) were females. Age range was from 18 to 75 years of age with mean age of 33.6 years and median of 30 years. Most mediastinal masses were identified in the 3rd decade of life (Table 1). Benign pathologies dominated our study with 28 out of 29 being benign masses (96.5%), and only a single case turned out to be malignant (3.5%).
| Decade | No. of masses encountered |
|---|---|
| 2nd | 5 |
| 3rd | 12 |
| 4th | 6 |
| 5th | 3 |
| 6th | 1 |
| 7th | 1 |
| 8th | 1 |
Table 1: Prevalence of mediastinal masses according to the decade they presented.
17 masses (58.6%) were localised to anterior mediastinum and 9 (31%) were localised to posterior mediastinum. Only 3 cases (10.3%) were localised to the middle mediastinum (Tables 2 and 3). 4 patients (13.7%) were asymptomatic at the time of diagnosis. In 2 patients the lesion was detected incidentally on routine chest X-ray which was done preoperatively for surgery of fibroadenoma and carcinoma of right breast.
| S.no | Type of mass | Frequency | Total percentage |
|---|---|---|---|
| 1 | Thymoma | 6 | 40% |
| 2 | Teratoma | 6 | 40% |
| 3 | Retrosternal goitre | 3 | 20% |
Table 2: Anterior mediastinal masses-frequency.
| S.no | Type of mass | Frequency | Total percentage |
|---|---|---|---|
| 1 | Benign epithelial cyst | 2 | 66.60% |
| 2 | Bronchogenic cyst | 1 | 33.30% |
Table 3: Middle mediastinum masses-frequency.
4 patients (13.7%) were asymptomatic at the time of diagnosis. In 2 patients the lesion was detected incidentally on routine chest X-ray which was done preoperatively for surgery of fibroadenoma and carcinoma of right breast.
Non-specific symptoms such as vague chest pain (62%) and shortness of breath on exertion (41.3%) constituted the most commonly presenting chief complaints of the patients. Other complaints included cough, haemoptysis weakness, weight loss, headache, Horner ’ s syndrome, features of obstructive sleep apnoea etc. (Table 4).
| S.no | Type of mass | Frequency | Total percentage |
|---|---|---|---|
| 1 | Neurofibroma | 5 | 55.50% |
| 2 | Schwannoma | 2 | 22.20% |
| 3 | Ganglioneuroma | 1 | 11.10% |
| 4 | Chylolymphatic cyst | 1 | 11.10% |
Table 4: Posterior mediatinal masses-frequency.
Chest X-ray and CECT were done in all patients. Mediastinal widening was seen in all the cases on chest X-ray. MRI, FNAC, VATS, thyroid function tests, immunohistochemistry, and urinary catecholamine assay were done as and when required. Collective methods were used to make diagnosis before surgery and most cases were diagnosed using non-invasive methods. CECT was the most effective investigation in diagnosis and was able to delineate the origin and extent of the mass in most cases.
Out of 29 patients, 28 patients went for resection of the mass using various surgical procedures including VATS, Posterolateral thoracotomy, sternotomy etc. Resection was not feasible in thymic carcinoma due to vascularity of the lesion and invasion of adjacent structures. One patient who presented to emergency department due to blunt trauma to chest was found to have retrosternal goitre but patient did not undergo surgery and was lost to follow up.
The variety of tumors revealed by histopathological examination were; Mature teratomas, thymomas, neurofibroma, retrosternal goitre, schwannomas, thymic carcinoma, benign epithelial cyst, bronchogenic cyst, chylolymphatic cyst and ganglioneuroma in decreasing order of frequency (Table 5).
| Symptoms | Number of patients |
|---|---|
| Vague chest pain | 18 |
| Breathlessness | 12 |
| Cough | 6 |
| Asymptomatic/incidental | 4 |
| Haemoptysis | 2 |
| Generalized Weakness | 1 |
| Myasthenic symptoms | 1 |
| Weight loss | 1 |
| Epigastric pain | 1 |
| Headache | 1 |
| Horner syndrome | 1 |
| Weakness of limbs | 1 |
| Dysphagia | 1 |
| Obstructive sleep apnoea | 1 |
| Neck swelling | 1 |
Table 5: Symptoms and their frequency.
