Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
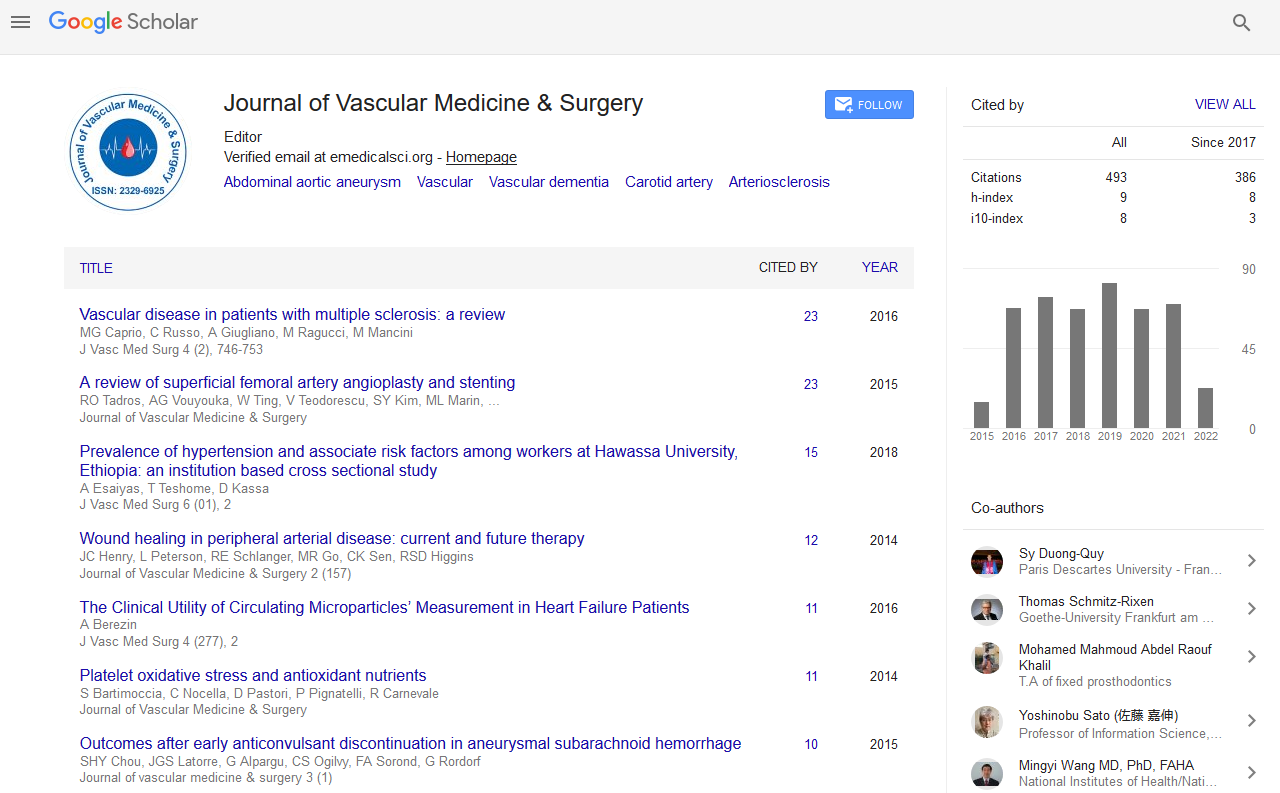
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2021) Volume 0, Issue 0
Cardiovascular Complications after Open-Heart Surgery
Himanshu Chawla*Received: 04-May-2021 Published: 26-May-2021, DOI: 10.35248/2329-6925.21.s5.004
Abstract
Open-heart surgery is any kind of surgery in which a surgeon makes a large incision (cut) in the chest to open the rib cage and operate on the heart. "Open" refers to the chest, not the heart. Depending on the type of surgery, the surgeon also may open the heart. This surgery on the heart or great vessels performed by cardiac surgeons. It is often used to treat complications of ischemic heart disease (for example, with coronary artery bypass grafting) to correct congenital heart disease or to treat valvular heart disease from various causes, including endocarditis, rheumatic heart disease, and atherosclerosis. It also includes heart transplantation.
