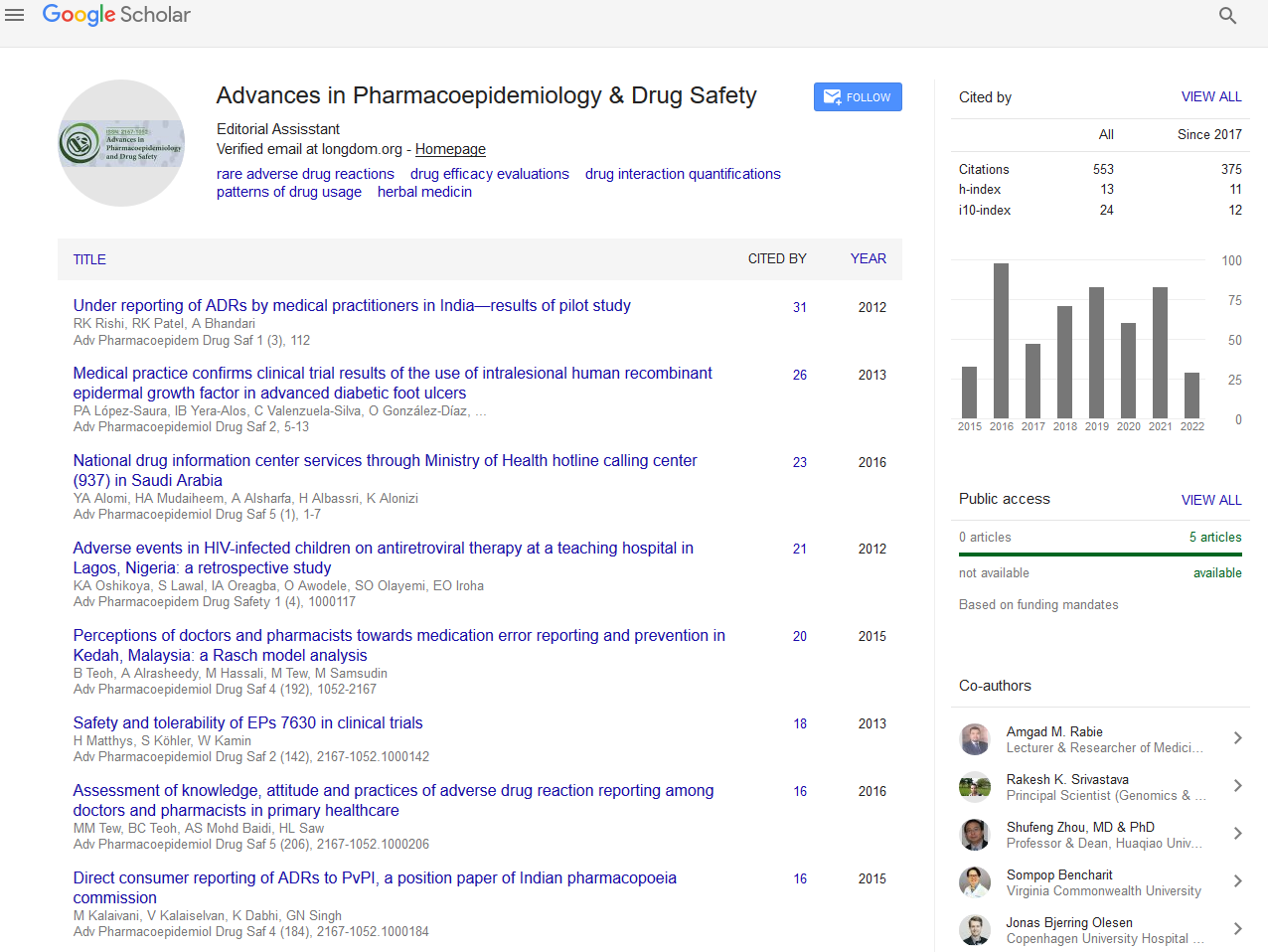
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- SWB online catalog
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research - (2020) Volume 9, Issue 2
Challenges of Hepatotoxicity Associated with Isoniazid Preventive Therapy among People Living with HIV in Eritrea
Mulugeta Russom1*, Araia Berhane2, Merhawi Debesai1, Hagos Andom3, Dawit Tesfai4, Zenawi Zeremariam2, Selamawit Gebrehiwet1, Nighisty Tesfamichael2, Saleh Mohammed Said5 and Hagos Ahmed62Communicable Disease Control Division, Ministry of Health, Asmara, Eritrea
3Ministry of Health Maekel Branch, Asmara, Eritrea
4School of Pharmacy, Asmara College of Health Science, Asmara, Eritrea
5HIV Clinic, Hahaz Hospital, Ministry of Health, Asmara, Eritrea
6National Statistics Office, Ministry of National Development, Asmara, Eritrea
Received: 20-Mar-2019 Published: 05-Jul-2019, DOI: 10.35248/2167-1052.20.9.228
Abstract
Background
Isoniazid preventive therapy (IPT) is an intervention recommended by the WHO for prophylaxis of Tuberculosis (TB) in people living with HIV (PLWH) and reported as generally safe with little risk of hepatotoxicity. Following its introduction in Eritrea in 2014, IPT related hepatotoxicity and fatality have been frequently reported to the Eritrean Pharmacovigilance Centre. The aim of this study is, therefore, to quantify the risk of hepatotoxicity, evaluate the effectiveness of close laboratory monitoring, assess the causal relationship of IPT and hepatotoxicity, identify possible risk factors and assess preventability of Isoniazid-induced hepatotoxicity in PLWH.
Methods
This was an observational cohort study of PLWH on IPT enrolled from three Antiretroviral therapy (ART) Clinics in Asmara, Eritrea, between August 2016 and February 2017. Causality and preventability of the cases was assessed using Naranjo probability scale and P-method respectively.
Results
