PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
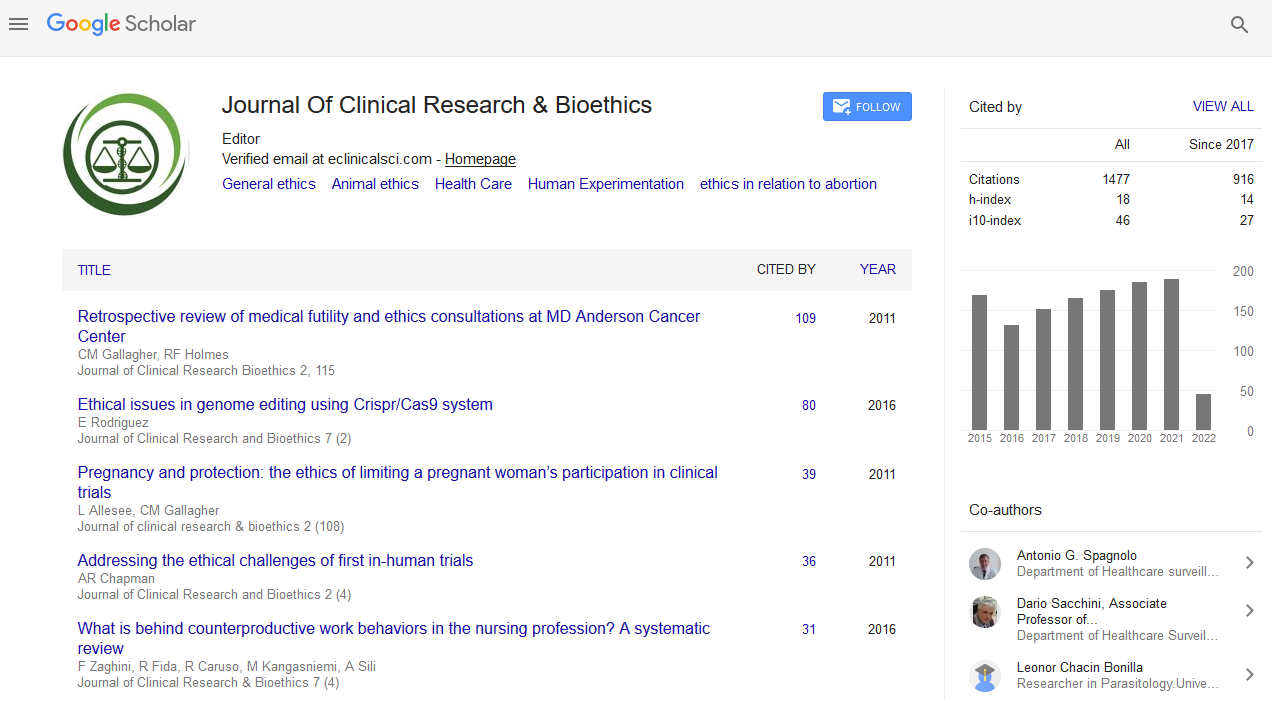
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Mini Review - (2020) Volume 11, Issue 5
Can Health Care Provider be a Surrogate Decision Maker?
Sobia Latif1* and Adnan Yaqoob22Department of Nursing, The University of Lahore, Lahore, Pakistan
Received: 26-Aug-2020 Published: 16-Sep-2020, DOI: 10.35248/2155-9627.20.11.361
Abstract
This commentary article is based on surrogate decision making which arises conflict for not giving consent for surgery but the health care provider (surgeon) took decision for surgery on the behalf of family to ensure a successful outcome for the patient. Ethics are central to the clinical practice of quality and safety of patient life. The informed consent process for emergency surgery and his surrogate as well as parents should make conclusion in regarded less time. The special cases of a surgical emergency developed possible complication to attain the target plan of the late decision for patient surgery, in the favor of patient right and humanitarian. The aim of this study is to lead a real direction for health care provider to take decision for surgery on the behalf of family for patient surgery in emergency situation.