Intensive care unit (ICU) stay of patients ranged from 1 to 5 days, and was longest for patient with myasthenic symptoms. Total hospital stay ranged from 10 to 60 days. One patient with previous resection of schwannoma in upper mediastinum, presented with another tumour in the neck after 11 years which was excised and biopsy revealed it to be a scwannoma.
Patient of aggressive thymic carcinoma died on 4th postoperative day due to respiratory insufficiency. Crude death rate of the study was 3%.
Discussion
Due to a rare incidence, non-specific symptoms and a wide array of possible diagnoses mediastinal masses present to clinicians as a challenge. Mediastinal masses can be neoplastic, congenital, inflammatory, hematopoietic, metastatic or vascular in origin. Lymphomas are the most common mediastina masses [5]. In our study we retrospectively studied 29 patients that presented to the authors in a regular out-patient department setting over a span of 11 years. Only those patients that had a biopsy or FNAC proven tissue diagnoses pertaining to a primary mediastinal mass were included in the study.
Mediastinal mass can be asymptomatic or produce a wide range of non-specific symptoms, breathlessness and vague chest pain being most common. They can also present as surgical emergencies like superior vena caval obstruction and stridor [6]. One of our patients also presented with Horner’s syndrome, in addition to the compression symptoms.
Our study was in line with other studies where anterior mediastinal masses (teratoma and thymomas most commonly) were more common than middle and posterior mediastinal masses [5]. In posterior mediastinal masses neurogenic tumor predominated as in accordance to other studies but our study had more cases of neurofibroma as compared to other studies where schwannomas were found to be more frequent [7-9].
Chest X-ray showed evidence of mediastinal mass/widening in all cases. CECT turned out to be the most useful and effective investigations to reach a diagnosis. This is in accordance to various studies that have been published in peer reviewed journals where CECT has an upper hand in distinguishing mediastinal masses in comparison to X-rays, ultrasonography and MRI [10,11].
USG or CT guided FNAC/ FNA biopsy was done in all cases and histopathological examination of the specimen after surgery confirmed the final diagnosis. Immunohistochemistry studies were done whenever indicated to confirm the diagnosis [12].Some studies have reported the use of invasive procedures like thoracotomy, anterior mediastinotomy to make diagnosis [5-13].
When comparing the benign vs. malignant nature, our study showed the predominance of benign masses (96.5%) much more than malignant (3.5%), as is shown in studies by Dasgupta and Adegboye [14,15]. Most studies that showed the predominance of malignant masses included lymphopoeitic malignancies (lymphomas) as part of the study [14-16].
Here we describe some of the peculiar cases that were encountered in the study which might help clinicians diagnose and manage similar cases in their practice.
Thymomas
In anterior mediastinal masses thymomas and teratomas dominated our study each with 40% frequency. Out of 6 cases of Thymoma 5 turned out to be benign and 1 turned out to be a case of aggressive malignant thymic carcinoma. Of all thymic masses in our study only 1 presented with myasthenic symptoms and rest presented with vague chest pain and breathlessness which is different from a lot of studies that suggest that myasthenia gravis occurs in approximately 30 to 50% of patients with thymoma [17]. Though some authors suggest that serum acetylcholine receptor antibodies should be checked in all patients of thymomas. Before resecting them, however, the management protocol does not change based upon the result and medical management is required only when active symptoms are present [17]. Largest tumor size that was seen was 15*15 cm, the pre-op FNAC was inconclusive and post operatively histological examination of excised specimen revealed thymoma (Figure 1). Post operatively patient developed aplastic anemia for unknown reasons and is currently undergoing treatment for the same. Three cases presented with unusual unassociated diseases in our study. Patient with myasthenic symptoms had poliomyelitis, one patient developed red cell aplasia postoperatively, one patient was diagnosed when undergoing evaluation for pemphigus and other was diagnosed on routine Chest X-ray before excision of fibroadenoma of breast (Figure 2).
Figure 1. CT showing Schwanomma.
Figure 2. CT showing thymoma.
Patient of invasive thymoma was a 20-year old male presented with severe respiratory distress due to compression. On exploration, the tumor was highly vascular and was encircling the great vessels with invasion of other neighboring structures. Only biopsy of the mass could be taken which revealed it to be a case of aggressive thymic carcinoma. The patient died in intensive care unit on post-op day 5 due to respiratory insufficiency.