Of the 360 eligible patients, 56 were identified with hepatotoxicity with an incidence rate of cases per 1000 person-months with a median time to reaction onset of 34 days. About 41% of the cases developed severe or very severe hepatotoxicity following initiation of IPT. INH was terminated in 78.6% of the cases and reaction abated in 84.1% (37/44) following withdrawal of INH. Besides, ART was discontinued in 42.5% of the cases due to hepatotoxicity. In majority of the cases (87.5%), the causal relationship was found to be ‘probable’ and in 82.1% hepatotoxicity was not preventable.
Conclusion
The incidence rate of INH-related hepatotoxicity is very high with a short time to reaction onset and the occurrence of severe/ very severe hepatotoxicity was unavoidable in substantial number of patients; making risk minimization plan and IPT deployment challenging.
Keywords
Patients on HAART; Isoniazid preventive therapy; Hepatotoxicity; Eritreadose; High dose
Introduction
Isoniazid Preventive Therapy (IPT) is an important intervention for preventing and reducing tuberculosis (TB) in people living with HIV in countries having higher risk of TB [1,2]. By providing Isoniazid 300 mg tablet on daily basis for six months, People Living with HIV (PLWH) are expected to be protected from TB for several months to years [1,3]. Several studies reported that the concurrent use of antiretroviral therapy (ART) and IPT pose little risk of hepatotoxicity (0.07-1.9%) where more events occur with concurrent use of Nevirapine than Efavirenz based ART regimen [4-7]. A recently conducted multi-country open-label randomized controlled clinical trial however reported a higher incidence (7.3%) of IPT related hepatotoxicity [8]. IPT has also been associated with small risk of fatal hepatotoxicity that ranges from 0.003% to 0.06% [9-11]. The possible mechanism by which Isoniazid causes hepatotoxicity has been controversial. Most recent studies, however, suggest that it is through bio-activation of INH itself which results a reactive metabolite that ultimately form covalent adducts to liver macromolecules [12-16]. Covalent binding of the active metabolite is more likely to lead to an immune response.
