PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
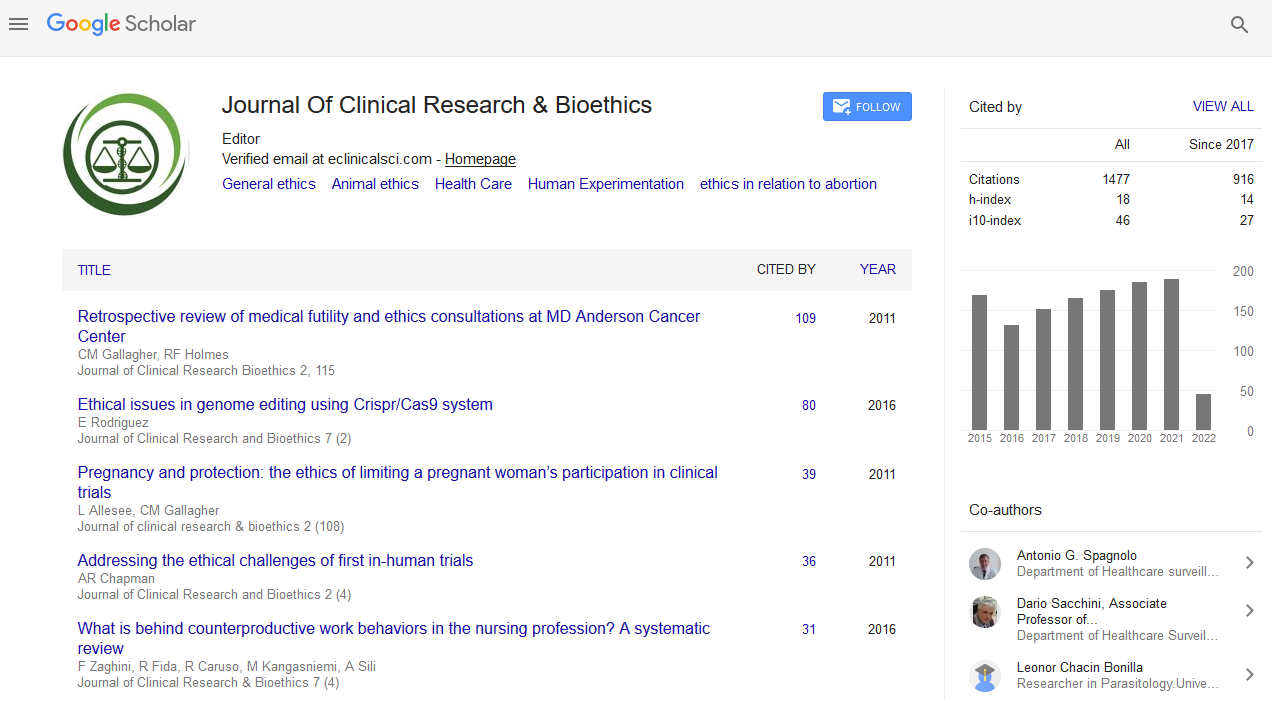
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Paper - (2019) Volume 10, Issue 1
Autonomy in Advanced Chronic Disease
Maia Goncalves A1,2*, Coelho E1, Pacheco A3, Barbosa C3 and Jacomo A22Institute of Bioethics, Universidade Católica Portuguesa, 4169-005, Porto, Portugal
3Serviço de Medicina Interna, Hospital de Braga, 4710-243, Braga, Portugal
Received: 30-Mar-2019 Published: 17-Apr-2019
Abstract
The authors question the respect for the principle of autonomy of the patient admitted into intensive care unit, limiting the scope of the question to the chronically ill. A questionnaire was drafted and distributed to 378 chronically ill patients in Hospital de Braga, which intended to assess whether they were informed of the possibility of the need for admission to intensive care, as well as invasive techniques that they might have to be submitted. The results showed that information was clearly insufficient. The scientific literature articles in this area supports that the lack of information is still very common. So, the authors propose improving this communication. Note that, in the context of chronic disease, prompt information of the patient of the future possibility of need for admission into intensive care is the way to ensure respect of their last will. They suggest that the doctor's commitment to respecting the autonomy of the chronically ill is an opportunity for better care.
Keywords
End-of-life Care; Autonomy; Ethics; Communication; Doctor-patient relationship
Introduction
The respect for patient autonomy is nowadays considered a fundamental ethical principle in clinical practice. Therefore, when a diagnosis is made, the patient should be informed of the possible therapeutic options, prognostic and possible complications. The clinical approach will result from sharing information and patient will. This model is usually designated by Patient Centered Care (PCC) allows a shared decision-making (SDM) [1].
In an intensive care scenario, especially in an emergency, the priority is to resuscitate and initiate advance life support, so mostly there is no room for SMD. Possibly, the exceptions are the presence of an “Advanced Directive of Will” (ADW) or a precise order to Do Not Resuscitate (DNR) in the clinical process.
