PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review - (2021) Volume 12, Issue 1
Bioethical Personal Views on the Medical Care for Elderly People in the So-Called “Terminal Phase”: A Proposal of a Comprehensive Consensus- Building Process as Part of the Double Roles of Physicians
Kenichi Meguro1,2,3*2Cyclotron Radioisotope Center, Tohoku University, Sendai, Japan
3Tohoku University Graduate School of Medicine, Sendai, Japan
Received: 11-Jan-2021 Published: 01-Feb-2021, DOI: 10.35248/2155-9627.21.12.367
Abstract
Medical care for elderly people in the so-called “terminal phase” is a major concern for both medical professionals and social communities. In this report, discussions at three academic conferences and among my research team are introduced based on individual case reports, in addition to presentation of my bioethical personal views: Longevity is determined by “heaven”, A family’s intentions should not be accepted without questioning, A comprehensive consensus-building process is needed as part of the double roles of physicians, and medical life and dignity principles are required, separately from life supremacism and value beyond individuals.Keywords
Medical care; Terminal phase; Professionals; Communities; Supremacism
Introduction
An issue herein presented should continue to be discussed. I have always advocated for the importance of Evidence Based Medicine (EBM) and taught this to my research team. However, although case reports on Narrative Based Medicine (NBM) is the lowest EBM level of 5, it is important as the basis of EBM, begin at “α” and end at “ω”. This report includes my current bioethical personal views based on discussions at three academic conferences and with my research team, using individual cases.
Discussions at Three Academic Conferences
The 40th Annual Meeting of the Neuropsychology Association of Japan
At the 40th Annual Meeting of the Neuropsychology Association of Japan held in Kumamoto in September 2016, we hosted a public project workshop “IV, Executive function: Neuropsychology related to daily life”. The objective of my research team is to support dementia patients in communities based on brain science. When defining executive function as the action control (planning/serial/ parallel) function in daily life, and considering that impairment of social adjustment is related to this function, Behavioral and Psychological Symptoms of Dementia (BPSD), which is important for understanding and support for dementia patients, can be understood as social adaptation disorder to the (personnel and material) environment, rather than just as behavior that is problematic to surrounding people [1].
At the workshop, oral intake disorder, which is easily misunderstood as a symptom of dementia patients in the terminal phase, was also discussed. Dysphagia includes a preceding phase (postural maintenance, cognition of eating, and other actions in a preliminary step to swallowing) and a swallowing phase. The preceding phase is often related to executive function. There are cases in which a patient can eat, but is evaluated as having no function to eat and worse yet, as being in the terminal phase. This raises questions about the correctness of assessment of eating function in medical care settings.
The 36th Annual Meeting of the Japan Society for Dementia Research
At the 36th Annual Meeting of the Japan Society for Dementia Research held in Kanazawa in November 2017, I served as chair of the “Multi-disciplinary collaborative workshop 2: Medical and nursing care for patients with severe dementia in the terminal phase”. In the workshop, difficulty with Artificial Hydration and Nutrition (AHN) performed after oral intake in the terminal phase was a particular focus of discussion. The summary is as follows:
• There was a physician who threatened a family suspicious about AHN by saying “Are you going to starve the patient?” and forced them to accept AHN. A nurse asked for a consultation because she was forced to administer intravenous drips by order of a physician that caused extensive subcutaneous bleeding due to leakage of infusion.
• Based on questionnaire surveys of physicians, infusion in the “terminal phase” may be performed in many cases so that a physician and the family of a patient feel relief by seeing the patient with an infusion bottle, rather than for improvement of the patient. Statements of families of patients to “at least perform infusion” (Semete-tenteki) were also noted.
• However, there is evidence that infusion in the “terminal phase” may decrease brain endorphins.
• Therefore, it is medically reasonable to do nothing when the intention of a patient is unclear, and not to perform infusion based on the intention of the family.