Considering the low risks of Isoniazid (INH) induced hepatotoxicity, countries have been recommended by the WHO to use IPT without routine laboratory monitoring of liver function [17,18]. However, following the introduction of IPT for PLWH in Eritrea in 2014, IPT associated hepatotoxicity and fatality have been frequently reported between 2014 and 2016 [19]. The investigation report shows that many of the cases were stable under Highly Active Antiretroviral Therapy (HAART) for several years without derangement of their liver enzymes prior to initiation of IPT.
In our previous publication [19], it was concluded that hepatotoxicity associated with IPT is serious and possibly more frequent than expected. It was also hypothesized that the life-threatening or fatal outcomes of the hepatotoxicity could be prevented by appropriate laboratory monitoring and/or dose-reduction for the underweight patients. The aim of this seven-month study is therefore to estimate the incidence of hepatotoxicity, assess the effectiveness of close laboratory monitoring in minimizing IPT related serious hepatotoxicity, assess the causal relationship of IPT and hepatotoxicity, identify possible risk factors and assess the preventability of INH-induced hepatotoxicity in PLWH.
Methods
Study design and setting
A seven-month prospective, longitudinal and observational cohort study was carried out on HIV patients taking IPT in three hospital ART clinics in Asmara between August 2016 and February 2017. Three hospitals with ART clinics in the Central region, two public and one private, were randomly selected and included in the study. The selected study sites were Orotta national referral and teaching hospital, Hazhaz hospital and Sembel hospital. The selected study sites provide services to about 37% of HIV patients taking HAART in the country [unpublished CDC data]. Patients on IPT were followed monthly until completion of the study.
Study population
Study participants came from different parts of the country; thus, the source population was not specific. All HIV infected patients on HAART eligible for IPT were enrolled into the study. Participants who had no active liver diseases (hepatitis C and B infection) and no history of regular alcohol intake were eligible for the study. Besides, those who stayed on IPT for less than two months before commencement of the study and had normal baseline liver function test (LFT) were enrolled.
Study instruments and data collection approach
Data collection tools were adopted from previous study instruments developed by the Eritrean Pharmacovigilance Centre. The study tools were improved with inputs of selected experts from hospitals, the National Regulatory Authority, Asmara College of Health Sciences, the WHO, the Uppsala Monitoring Centre and other members of international universities including the Erasmus University Medical Center of the Netherlands. Two data collection tools were used for this study; a listing form and structured questionnaire. The listing form was aimed at capturing the background information of all the study population (age, sex, body weight, cumulative drug exposure, alcohol intake, number of drugs taken, and type of ART regimen, comorbidities and latest CD4 count). Whereas the structured questionnaire was designed to document reaction (hepatotoxicity) and drugs detail as well as baseline and/or follow-up test results including LFT, hepatitis B and C serology and CD4 cell count. For all enrolled patients, venous blood samples were taken on monthly basis (if not possible, every other month) to monitor liver function. Moreover, patients were encouraged to report any signs and symptoms of hepatotoxicity at the earliest. Causality and preventability assessment were performed using Naranjo probability scale [20] and P-method [21] respectively
Exposure and outcome definition
In this study, patients were exposed to a life-long treatment of first-line HAART (64.4% on Zidovidine+Lamuvidine+Nevirapine, 33.9% on Atripla and 1.7% were taking other regimens including the second-line) and some patients were taking co-trimoxazole 960 mg on daily basis in addition to HAART. Moreover, all patients were exposed to Isoniazid 300 mg and Vitamin B6 once daily for six months.
The study end point was hepatotoxicity following use of IPT and its severity was assessed based on the US-FDA drug-induced liver toxicity grading scale [22] as follows:
• Mild hepatotoxicity is defined as aspartate aminotransferase (AST) or alanine aminotransferase (ALT) elevations of 1.1-2.5 times the upper limit normal (ULN) (<121 IU/L).
• Moderate hepatotoxicity is defined as elevation of AST or ALT of 2.6-5.0 times the ULN (121-200 IU/L).
• Severe hepatotoxicity is the elevation of AST or ALT of 5.1-10 times of the ULN.