The natural evolution of chronic diseases allows us to anticipate a future need for admission in intensive care, therefore the patient should be timely informed of that possibility so that he can consciously express his will.
Internal Medicine is not defined by an organ system, by specialized knowledge or complex specific techniques, however it practices the mastery of care [2]. It privileges the doctor-patient relationship favoring a humanistic connection, which is crucial in an increasingly complex fragmented technologic healthcare. In this context, the respect for autonomy is of relevance in Internal Medicine clinical practice.
The aim of this study was to question patients with chronic diseases from Hospital de Braga if their doctors had informed them that they might need a future admission in intensive care. And, about the invasive techniques that might be necessary, namely orotracheal intubation, mechanic ventilation or tracheostomy.
Methods
The authors did a cross-sectional study including patients with chronic disease, defined by World Health Organization (WHO), admitted in Intensive Care Unit (ICU) or in Internal Medicine Department (IMD) of Hospital de Braga, from April 6th to November 19th of 2017. Patients from IMD also needed to fulfill criteria for a possible future admission in ICU.
Patients were grouped by most frequent chronic diseases defined by WHO: cardiovascular, oncologic, kidney, pulmonary and diabetes. Recorded data also included: age, literacy, previous information about need for admission in ICU (given by his doctor), as well as need for invasive measures (orotracheal intubation, mechanic ventilation or tracheostomy); and, if the patient wanted to know more about ICU.
Statistical analysis was done with IBM SPSS Statistic, version 22.
Ethical and deontological principles referring to the best practice in recording and data analysis were respected through the entire study.
Results
378 patients were included: 53.2% from ICU and 46.8% from IMD. Mean age was 59.95 with a median of 62, ranging from 20 to 81-year-old. Regarding literacy: 13.2% were illiterate, 19.3% had 4 years of school, 20.4% had 6 years of school, 18% had 9 years of school, 16.9% finished high school and 12.2% had a university degree.
Concerning chronic disease, there was a greater prevalence of cardiovascular disease (33.9%), followed by pulmonary (27.8%), kidney (16.9%), diabetes (11.6%) and oncologic disease (9.8%).
76.7% of all patients included answered that they had no information about a possible admission in ICU; it was verified that there was no significant interdependency between OMS chronic disease groups and these information (p=0.155). A significant interdependency was verified between literacy and information about possible need for ICU admission (p<0.001), with least literate patients tending to respond “No” and welleducated (more than 6 years of school) tending to respond “Yes”.
There were 88 patients (23.3%) affirming to have information about possible need for ICU admission. In this group, 24.4% knew about possible orotracheal intubation, 13.8% knew about possible mechanical ventilation and 4.2% knew about a possible tracheostomy.
When asking about if they would like to know more about ICU, 81.5% of patients responded “Yes”. There was a significant interdependency (<0.001) of the answer to this question and literacy, mostly related to illiterate leaning to respond “No” when compared to literate patients. In OMS chronic disease groups was also verified a significant interdependency (p=0.006) with the answer to this question, in with oncologic and diabetic patients lean to respond “No” more than the other groups.
Discussion
Patients with concomitant chronic diseases are increasingly frequent and magnify complexity of healthcare. In developed countries, one out of four adults have at least 2 chronic conditions, and more than a half of older patients have three or more chronic diseases [3,4].
The average life expectancy in developed countries will be 85-87 years-old by 2050, with an associated inversion of demographic pyramid [5].
One could say that the demographic and epidemiologic changes have important implications in healthcare and bring new ethical and clinical challenges. It would not make any sense that the clinical and scientific progress had conquered a remarkable increase in life expectancy and now there was no ability to respond to new challenges. There are big challenges mostly concerning Nacional Healthcare System, and there are huge challenges each individual face every day taking care of patients with multiple chronic diseases with increasingly advanced ages.
Guidelines are excellent to support clinical decision; however, they are related to only one clinical entity.
Although pharmacological interactions can be anticipated, the probability of side effects is enhanced when five or more drugs are associated. Even though in some scenarios adding more drugs will benefit the patient, when facing multiple chronic diseases and/or fragility/deficiency the probable benefit diminishes outbalanced by the increased risk of harm [6].
The use of devices in older patients, such as implantable cardiac defibrillators, must be well pondered because in many cases the mortality is not diminished [7].
Or deciding to initiate haemodialysis in advanced aged patients. It is known that older adults with advanced chronic renal failure have high probability of death by other causes. Exception to this scenario is rapidly progressive kidney injury in an otherwise healthy patient. Is initiating renal replacement therapy a clinically and ethically easy decision? [8,9].
What about valvular cardiac diseases? Aortic stenosis (AS) is the most common valvular disease in developed countries and its impact on public health resources will increase because of aging of western population. In a study from United States of America, prevalence of AS in patients older than 75 years old was 12.4%, with 3.4 of sever AS. The authors concluded that about 290000 elderly with high surgical risk could be treated with transcatheter aortic valve replacement. These estimates have considerable clinical, ethical, economic and social implications [10].