• In addition, some families delusionally believe the power to confer immortality as they hope that an elderly patient will live eternally.
I regret that I did nothing other than explaining these situations as the chair, but I began the symposium after confirming the following points:
• Oral intake becoming impossible does not indicate the “terminal phase”. It is not rare that difficulty with oral intake may develop as a neurological syndrome, also first of all, it is difficult to define the “terminal phase”.
• The intention/behavior of a patient is not necessarily based on decision-making of the patient. Human behaviors are mostly determined at the whim of circumstance. Brain ≠ mind ≠ body. This means that understanding, feeling, and physical needs do not necessarily correspond with each other. This is common in human beings.
• Medical follow-up observation is not equal to “doing nothing”.
• A decision on whether a medical practice is performed to save life or to prolong life, and on whether a disease is in the acute or chronic phase cannot be made before therapeutic effects are confirmed.
I was surprised at many things in the symposium, but it was meaningful that important problems were presented.
The 19th Annual Meeting of the Japanese Society for Dementia Care
Based on the discussions at the two meetings above, I planned an independent symposium, “Support for the elderly in the so-called ‘terminal phase’: A review of medical care and nursing care” at the 19th Annual Meeting of the Japanese Society for Dementia Care held in Niigata in June 2018, to continue the discussion of the importance of NBM at clinical sites.
Medical care, especially infusion and gastrostomy, for patients in the “terminal phase” who have difficulty with oral intake has been widely discussed from medical care and ethical standpoints. In a difficult situation where the intention of a patient cannot be confirmed, on-site medical professionals have to make decisions while taking into consideration EBM, as well as the premorbid intention of a patient, intention of the family, and their cultural and economic backgrounds. Some academic societies have prepared guidelines, but sufficient consideration of on-the-spot opinions in these guidelines requires more discussion. This independent symposium aimed to start this discussion by presenting on-the-spot individual cases related to NBM as evidence.
I placed a focus on the importance of the guidelines in the introduction, as shown in Figure 1. In relationships of the physician with the patient and family, and between guidelines and medical sites, it is not easy to reach a consensus. In addition, “guidelines” are not equal to “manuals”, and the presence of guidelines should not lead to loss of discussion on consensus building. Problems in real on-site situations where medical professionals have difficulty with individual cases are not simple and cannot be solved using academic society guidelines. Legal responsibility may arise at medical and welfare sites, but relationships based on mutual trust are most important.
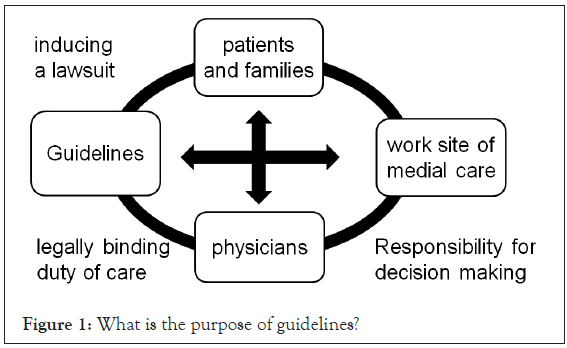
Figure 1: What is the purpose of guidelines?
Discussions in our Research Team
The symposiums at the three academic society meetings above were extremely meaningful because I had opportunities to hear various opinions. The definition of the “terminal phase” among medical professionals and the decision to terminate treatment are major problems.
Based on past experience, I had the impression that the discussions at the meeting were similar to the absurd remark of a certain professor, “therapeutic nihilism”, in which he insisted that there is no requirement for psychosocial intervention and rehabilitation without EBM because dementia would never be cured. I successfully refuted this argument by showing that psychosocial intervention and rehabilitation are also meaningful for evaluation of the efficacy of dementia medication. In addition, I had the experience of clarifying problems related to the difficulty in creating EBM, such as establishing a group for non-specific intervention, etc [1,2].