• Very severe (potentially life threatening) can be defined as the elevation of AST or ALT >10 times ULN.
Statistical analysis
CSPro version 6.3 and SPSS version 20 were used to enter and analyze data respectively. Descriptive statistics was performed to calculate incidence, time to onset of the hepatotoxicity, median age and body weight of the cases. To assess associations of risk factors for the hepatotoxicity, the variables of interest were subjected to logistics regression model and results were presented with adjusted odds ratio accompanied by p-value and 95% confidence interval to test the level of significance. Associations with p-value less than 0.05 were considered as statistically significant.
Ethical considerations
Ethical clearance was obtained from the Health Research Ethics and Protocol Review Committee of the Ministry of Health. In addition, all ethical and professional considerations were followed during the study to make patients’ identity strictly confidential. Informed consent was also obtained from each study participant prior to enrolment.
Results
Between August 2016 and February 2017, 360 HIV patients on IPT were followed with mean observation time of 4.4 months. Of these, 69.7% were females with median age of 39 and 46 for males (Table 1). All but three patients were not consuming alcohol while they were on IPT and nine patients had other comorbidities. Detailed background characteristic of the study population is depicted in Table 1.
Table 1: Distribution of the HIV patients on IPT by background characteristics.
| Background Characteristics | Number | % | |
|---|---|---|---|
| Hospital | Orotta national referral Hospital | 286 | 79.4 |
| Sembel Hospital | 32 | 8.9 | |
| Hazhaz Hospital | 42 | 11.7 | |
| Age group | 15-34 | 82 | 22.8 |
| 35-44 | 157 | 43.6 | |
| 45-54 | 89 | 24.7 | |
| 55 and above | 32 | 8.9 | |
| Sex | Male | 109 | 30.3 |
| Female | 251 | 69.7 | |
| Any Comorbidity | Yes | 9 | 2.5 |
| No | 351 | 97.5 | |
| Treatment status | ART+INH | 360 | 100 |
| INH alone | 0 | 0 | |
| ART status | Nevirapine based | 232 | 64.4 |
| Efavirenz based | 122 | 33.9 | |
| Others | 6 | 1.7 | |
| Total number of drugs taken | 5 | 274 | 76.1 |
| 6 | 70 | 19.4 | |
| 7 | 12 | 3.3 | |
| 8 | 3 | 0.8 | |
| 9 | 1 | 0.3 | |
| CD4 count | Below 200 | 43 | 11.9 |
| 200-349 | 69 | 19.2 | |
| 350 and above | 246 | 68.3 | |
| Not Reported | 2 | 0.6 | |
| Total | 360 | 100 | |
During the study period, 15.6% (56/360) of the study participants were identified with hepatotoxicity with a median time-to-reaction onset of 34 days. To exactly quantify the risk, incidence rate was found to be 37 cases per 1000-person months. This indicates that if 1000 patients be exposed to IPT for a month, we would get 37 cases of hepatotoxicity. According to US-FDA drug induced liver toxicity grading scale [22], about 41% the cases developed severe or very severe hepatotoxicity following the initiation of IPT though there was monthly laboratory monitoring in 78.5% (Table 2).
Table 2: Severity of the hepatotoxicity cases according to the US-FDA drug induced liver toxicity grading scale.
| S. No. | Severity | Count |
|---|---|---|
| 1 | Mild | 13 |
| 2 | Moderate | 20 |
| 3 | Severe or very severe | 23 |
| Total | 56 |
US-FDA: United States Food and Drug Administration
Acute hepatotoxicity (severe and very severe) was developed within a month in seven cases and in the second month in eight cases (Table 3).