Keywords
Surrogate decision; Intra-cranial bleed; Craniotomy; Hippocratic oath; Health Care Providers (HCP)
Scenario
A 30 year old male landed up in Neuro emergency followed by a Road Traffic Accident (RTA) with head Injury. Patient condition was critical and unconsciously maintained GCS 7/15, CT scan brain revealed intra cranial bleed. The doctor planed for surgery (Craniotomy) on urgent basis but family was not agreed for surgery consent because his father was in abroad who decision taking person in his family was. The family tried to contact with his Father but contact was not possible, that’s why patient surgery delayed and health care provider took decision for surgery on the behalf of family.
Introduction
Health is an essential need for survival of human race this study will focus on health care provider took a decision on the behalf of surrogate decision due to surrogate unable to take decision for patient surgery. When a patient is unconscious and cannot take his decision. An ethical dilemma arises when a health care provider is obliged to take surrogate decision on the behalf of an unconscious patient. To resolve the ethical dilemma legal and ethical domains should appoint authorities who can take decision in the best interest of patient and organization. Health care providers face many challenges related to surgeries and consent. In clinical settings sometimes families can’t be take right decision for surgery and health care provider decided for surgery to save the life of the patient.
Analysis of the Scenario
My case scenario is based on beneficence of patient and health care providers ability to take surrogate decision on the behalf of family. Health care provider followed the theory of teleology to save the life of young patient. In the given scenario health care provider faced conflict for surgery of young patient whose family was unable to take proper decision and health care provider has to take decision for surgery without consent of family. Considering the code of ethics, health care providers violated the principal of autonomy on the behalf of dying person.
1st Position (From the Lens of Family)
Health care organization faces many critical situations in which family cannot take good decision for a critical patient and health care provider has to take surrogate decision on the family to save an ill person. Similarly in my case scenario patient surgery was delayed because family was unable to take right decision, and hospital ethical committee took decision to prevent the patient from complications. Though, the codes of ethics clearly state that patient and family has a right to take decision for treatment and procedure, but in such case health care provider is obliged to violate the principal of autonomy. In addition, health care providers are prone for justice, and have duty of care in order to live up the standards of quality practices. In this critical situation health care providers follow the theory of teleology (moral duty from what is good or enviable as an end to be achieved). Therefore the health care provider’s decision for surgery was based on saving the life of patient whose family does not want to lose their son and was in doubt, to be allowed the surgery or not [1].
In such situations the surgeon should take guidance from the principles of ethics which are enshrined.
2nd Position (From the Lens of Health Care Provider)
Beauchamp and Childress described the ethical principal which can follow in health care delivery system which includes Autonomy, Beneficence, Justice, and Non-malfecence. In my case scenario beneficence and surrogate decision making can be applied because family is unable to take ethical decision However, the principle of the patient’s autonomy is more challenging to evaluate, as the patient is unconscious and added no specific consent for the surgeon to proactively treat. HCP has responsibility to provide high quality care to patient and prevent them from harms. However, in this case HCP has to take ethical decision based on its expertise and knowledge. In clinical organization, ethical committee takes decision which is according to the interest of patients and family. Taking consent is an important document which is ethically important before any invasive procedure. Health care organization should have an ethical committee which consists on persons having knowledge and expertise to manage such ethical situations. In this case surgeons took decision for surgery because patient’s life was in danger and any delay in surgery can lead to severe consequences. Surgery on time can save the young man life; therefore surgeons were obliged to perform the surgery without consent. Surgeons did not consider the family decision as they do for the best interest of patient (beneficence) that was more important. Surgeons follow the Hippocrates oath which state as
“I will remember that I do not treat a fever chart, a cancerous growth, but a sick human being, whose illness may affect the person's family and economic stability. My responsibility includes these related problems, if I am to care adequately for the sick. I will prevent disease whenever I can, for prevention is preferable to cure”.
Therefore decision of surgeons may also be correct in terms of doing good for patient (beneficence). This paper highlights the medical decision of a dying person whose family was unable to take decision for surgery.