This is also a problem with the nature of “therapeutic nihilism”. The idea that “psychosocial intervention and rehabilitation are not necessary because dementia is never cured”, is the same as “treatment is not necessary for elderly people because dementia is never cured and those in the “terminal phase” will die a natural death”. With more extreme logic, this develops into the idea that, “all medical procedures are not necessary because human beings will die someday”.
Under the belief that endurance makes a person stronger, vigorous discussions on this important problem have been held in my research team. For these discussions, I provided three cases of NBM, which I remembered from experiences as a physician.
Case A: A woman in her 80’s with cancer who I met during residency. She was a Christian (baptized in childhood) in the last stage of cancer who asked me to tell her everything because she was not afraid to die as she could be beside God. Together with an instructor, I provided as much medical information as possible to the patient and her family. At that time, she showed gratitude. However, in the final stage, she said she did not want to die while holding my hand, and began to chant out loud a Buddhist sutra, Namu Amida Buddha. Her family said, “You are behaving in an embarrassing way as a Christian. Please have greater dignity!” This was the first time I heard the word dignity [REF 1] as a physician.
Case B: A surgeon in his 70’s who believed in medical treatment as a rationalist and had never believe in God. He had severe consciousness disturbance due to systemic metastasis of cancer, but came back to life because of treatment provided by his primary physician. He seemed to face the “door between life and death” and his values totally changed. He expressed his sincere gratitude to surrounding people, who were surprised and said it was not like him.
Case C: A 99-year-old woman who was one of my relatives and was admitted to a special nursing home. She repeatedly developed hypoxic encephalopathy and a gradually decreased consciousness level in a situation with no conversation and oral intake capabilities. She could not recognize me. Since her consciousness disorder continued, I asked for her admission to a core hospital. However, a chief nurse at the hospital said, “it is certain that she is in the “terminal phase” because she is 99 years old and has difficulty with oral intake, and thus, she should be taken care of at a special nursing home”. I insisted that she should receive the best modern medical care, and this was provided at the hospital. Her hypoxic encephalopathy gradually improved and she came back to consciousness. We were able to say goodbye and she thanked me in her last words.
I consider that medical professionals who take care of a patient cannot make a decision about whether his/her dignity can be maintained, or whether the patient is in the “terminal phase”. In addition, agreement of the family of a patient varies depending on individual families. Physicians such as me are in a position to oppose euthanasia [REF 2] in any cases, including “non-voluntary/ inactive euthanasia”, and thus I could take the actions in Case C above. However, other people may reluctantly follow medical professionals due to peer pressure to suspend treatment. Therefore, physicians should have “double viewpoints”, as described below.
The cases presented to our research team included a patient with inability of oral intake and decreased consciousness who lived longer because gastrostomy and AHN improved systemic conditions and enabled oral intake. Based on this case, we also held discussions on gastrostomy. At clinical sites, many patients live longer with a smile and no pain due to gastrostomy. Gastrostomy is covered by insurance in Japan, and is not a special method. Thus, people around a patient should not deny use of this method unilaterally, and should not regard it as a simple life-extending procedure.
Considering “self-judgment ability” and “judgment by family/ medical professionals” for this method, what is not hoped for at present may differ from prediction of future requirements. As mentioned above, the “intention” and “behavior” of a patient are not necessarily based on “decision-making” of the patient. Human behaviors are mostly determined at the whim of circumstance. “Understanding”, “feeling” and “physical needs” do not necessarily correspond with each other. This is common in humans.
There is also a concept of “vulnerability”. There are differences among various advocate groups, but one idea suggests that personal autonomy may be ideal for protection of “vulnerable people” who have difficulty having such autonomy. Another idea suggests that achievement of autonomy is promoted by distinguishing the universal vulnerability in all persons and the special vulnerability of specific groups or individuals. Both are bioethical views, with the former considering personal autonomy to be ideal, and the latter based on universal vulnerability. I suggest that this is the “Papez-MacLean theory” based on the non-integrated condition of a human brain (knowledge=brain vs. emotion=mind vs. life=body) [3,4].