Table 3: ALT (IU/L) results of selected cases developed severe or very severe hepatotoxicity within the first or second month following use of IPT.
| Case number | Baseline | First Month | Second Month |
|---|---|---|---|
| 1 | 24 | 532 | |
| 2 | 28 | 216 | 1056 |
| 3 | 10 | 1016 | |
| 4 | 23 | 579 | |
| 5 | 14 | 198 | 1260 |
| 6 | 27 | 60 | 509 |
| 7 | 48 | _ | 1561 |
| 8 | 28 | 300 | 400 |
| 9 | 40 | 1050 | 1385 |
| 10 | 27 | 1215 | |
| 11 | 18 | 51 | 389 |
| 12 | 12 | 110 | 322 |
| 13 | 24 | 512 | |
| 14 | 41 | 82 | 453 |
| 15 | 24 | 67 | 693 |
ALT: Alanine aminotransferase; IU: International Unit; L: Liter; IPT: Isoniazid Preventive Therapy
To manage hepatotoxicity, INH was withdrawn in 78.6% of the cases. Of those, reaction abated in 84.1% (37/44) following withdrawal of INH and persisted in one case. In majority of the cases (87.5%), the causal relationship using Naranjo probability scale was found to be ‘probable’ and in 82.1% hepatotoxicity was not preventable (Table 4). Besides, HAART was discontinued and switched to other regimen in 42.5% of the cases due to hepatotoxicity.
Table 4: Summary of causality and preventability assessments.
| Assessment | Category | % of cases |
|---|---|---|
| Causality | Probable | 78.6 |
| Possible | 21.4 | |
| Preventability | Preventable | 16.1 |
| Non-preventable | 82.1 | |
| Non-assessable | 1.8 |
To identify possible risk factors, variables namely age, sex, body weight, ART status, polypharmacy and CD4 count were subjected to multivariate regression analysis and none of these variables show an association (Table 5).
Table 5: Summary of the multivariate analysis that test the association of some background characteristics and hepatotoxicity among HIV patients on IPT.
| Background Characteristics | Patients developed hepatotoxicity | Multivariate logistic regression analysis | ||||
|---|---|---|---|---|---|---|
| Number of study participants | % of patients with hepatotoxicity | Adjusted Odds ratio | 95% CI | P-value | ||
| Broad age group | 55 and above | 32 | 9.4 | 1 | reference | reference |
| 15-34 | 82 | 17.1 | 1.93 | 0.50-7.51 | 0.344 | |
| 35-44 | 157 | 15.9 | 1.71 | 0.47-6.20 | 0.416 | |
| 45-54 | 89 | 15.7 | 1.7 | 0.54-6.45 | 0.435 | |
| Sex | Male | 109 | 13.8 | 1 | reference | reference |
| Female | 251 | 16.3 | 1.08 | 0.54-2.20 | 0.822 | |
| ART status | Efavirenz based | 122 | 12.3 | 1 | reference | reference |
| Nevirapine based | 238 | 17.2 | 1.38 | 0.70-2.70 | 0.352 | |
| Number of drugs he/she was taking | Five | 274 | 15 | 1 | reference | reference |
| 6 and more | 86 | 17.4 | 2.11 | 0.92-4.83 | 0.078 | |
| CD4 count | Below 200 | 43 | 7 | 1 | reference | reference |
| 200-349 | 69 | 17.4 | 3.86 | 0.95-15.60 | 0.058 | |
| 350 and above | 248 | 16.5 | 3.13 | 0.79-12.39 | 0.1 | |
| Total | 360 | 15.6 | ||||
IPT: Isoniazid Preventive Therapy; ART: Antiretroviral Therapy; CI: Confidence Interval
Discussion
This study revealed a higher incidence rate of hepatotoxicity associated with the use of IPT compared to previous findings [4-8]. Though fatalities had been prevented with the monthly laboratory monitoring, the occurrence of severe and very severe hepatotoxicity was unavoidable in substantial number of patients. Moreover, the short time to reaction onset, median 34 days, reflects that hepatotoxicity following use of IPT is likely to happen within a month making risk minimization approach challenging even with close laboratory monitoring. This is inconsistent with the WHO recommendation that encourages member states to use IPT without routine laboratory monitoring [17].