Neurogenic tumor
Neurogenic tumors are the most common posterior mediastinal masses [8]. They can arise from peripheral nerves, sympathetic ganglia or parasympathetic ganglia [18]. In our study there were 5 cases of neurofibroma, 2 cases of schwannoma and 1 case of ganglioneuroma. The neurogenic tumors in our study originated from one or more of the intercostal nerves.
Largest tumor that was seen was of ancient schwannoma measuring 20*15 cm and on CECT it extended from arch of aorta to the base of skull displacing the carotid sheath anteriorly, and compressing the major vessels and completely occluding them. Tumor was occupying the upper 1/3rd of left hemi-thorax displacing the trachea to the right side (Figure 3). This patient presented with large lump in the neck, breathlessness, chest pain and Horner’s syndrome. 8 years later the patient was reoperated for another 6*8 cm schwannoma anterior to C2-C4 vertebra which was displacing the esophagus and trachea anteriorly.
Figure 3. CT showing thymoma.
One patient presented to our department with chest pain and shortness of breath after she has been operated by a neurosurgeon for a neurofibroma with intraspinal extension 1 year back. Chest X-Ray showed mediastinal widening and CECT showed tumor in the posterior mediastinum reaching upto the thoracic vertebra without any intraspinal extension on the MRI. The tumor was excised via posterolateral thoracotomy and a separate incision on the back.
Though it has been suggested that all patients with a confirmed diagnosis of a neurogenic tumor should undergo MRI to exclude intraspinal extension of the tumor we suggest that CECT can delineate enough information to know whether an MRI is required or not and hence the decision can be made on a case by case basis [8-18].
Ganglioneuroma-20 year old male with poliomyelitis presented with left side chest and epigastric pain. USG and CECT revealed diffuse mass in the paraspinal region of the left hemithorax starting from T4 and extending upto T12 below the diaphragm through the aortic hiatus without any effect on the aorta itself. Multiple masses originating from multiple intercostal nerves (T4-T12) extending into the abdomen were seen during the surgery that was done through left abdominothoracic approach and the mass was resected. Urinary catecholamine studies including urinary vanillylmandelic acid (VMA) testing were done prior to surgery to differentiate from pheochromocytomas.
Retrosternal goitre
In this study, 3 cases were of retrosternal goitre. Out of these three cases 1 case that was diagnosed when being evaluated for blunt chest trauma did not give consent for the surgery. One case presented with respiratory symptoms and due to tracheal compression by the retrosternal goitre and an evident neck swelling. In the 3rd case a 45 year old obese female with short neck, who was earlier being treated for obstructed sleep apnoea by the chest physicians for a year and a half suddenly develops respiratory distress in the midnight. Chest X-ray was done and it revealed tracheal deviation and compression with mediastinal widening at the thoracic inlet (Figure 4). CECT scan suggested enlarged thyroid with intrathoracic extension upto the level of the carina. Flexible bronchoscopy showed tracheal comression anteroposteriorly (Figure 5).Clinically thyroid enlargement could not be appreciated due to short neck and obesity. After stabilization, FNAC was done and it suggested retrosternal goitre for which total thyroidectomy was done. After surgery she was discharged on thyroxine replacement and she complains of obstructed sleep apnoea resolved [19].
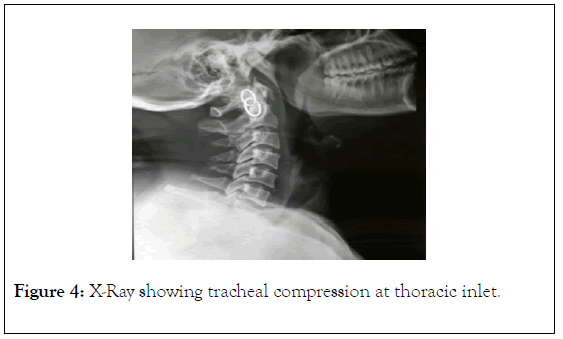
Figure 4. X-Ray showing tracheal compression at thoracic inlet.