“Longevity” is determined by “heaven”
End-of-life care-related problems are caused because “longevity” is related to the end-of-life care provided to elderly people. In addition, “therapeutic nihilism” easily occurs in medical professionals for old-old patients because the overlapping portion of three circles of “cerebral stroke”, “dementia” and “bed confinement” is higher than that in western countries [5,6].
In Western countries, dementia refers to Alzheimer disease and other neurodegenerative disorders, and the incidence of cerebrovascular disease as a complication is relatively low. In Japan, where the incidence of small infarction is high, cerebral infarction easily develops as a complication in dementia patients, including those with Alzheimer disease and reduces ADL by limiting speech, impairing swallowing, and, even worse, causing a bedridden state. Many Japanese dementia patients or elderly people aged ≥ 100 years can walk stably and take care of themselves after living in Brazil for a long period, after being born with Japanese genes and growing up with elementary education in Japan. This suggests that the large overlap of the three circles is caused by "environment", and not, by "aging" [7,8].
When a patient with severe dementia shows decreased ADL with difficulty in speaking, swallowing and understanding, and requires AHN such as gastrostomy, it is understandable to think that the patient may be coming to the end of his/her life. I remember an experience of being overcome by a sense of helplessness in a situation in which no surgical treatment could be provided for an elderly patient, or no medical procedure could be provided, while receiving training in the department of surgery as a student of a faculty of medicine. In treatment for patients with neurological diseases, especially dementia, in which cooperation between medical and nursing care professionals is extremely important, it should be recognized that both surgery and medical science are only capable of helping a patient to improve and die a natural death; that is, medical science cannot cure the patient.
Regarding “lifespan”, I have always suggested the importance of EBM and taught it to members of my research team. However, I am strongly against intervention of EBM in defining a longer lifespan. Is it required to perform a Randomized Clinical Trial (RCT) for patients in the “terminal phase” to demonstrate that pain may be decreased by increased intracerebral endorphin production with no infusion? If I may be allowed to say something unscientifically, “longevity” is determined by “heaven”. Medical professionals should only face, stay with, and support human beings living in nature.
As seen in Case C above, a 99-year-old patient was viewed as in the “terminal phase” in lifespan theory, but the oldest recorded person was 122 years old.
Case D: Jeanne Louise Calment (1875-1997). A French person recorded as the oldest person worldwide (122 years old). She stated, “I have never become ill so far” [7].
Adolescence: Woke up at 8:00 in the morning and had hot chocolate and cafe au lait as breakfast in her elementary school days.
Adulthood: Married at age 21, enjoyed cycling and mountainwalking, and went to church every Sunday.
Adulthood elderly: Had a broken ankle at age 60 and a broken lower extremity at age 100, but recovered to the ambulatory level with no rehabilitation. At age 88, her grandchild died, and since then she lived alone until age 110. Due to a mistake in fire handling at home, she then moved to a nursing home.
“Super” elderly: Stopped smoking at age 117 because she wanted to live longer. A psychological examination at age 118 suggested verbal memory/fluency similar to that of persons in their 80’s, with normal frontal lobe function and no depression.
This case makes it clear that an age of 99 years is not the end of life. Do those who apply EBM to this situation insist that aggressive treatment is provided before the end of a biological lifespan calculated based on genes of individuals, and should not be provided after the end of the lifespan? First of all, it is doubtful whether EBM can be created without pain for a patient in a situation in which the guidelines of academic societies may be used through a specific principle or opinion based on insufficient EBM. The above-mentioned idea, “intracerebral endorphin production may be increased with no infusion", is based on an animal experiment performed 30 years ago. Science should not intervene in the field of longevity, but EBM requires observation of individual cases before termination of infusion or other interventions.