The probability that hepatotoxicity is linked to IPT is favoured by the fact that majority of the study population were stable on HAART for several years before the initiation of IPT. Besides, reaction recovered merely following withdrawal of IPT in majority of the cases and other possible alternative explanations were ruled out in all but three cases. The high rate of IPT discontinuation in several patients might contribute to resistance of Isoniazid. The treatment of HIV has also been compromised with the introduction of IPT.
Although our previous hypothesis [19] suggested that low body weight of patients (overdose), being female and old age could be risk factors for the occurrence of Isoniazid-induced hepatotoxicity, none of these suspected risk factors are found to be significantly associated with the occurrence of hepatotoxicity in this study. However, it is important to note that patients with higher CD4 count were more likely to develop hepatotoxicity compared to those with lower CD4 count as the p-value hits near the cut point of the level of significance (AOR=3.86; 95%CI: 0.95-15.60; p=0.058). In this study, patients on IPT taking Nevirapine-based HAART had no increased risk of hepatotoxicity compared to those taking Efavirenz-based regimen.
The strength of the study is that the protocol was developed and reported according to ENCePP checklist [23] and STROBE guidelines [24] respectively. On the other hand, the main limitation of the study was lack of a comparator group which was not possible to do so as it is unethical to deprive patients from taking Isoniazid for study purposes.
Conclusion
In conclusion, the risk of hepatotoxicity associated with IPT is much higher than what is reported with a very short time to reaction onset. Though fatalities might have been prevented with the monthly laboratory monitoring introduced for the study purposes, the occurrence of severe and very severe hepatotoxicity was unavoidable in substantial number of patients. Taking the above facts into consideration and the relatively low rate of TBHIV co-infection in the country [25], deployment of IPT in Eritrea seems challenging which requires immediate risk/effectiveness assessment and further risk minimization plans. To identify and manage cases at earliest, we recommend a closer laboratory and clinical follow-ups especially for the first two months of treatment.
Declarations
Consent for publication: All co-authors have given their consent for publication.
Competing interests: The authors declare that they have no competing interests.
Authors' contribution: All of the authors played a key role on the analysis, interpretation of the cases, write-up and editing of the manuscript.
Acknowledgments
The authors would like to acknowledge Mussie Biemnet, Orotta National Referral Hospital, Zewdi Yirgalem from Sembel Hospital and Mehari Zeregabr from the Eritrean Pharmacovigilance Centre for their immense collaboration and assistance during the study period.
REFERENCES
- Badje A, Moh R, Gabillard D, Guéhi C, Kabran M, Ntakpé JB, et al. Effect of isoniazid preventive therapy on risk of death in west African, HIV-infected adults with high CD4 cell cou nts: long-term follow-up of the Temprano ANRS 12136 trial. Lancet Glob Health. 2017;5(11):e1080-e1089.
- Martinson NA, Barnes GL, Moulton LH, Msandiwa R, Hausler H, Ram M, et al. New regimens to prevent tuberculosis in adults with HIV infection. N Engl J Med. 2011;365:11-20.
- Golub JE, Cohn S, Saraceni V, Cavalcante SC, Pacheco AG, Moulton LH, et al. Long-term Protection from Isoniazid Preventive Therapy for Tuberculosis in HIV-Infected Patients in a Medium-Burden Tuberculosis Setting: The TB/HIV in Rio (THRio) Study. Clin Infect Dis. 2015;60(4):639-645.
- Grant AD, Mngadi KT, van Halsema CL, Luttig MM, Fielding KL, Churchyard GJ. Adverse events with isoniazid preventive therapy: experience from a large trial. AIDS. 2010; Suppl 5:S29-S36.
- Tedla Z, Nguyen ML, Sibanda T, Nyirenda S, Agizew TB, Girde S, et al. Isoniazid-associated Hepatitis in adults infected with HIV receiving 36 months of Isoniazid Prophylaxis in Botswana. Chest. 2015;147(5):1376-1384.
- A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015; 373(9):808-822.
- Rangaka MX, Wilkinson RJ, Boulle A, Glynn JR, Fielding K, van Cutsem G, et al. Isoniazid plus antiretroviral therapy to prevent tuberculosis: a randomised double-blind placebo-controlled trial. Lancet. 2014;384(9944):682-690.