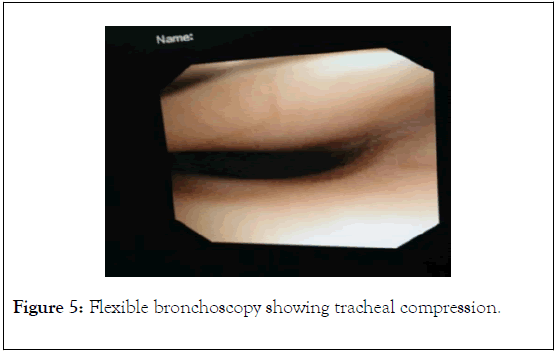
Figure 5. Flexible bronchoscopy showing tracheal compression.
Teratomas
Teratomas are germ cell tumors and can present anywhere in the midline. Though germ cell tumors are uncommon in the mediastinum, 75% of germ cell tumors originating in the mediastinum are teratomas [17-21]. Most of the teratomas are mature teratomas that are well differentiated and benign in nature. Teratomas can arise both in children and adults. When large enough teratomas may rupture and present with drastic mediastinal symptoms [17]. We encountered 6 cases of teratomas, all of them were mature, benign masses and all were diagnosed with CECT except in the case of a 20 year old female where due to diagnostic dilemma of massive hydrothorax ICD was put in to relieve the respiratory distress by the chest physicians but without any relief. Patient was explored using right PLT and diagnosis of giant teratoma of mediastinum was made during surgery, filling whole of the right hemithorax. Management of a symptomatic teratoma includes surgical excision as most cases do not have recurrence when excised completely. Teratomas can calcify and become adherent to nearby structures. In one of our cases the wall of giant teratoma was calcified and a part of the wall was adherent to the pericardium (Figure 6).
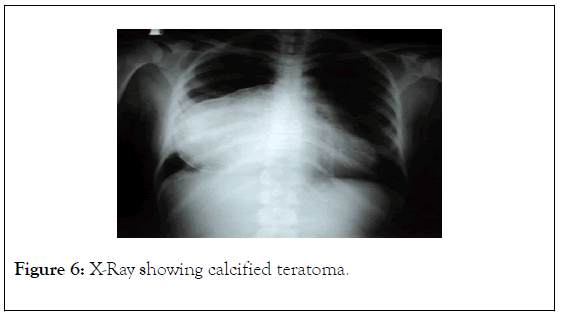
Figure 6. X-Ray showing calcified teratoma.
Chylo-lymphatic cyst
A 22 year old male patient with progressive symptoms of orthopnoea came to surgical OPD after he was referred from a community health centre. When investigated, CECT scan suggested cystic lesion in the upper posterior mediastinum of about 10*6 cm from the arch of aorta to the thoracic inlet shifting the trachea to the right side. FNAC revealed milky fluid. Exploration was done using the lower cervical approach and the cyst was excised. On the 3rd post-operative day Romovac started draining chyle in the drain, which was initially managed conservatively however due to persistently increasing amount of the draining fluid ligation of thoracic duct by VATS was done and patient was discharged after 5 days without any complications and was in regular follow up with no residual complains.
Conclusion
Mediastinal masses are rare and can present as a challenge for clinicians due to protean manifestations. Clinicians need to be vigilant as a lot of times diagnosis can be delayed and patients can land up with features of respiratory distress due to compression of trachea or carina as seen with some of our cases. Anterior mediastinal masses are most common followed by posterior mediastinum which mostly comprises of neurogenic tumors. Middle mediastinal masses are very rare and are generally benign cysts. Surgical resection of the mass is required in most of the cases. Most of the time diagnostic clues can be picked up on routine Chest X-ray. CECT scan reveals the exact extent of the mass and USG or CT guided FNAC can help in making the tissue diagnosis. Other investigations are usually adjuvant and should only be done when other investigations fail or when extra information is required based upon above investigations. Though excision by thoracotomy is the operative management chosen for most of the cases, use of VATS should be done whenever feasible as it leads to less postoperative pain, faster recovery, short hospital stay, better cosmetic results and overall patient satisfaction rate.
REFERENCES
- Fraser RS, Pare JAP, Fraser RG. Synopsis of Diseases of the Chest. Philadelphia: WB Saunders; 1994.