Family “intention” should not be accepted without questioning As described in one of my books [1], most family members of outpatients sincerely think about the patient and create a trusting relationship with medical professionals as “partners”, so that appropriate treatment and care are provided to the patient. However, such families are ordinary people, not medical professionals, and some provide incorrect information or are not cooperative. Medical professionals should understand that they may encounter these families.
Case E: An 84-year-old male patient with Alzheimer disease with a complication of sick sinus syndrome. He developed bradycardia and fainting, and I explained to his family about a request for a physician from the cardiovascular department to perform insertion of a pacemaker. However, they did not understand, saying that such treatment would be too much because he was such an old man. I strongly recommended the procedure as he had a second fainting episode, and his family reluctantly accepted. It was difficult to confirm the intention of the patient before the procedure because he had impaired cognitive function. The insertion was a normal treatment and the private medical cost was not high. It was explained that he was at risk with two attacks, but it took a long time to have the pacemaker inserted. The patient was older than the average life expectancy of Japanese people, and it is probable that medical treatment was refused due to his high age. This was a typical case of “ageism”.
The adult guardian system enables protection of financial assets of a patient who has lost the capability of property management due to dementia, etc. by establishing a legal guardian, but the guardian has no rights regarding medical practice. However, physical health is an important asset, and a family should not ignore the health problems of a patient by judging a medical practice to be unnecessary without the patient’s permission. Such families may not visit the patient much, whereas nursing staff who take care of the patient every day provide empathetic care to the patient like a true family. However, when a patient has no capability to express agreement, family may be allowed to be a guardian only when medical practices are appropriate. Medical professionals should make the families of patients understand that professionals evenly provide the best treatment and care, while standing on the side of the patient.
Double roles of a physician: Comprehensive consensus building process
I consider that a physician has two roles, as follows:
• As a “soldier” on the front line of the fight: The role of a “soldier” is to fight against diseases to protect the life of patients, and
• As a “politician” for civilian control, or a “manager” to achieve “totally optimized” [REF 3] management: An organizer/manager for consensus building with families, caregivers, etc.
Regarding, it is important prepare for the best performance based only on “conscience” (Oath of Hippocrates). Physicians should choose the best procedures for diseases as specialists. Both physicians and other medical professionals must not abandon selection of therapeutic methods. However, it is not a simple question of whether they can play these roles. Medical sites, economic conditions, preliminary intentions of a patient and family (changeable depending on the disease stage), and other factors produce a complicated mix. The role in should be considered, and a physician should play these two roles by switching viewpoints. For this, it is important that physicians should not add peer pressure on surrounding people. They have to play a role of coordinator and avoid statements when possible.
Members of my research team presented a local criminal case in which a dementia patient committed violence against his wife, who gave him a few words of warning, as group work at a regional comprehensive care meeting held in another area. The meeting participants were absolutely appalled at the behavior in this case because they could not accept it sociocultural and the only physician who participated in the meeting said that the patient should have been moved to a nursing care facility immediately after the violent incident. Then, all participants stopped talking and the discussion was terminated. However, a member of my research team, who was a care manager, continued the group work as the chair, and this grew understanding among the participants. Care management should be performed by physicians and other medical professionals, and thus physicians should be careful about making weighty statements at a meeting with participation of other medical colleagues [9].
In summary of these findings based on the bioethically important “Oath of Hippocrates” and “informed consent”, medical professionals should prepare the best treatment in accordance with the “Oath of Hippocrates”. However, they should manage the comprehensive consensus-building process, placing a focus on the situation of a patient (and family) as much as possible. For this, physicians should avoid statements when possible and never add peer pressure (Figure 2).