- Ngongondo M, Miyahara S, Hughes MD, Sun X, Bisson GP, Gupta A, et al. Hepatotoxicity during Isoniazid preventive therapy and antiretroviral therapy in people living with HIV with severe immunosuppression: A secondary analysis of a multi-country open-label randomized controlled clinical trial. J Acquir Immune Defic Syndr. 2018;78(1):54-61.
- Metushi IG, Nakagawa T, Uetrecht J. Direct oxidation and covalent binding of isoniazid to rodent liver and human hepatic microsomes: humans are more like mice than rats. Chem Res Toxicol. 2012;25(11):2567-2576.
- Metushi IG, Uetrecht J. Isoniazidâ€Âinduced liver injury and immune response in mice. J Immunotoxicol 2014;11(4):383-392.
- Metushi IG, Cai P, Vega L, Grant DM, Uetrecht J. Paradoxical attenuation of autoimmune hepatitis by oral isoniazid in wildâ€Âtype and Nâ€Âacetyltransferaseâ€Âdeficient mice. Drug Metab Dispos. 2014;42(6):963-973.
- J L, Ig M, Jp U, Einhorn S, Da M, Pb W, El LC. Investigation of Isoniazid DILI Mechanisms in Human Induced Pluripotent Stem Cell Derived Hepatocytes. Drug Metab Rev. 2014;45:177.
- Meng X, Maggs JL, Usui T, Whitaker P, Ns F, Dj N, et al. Autoâ€Âoxidation of isoniazid leads to isonicotinicâ€Âlysine adducts on human serum albumin. Chem Res Toxicol. 2015;28(1):51-58.
- Millard PS, Wilcosky TC, Reade-Christopher SJ, Weber DJ. Isoniazid related fatal hepatitis. West J Med. 1996;164(6):486â€Â491.
- Salpeter SR. Fatal isoniazid-induced hepatitis. Its risk during chemoprophylaxis. West J Med. 1993;159(5):560â€Â564.
- Kopanoff DE, Snider DE, Caras Jr GJ. Isoniazid-related hepatitis: a U.S. Public Health Service cooperative surveillance study. Am Rev Respir Dis. 1978;117:991â€Â1001.
- World Health Organization. Adverse events associated with the use of isoniazid preventive therapy among people living with HIV. Geneva, Switzerland: Information note; 2015.
- WHO. Guidelines on intensified tuberculosis case finding and isoniazid preventive therapy for people living with HIV in resource constrained setting. Geneva, Switzerland. 2011.
- Russom M, Debesai M, Zeregabr M, Berhane A, Tekeste T, Teklesenbet T. Serious hepatotoxicity following use of isoniazid preventive therapy in HIV patients in Eritrea. Pharmacol Res Perspect. 2018;e00423.
- Naranjo CA, Busto U, Sellers EM. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239â€Â245.
- Benkirane R, Soulaymani R, Khattabi A, Benabdallah G, Alj L, Sefiani H, et al. Assessment of a new instrument for detecting preventable adverse drug reactions. Drug Saf. 2014;38(4).
- US-FDA. Guidance for Industry: Toxicity Grading Scale for Healthy Adult and Adolescent Volunteers Enrolled in Preventive Vaccine Clinical Trials. September 2007.
- The European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP). Guide on Methodological Standards in Pharmacoepidemiology (Revision 5). EMA/95098/2010.
- Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the reporting of observational studies in Epidemiology (STROBE) statement: guidelines for report-ing observational studies. BMJ. 2007. 335(76264):806-808.
- WHO. Global Tuberculosis Report. 2018.
Citation: Russom M, Berhane A, Debesai M, Andom H, Tesfai D, Zeremariam Z, et al. (2019) Challenges of Hepatotoxicity Associated with Isoniazid Preventive Therapy among People Living with HIV in Eritrea. Adv Pharmacoepidemiol Drug Saf 8:2
Copyright: �© 2019 Russom M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.