Justification of My Position
My view point is in favor of surgeon’s decision for surgery because that can save the patient’s life. Although, the principal of autonomy violated here because ethical committee took decision for surgery without the consent of family. Patient values have to be considered while taking surrogate decisions. This is always a challenging position for health care practitioners to have intercession best in the awareness of patient’s wellbeing and respect of their preferences. Autonomy means self-rule whereby an individual has freedom of his/her own choices and responsible for their decisions. Beauchamp, 1994 as cited by Edwards, 2011 recommended that beneficence should be preference when patient life is in danger. While in this case beneficence is preferred because if we consider the decision of family, patient can be died. Therefore surgeon’s decision was correct because their efforts were for patient’s life [2].
If we analyze the decision which was taken by ethical committee, then it would be in favor patient. If health care provider cannot take decision for surgery and patient died, then they would feel guilt for not saving the life of young boy.
On contrary informed consent is necessary before any invasive procedure to prevent harmful consequences. Consent is significant in the conditions of three important terms that are legitimate, ethical and directorial. Ethically it ropes self-directed decision making and chains goals defined by patients. Organizationally HCP should be role model to take decision. Care is well thought- out as a common practice between a caregiver (nurse/family) and care receiver (patient). Such practice verifies that weather patient’s requirements are met or not. If this practice is not followed properly and the abuse of power occurs with the intent to profit the patient then it is known as paternalism. So patient’s needs and requirements should be given the precedence by taking informed consent over parents will [3,4].
Possible Consequences
Possible consequences may come latter from the patient family as they can file case in healthcare commission against health care providers (Doctors and Nurses).
Practices without ethical consideration can lead to such consequences that can victimize the patients. If HCP’s fails to take surrogate decision, this might be leads to death or more severe complication for patient. Therefore HCP has to take the position of surrogate decision maker to avoid the severe consequences. Although taking consent is important and surgery cannot done without written or verbal consent, but in this case refusal for consent harm the patient and creates a difficult situation for HCPs to proceed or not. At this moment ethical committee has to consider the whole situation and has to provide best decision which is in favor of patient [5,6].
Recommendation
To deal such challenges HCO should conduct conferences to solve the problem and handle such issue ethically. Inventive method of preoperative education should be adopted in the emergency setting to improve the surgical care. Ethical committee should step forward in such challenges to handle the dilemmas. Organization should develop rules to handle situations and conferences should be conducted for this practice. Community should also give awareness on media to cooperate with HCPs to save the life of victim [7,8].
Conclusion
Challenges in health can be tackled by offering health care on basis of priority that would show justice. It is the accountability of the Punjab health department and Ministry of National Health Services. Rules and harmonization for priority setting, WHO guidelines should be follow both at regional and national level. In addition WHO should enlarge their Universal Health Coverage (UHC) in Pakistan with a purpose to amplify thorough and strain care services considering the increasing health care weight. The ambulance services should be harmonized with the hospital triage nurses to make suitable actions before the patient appearance. National Highway and Motorway Authority of Pakistan should cheer headdress and seat belt use and harshly apply rule to journey vehicles in precise lanes to decrease accidental events and deaths and dispirit driving by teenagers and older adults with therapeutic troubles.
REFERENCES
- Brown TM, Cueto M, Fee E. The World Health Organization and the transition from international to global public health. Am J Public Health. 2006; 96(1): 62-72.
- Childress JF, Beauchamp TL. Principles of biomedical ethics: Oxford University Press New York. 2001.
- Hall DE, Prochazka AV, Fink AS. Informed consent for clinical treatment. Cmaj. 2012; 184(5): 533-540.
- Lachman VD. Applying the ethics of care to your nursing practice. Medsurg Nurs. 2012; 21(2): 112-4.
- Strech D, Hurst S, Danis M. The role of ethics committees and ethics consultation in allocation decisions: A 4-stage process. Med Care. 2010; 48(9): 821-6.
- Strech D, Sofaer N. How to write a systematic review of reasons. J Med Ethics. 2012; 38(2): 121-126.
- Strech D, Synofzik M, Marckmann G. How physicians allocate scarce resources at the bedside: A systematic review of qualitative studies. J Med Philos. 2008; 33(1): 80-99.
- Organization, W. H. Constitution of the world health organization. 1995.
Citation: Latif S, Yaqoob A (2020) Can Health Care Provider be a Surrogate Decision Maker? J Clin Res Bioeth. 11:361.
Copyright: © 2020 Latif S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.