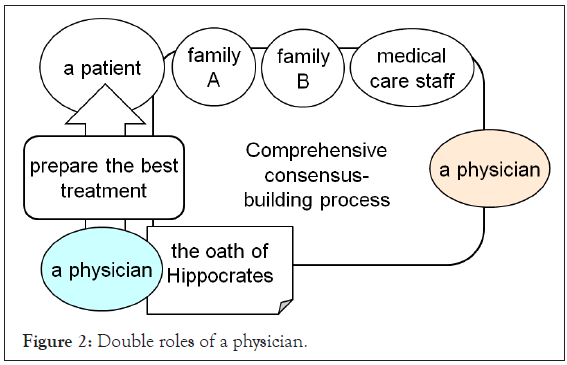
Figure 2: Double roles of a physician.
QOL and dignity: Medical “life” principle/ medical“dignity”principle
The term “QOL” [REF 4], which I feel has a facile nuance, is often compared with dignity in discussions. As seen in Case A, “death with dignity” is associated with some “values” that are against simply prolongation of life. However, only a person has a right to determine how the person lives with dignity, not as a simple living body. Other people, especially medical professionals, do not have the right to determine the life of the person.
I am not a life supremacist. When an absolute priority is placed on life, values of caring only about oneself are formed, with no consideration for surrounding people. Based on the extreme logic of life supremacism, eternal life will be the maximum value, and even surrounding people may have a delusion of elixir of life, as discussed at the 36th Annual Meeting of Japan Society for Dementia Research. Only when values beyond life are confirmed, the importance of limited life is found. “Man is mortal, and art is eternal”. This is in “Kwakyo”, one of Zeami’s writings. Values beyond life are the reason that harakiri (suicide by disembowelment) is deemed more important as honor in bushido (the spirit of the samurai), and that spirits of the war dead should be publicly honored. Besides such exaggerated things, a parent will help his/her child who suddenly runs onto a railway without considering the safety of him/herself. I do not agree with the idea that a person who tries to retrieve a drowning person in a river should be criticized in theory, or that a life was lost for nothing due to no respect for life.
“Values” are developed through mutual interaction with the “principle of values”, which can be expressed as “God” in monotheistic cultural areas, and as “community” which is equal to human relationships, including Shinto and Buddhist deities, in Japan. These should be most respected in internal life as a code of conduct for individuals, irrespective of being conscious or not. However, medical practice is provided to others, not to oneself, with “life” put first. Even if this causes a sense of discomfort, “removal of pain” is understandable. Medical practice is to cure a disease of others with a priority placed on “life” not to cure “values”. Pain may be caused in treatment of a disease, but only “no pain” must be shared as a value in end-of-life care.
Refusal of life extension" based on their own "values" and "values" to adhere rigidly to life while receiving criticism about no dignity from surrounding people, as seen in Case A above, should be equally respected, and surrounding people, especially medical professionals, should not recommend a specific way of death. However, such discussions are not simple because the values, other than removal of pain, are not uniform regarding one of the double roles of physicians, “sociocultural consensus building with surrounding people”, when it becomes difficult for a patient to express their own intention.
Enlightenment of religions including death with dignity may be necessary, but it is not easy to discuss how people should face death in Japan, where “community” culture is a base, rather than monotheistic culture. However, it is certainly the height of hypocrisy if a person recommends death with dignity and termination of useless treatment for others in the terminal phase in medical practice, while the person enjoys his/her life in real society based on the idea of life supremacism without admitting “values” beyond “life”. Consistency can be confirmed if a person admits the “values” beyond life, and hopes for death with dignity when the person is in the “terminal phase”. However, even this should be the internal values of the person, and should not be recommended for others with peer pressure.
I hope here to have considered medical “life” and “dignity” principles from a standpoint of medical care, independently from life supremacism, “values” beyond individuals, and monotheistic principles (Table 1). It is certain that medical professionals should emphasize life, but this idea should be carefully considered to avoid its expansion to entire values, and they should be humble themselves.
| Life supremacy | Medical care | Values beyond individuals | ||
|---|---|---|---|---|
| Medical life supremacy | Medical dignity supremacy | |||
| Consensus with surroundings | Depends on the case? | Important | Depends on the case? | |
| Principle of values | Life | Life | Life with values | God |
| Field of human relationship | ||||
| Removal of pain | Yes | Yes | Depends on the case? | |
| Death with dignity | No death with dignity | No death with dignity | Death with dignity=No pain | Death with dignity ≠ No pain |
| Life>>dignity | Life>dignity | Life<dignity | Life<<dignity | |
| What we call “life extension” treatment | Agree | Disagree | Disagree | Depends on the case? |
Table 1: Medical life and dignity principles from a standpoint of medical care.