- Shields TW, Locicero J, Ponn RB, Rusch VW. General Thoracic Surgery (6th edn) Philadelphia: Wolters Kluwer | Lippincott Williams & Wilkins.
- Rubush JL, Gardner IR, Boyd WC, Ehrenhaft JL. Mediastinal tumors: Review of 186 cases. J Thorac Cardiovasc Surg. 1973; 65: 216-222.
- Wongsangiem M, Tangthangtham A. Primary tumors of the mediastinum: 190 cases analysis. J Med Assoc Thai. 1996; 79: 689-697.
- Vaziri M, Pazooki A, Zahedi-Shoolami L. Mediastinal masses: Review of 105 Cases. Acta Medica Iranica. 2009; 47(4): 297-300.
- Dubashi B, Cyriac S, Tenali SG. Clinicopathological analysis and outcome of primary mediastinal malignancies: A report of 91 cases from a single institute. Ann thorac Med. 2009; 4(3): 140-142.
- Kapoor A, Singhal MK, Narayan S, Beniwal S, Kumar HS. Mediastinal Schwannoma: A clinical, pathologic, and imaging review. South Asian J Cancer. 2015; 4(2): 104-105.
- Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: Part 2. Tumors of the middle and posterior mediastinum. Chest. 1997; 112: 1344-1357.
- Feryal G, Basak E, Aysegul U, Rejin K, Tansu S, Alaaddin C. Mediastinal Masses In Children: Experience With 120 Cases. Pediatric Hematology and Oncology. 2012; 29: 141-147.
- Tomiyama N, Honda O, Tsubamoto M, Inoue A, Sumikawa H, Kuriyama K, et al. Anterior mediastinal tumors: Diagnostic accuracy of CT and MRI. European Journal of Radiology. 2009; 69: 280-288.
- Juanpere S, Cañete N, Ortuño P, Martínez S, Sanchez G, Bernado L. A diagnostic approach to the mediastinal masses. Insights Imaging. 2013 ; 4(1): 29-52.
- Ruediger H, Lars K, Helmuth G, Konrad S, Winfried P. The value of a noninvasive diagnostic approach to mediastinal masses. Ann Thorac Surg. 2003; 75: 1086-1090.
- Devi GHJ, Das JK, Pasha MM, Prathima KM. Retrospective analysis of mediastinal lesions: A tertiary care center experience. SSRG International Journal of Medical Science. 2015; 2(9).
- Dasgupta S, Bose D, Bhattacharyya NK, Saha M, Biswas K, Biswas PK. A clinicopathological study of mediastinal masss operated in a tertiary care hospital in Eastern India in 3 years with special reference to thymoma. India J Pathol Microbiol. 2016; 59(1): 20-24.
- Adegboye VO, Ogunseyinde AO, Obajimi MO, Ogunbiyi O, Brimmo AI, Adebo OA. Presentation of primary mediastinal masses in Ibadan. East African Medical Journal. 2003; 80: 484-487.
- Aroor AR, Rama PS, Seshadri S, Teerthanath S, Uppoor R. A Study of Clinical Characteristics of Mediastinal Mass. 2014 Feb; 8(2): 77-80.
- Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: Part 1. Tumors of the anterior mediastinum. Chest. 1997; 112: 511-522.
- Reed JC, Hallet KK, Feigin DS. Neural tumors of the Thorax: Subject Review from the AFIP. Radiology. 1978; 1(126): 9-17.
- Dalal AK, Dalal UR, Wani AJ. Retrosternal goitre masquerading as obstructive sleep apnoea in a middle-aged female. J Evid Based Med Healthc. 2017; 4(78): 4639-4642.
- Peterson CM, Buckley C, Holley S, Menias CO. Teratomas: A Multimodality Review. Curr Probl Diagn Radiol. 2012; 41: 210-219.
- Temes R, Chavez T, Mapel D. Primary mediastinal malignancies: Findings in 219 patients. West J Med. 1999; 170: 161-166.
Citation: Dalal RU, Dalal KA, Katrik A, Saini V, Anand L (2020) Clinicopathological Profile of Primary Mediastinal Masses: Our Experience. J Surg Anesth. 10.35248/2684-1606.19.3.126
Copyright: �?â??�?�© 2020 Dalal RU, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.