Keywords
Heart; Cardiovascular surgery; Aortic valve; Cardiac arrest
Description
In patients undergoing major vascular surgery, Cardiac complications are the leading cause of perioperative and late mortality and morbidity. The involvement of underlying coronary artery disease is linked to this (CAD). Diabetic neuropathy and decreased exercise ability due to non-cardiac diseases such as a stroke or claudication may make CAD asymptomatic. The surgeon has a rare opportunity to improve patients' perioperative and long-term outcomes by carefully evaluating and managing cardiac risk factors prior to surgery. Risk reduction strategies aimed at reducing the incidence of perioperative cardiac complications can be grouped into two categories: Perioperative medical therapy and pre-operative coronary revascularization [1].
Cardiovascular disease is the leading cause of death globally and is responsible for 17 million deaths per year. Approximately 85% of cases occur in developed countries and the phenomenon is one of the consequences of population aging. The cardiological postoperative complications considered were: fatal AMI and non- fatal AMI, congestive heart failure, cardiogenic shock, Acute Atrial Fibrillation (AAF) and other arrhythmias [2].
The RCRI reliably predicts death and nonfatal myocardial infarction in patients undergoing vascular surgery, but preoperative coronary artery revascularization does not minimize the risk of death or nonfatal myocardial infarction in any high-risk subset of the RCRI. In stable patients undergoing non-urgent major non- cardiac surgery, this index can identify patients at higher risk for complications. This index may be useful for identification of candidates for further risk stratification with noninvasive technologies or other management strategies, as well as low-risk patients in whom additional evaluation is unlikely to be helpful.
History of congestive heart failure, pulmonary edema, or paroxysmal nocturnal dyspnea; physical examination showing bilateral rales or S3 gallop; or chest radiograph showing pulmonary vascular redistribution were all used to characterize congestive heart failure. Both of these factors were found to be linked to significant cardiac complications.
When Open Heart Surgery Needed?
Open-heart surgery may be done to perform a CABG. A coronary artery bypass graft may be necessary for people with coronary heart disease. Coronary heart disease occurs when the blood vessels that provide blood and oxygen to the heart muscle become narrow and hard. This is often called “hardening of the arteries.” Hardening occurs when fatty material forms a plaque on the walls of the coronary arteries. This plaque narrows the arteries, making it difficult for blood to get through. When blood can’t flow properly to the heart, a heart attack may occur.
Risks for open-heart surgery include chest wound infection, heart attack or stroke, irregular heartbeat, lung or kidney failure, chest pain and low fever, blood clot, etc.When you wake up after surgery, you will have two or three tubes in your chest. These are to help drain fluid from the area around your heart. You may have intravenous (IV) lines in your arm to supply you with fluids, as well as a catheter (thin tube) in your bladder to remove urine. You will also be attached to machines that monitor your heart. Nurses will be nearby to help you if something should arise. You will usually spend your first night in the Intensive Care Unit (ICU). You will then be moved to a regular care room for the next three to seven days.
Conclusion
Most people who’ve had a CABG benefit from participating in a structured, comprehensive rehabilitation program. This is usually done outpatient with visits several times a week. The components to the program include exercise, reducing risk factors, and dealing with stress, anxiety, and depression. Increases in the physician- to-patient ratio in the ICU, as well as intensivists rounding, can lead to a reduction in in-hospital mortality and cardiac arrest. Pre-operative cardiac assessment of patients undergoing major vascular surgery also allows physicians to minimize perioperative and late cardiac risk by preventing complications and providing the best possible care of myocardial ischaemia.
REFERENCES
- Klein KJ, Urk HV, Bax JJ, Poldermans D. Cardiac complications after elective major vascular surgery. Acta Anaesthesiol Scand. 2003; 47(6): 643-54.
- Pereira KSM, de Oliveira JCP, de Carvalho FC, van Bellen B. Cardiac complications in vascular surgery. J Vasc Bras. 2016; 15(1): 1-3.
Citation: Chawla H (2021) Cardiovascular Complications after Open-Heart Surgery. J Vasc Med Surg.S5:002.
Copyright: © 2021 Chawla H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.