Acknowledgment
Valuable discussions with Dr. Hideki Yamazaki and Prof. Atsushi Asai are greatly appreciated.
References
REF 1: “Dignity” is etymologically related to “murti”. According to Nakano dignity is an “invaluable thing”, “importance of others”, “responsibility for others=ethics” and other real feelings that people have in their experiences with “sacred things”, and is totally different from secular values qualitatively.
REF 2: Euthanasia can be divided into four categories: “voluntary” vs. “non-voluntary” and “active” vs. “passive”. Active euthanasia is not discussed in Japan. The medical concern is passive euthanasia for a patient in the “terminal phase”. In Japan, active euthanasia is not allowed culturally, but passive euthanasia is discussed as “death with dignity”.
REF 3: Total optimization is management jargon for an entirely optimized corporation, organization, or system, and suggests thinking processes focused on improvement of the whole organization or system, rather than improvement of partial productivity or efficiency. Medical nursing care for elderly people is provided mainly to the patient, but is also related to “human beings”, including medical professionals and families of patients, as well as surrounding cultural/economic aspects. This indicates the importance of a “comprehensive consensus-building process” (my phrase) at medical sites.
REF 4: Some scholars divide QOL into “medical QOL” and “life QOL” or discuss QOL only for the “quality of a living body”, compared with sanctity of life (SOL). There is need to clarify what is really being suggested, without being captivated by the word “QOL”.
REFERENCES
- Meguro K. Dementia medical science: For dementia countermeasures in local governments-proposal from tajiri project. Emerg Med Publisher. 2011.
- Meguro K. Cholinesterase inhibitors are compatible with psychosocial intervention for alzheimer disease patients suggested by neuroimaging findings. Psychiatry Res Neuroimaging. 2017; 259: 29-33.
- Iketani S. Bioethics and "vulnerability". Bulletin of Ryotokuji University Research. 2016; 10: 37-68.
- Meguro K. Human security: Social support for the health of the aging population based on geriatric behavioral neurology. Nova Science Publishers Inc. 2018.
- Kasai M, Meguro K. Estimated quality-adjusted life-year associated with the degree of activities of daily living in patients with Alzheimer’s disease. Dement Geriatr Cogn Disord. 2013; 3: 482-488.
- Meguro K, Ishii H, Yamaguchi S, Ishizaki J, Shimada M, Sato M, et al. Prevalence of dementia and dementing diseases in Japan: The Tajiri Project. Arch Neurol. 2002; 59: 1109-1114.
- Ritchie K. Mental status examination of an exceptional case of longevity JC aged 118 years. Br J Psychiatry. 1995; 166(2): 229-235.
- Nakano T. Meaning of dignity and human rights. Social Welfare. 2019; 50:1-12.
- Nakashima F, Takada J, Shoji M, Kumai K, Sugawara N, Meguro K. Local residents for cases where they could not be discharged from their homes due to so-called "nuisance" awareness advancement: Significance of community care meetings. Dement Care J. 2011; 105-111.
- Meguro K. Elderly immigrants living in Brazil: Stories and history seen through a dementia survey. Emerg Med Publisher. 2010.
Citation: Meguro K (2021) Bioethical Personal Views on the Medical Care for Elderly People in the So-Called “Terminal Phase”: A Proposal of a Comprehensive Consensus-Building Process as Part of the Double Roles of Physicians. J Clin Res Bioeth. 12:367.
Copyright: © 2021 Meguro K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.