The list of many more procedures in which the clinical and ethical decision about the clinical approach defies the best clinical sense, would be necessarily extensive. These are daily decisions to Internal Medicine physicians or in which they are called to participate.
Those who treat elderly with multiple chronic diseases are frequently confronted with the need to consider the benefit of an intensive care admission during an exacerbation. Nowadays, it is frequent that these patients are proposed to admission in intensive care during acute exacerbations of chronic diseases [11].
A study made in Portugal between 2000 and 2010 concluded that patients older than 75 years old admitted in ICU almost doubled (1837 patients in 2000, and 3491 patients in 2010) [12]. The benefit of admission of elderly in intensive care is not established [13]. There are no defined clinical criteria. There are few published literatures but with no objective conclusions. Nowadays, there is no ideal combination of independent prognostic factors associated to the benefit of elderly admission in intensive care. Even in the same country, there are different opinions in the triage method. Besides age, other important prognostic factors in the critically ill elderly are comorbidities and geriatric syndromes such as fragility, sarcopenia and dementia [14].
For instance, one can consider that the reason to propose an admission of a patient to intensive care is an understanding that the physiologic reserve of the patient is enough to endure it and that the clinical situation is reversible. Intensive care is a sparse resource with high cost. In its routine are included several invasive procedures which can carry life-threatening complications, namely invasive mechanic ventilation, placing of central venous catheters or intracranial pressure monitoring, etc. [15].
In general, all patients admitted in intensive care are critically ill and have life-threatening conditions in which intensive care resources are needed. It is also known that if the physiologic reserve of a patient is already very limited, the catabolism and physiologic demand of an intensive care admission will result in a huge increase in intra-hospital mortality (compared to other age groups), even if the patient is discharged from ICU [16,17].
This is usually the method whether to propose a patient for intensive care admission: Taking in account the state odd art, being as updated as possible, analysing all variables and sharing the decision with Intensive Care physicians. However, most of the times, the main intervenient in these decision-making process (the patient), never had a chance to express his will. Obviously, the opportunity for participate in this decisionmaking process is not during a severe acute exacerbation. The time frame for that kind of intervention had already existed. In follow-up appointments, options of end-of-life care should be discussed in the same way as the introduction of new drugs or treatments. It must be kept in mind that in a future emergency there might be no place for informed consent and, if not explicit, the patient’s last will may not be respected. In an elderly patient with multiple chronic diseases, the odds of needing an intensive care admission are very high. A timely information to the patient, taking in account the implicit scenario of intensive care, is a way to respect the autonomy principle. The authors think that this is an area were the mastery of internal medicine doctors can be optimized, one of the reasons which led to this questionnaire.
The results are very clear, only 23.3% of all patients had been informed about the possibility of an intensive care admission; in these sub-group, only 4.2% were aware of tracheostomy. In other words, less than a quarter of all patients had been informed about the possibility of an intensive care admission. The content of the provided information would not have been very enlightening, given the near-ignorance of the invasive techniques that they would eventually have to face if they were admitted in intensive care. It is evident that these conclusions cannot be generalized to other hospitals or countries. However, there is literature showing similar results all over the world. There are several alerts for the need to give better information to cardiac failure patients, both in United Stated of America and in Europe [18,19].
Chronic respiratory failure is a terminal irreversible increasingly frequent condition in which an acute exacerbation can lead to inadequate admission in intensive care. To submit these patients to orotracheal intubation and invasive mechanical ventilation leading to difficult or impossible ventilatory weaning is certainly clinically and ethically bad practice. Most of the times, the patient ends up with a tracheostomy and he is discharged to general ward highly dependent of a portable ventilator. There are also several publications in chronic respiratory failure proving that the patient needs to be better informed [20,21].
In oncological disease, it’s clear that the patients often benefit from the intensive care support, namely after surgery, in the treatment of infectious complications and of iatrogenic consequences of chemotherapy and radiotherapy. When the oncological disease develops despite the implemented therapeutic measures and the patient shows a simultaneous cachexia progression, admission of such a patient in the ICU would be therapeutic fixation [22,23].
In Portugal, the Internal Medicine physician is frequently a permanent back up to patients admitted in all hospital wards. In most patients, the opportunity for previous information is not responsibility of the Internal Medicine physician. But in some cases, it may be; and the respect for patient autonomy is an opportunity to better care and to enhance the doctor-patient relationship. When a patient trusts his doctor to properly clarify and inform him, so that they can consciously decide therapies that the patient wants to be submitted when in is not able to express it, is to entrust the doctor to respect the patient last will. Many therapeutic fixations could have been avoided if patients with chronic diseases have had the possibility to express their wishes [24].
At last, ADW is one more step to respect the patient’s autonomy. Patients with chronic diseases who survived an intensive care admission have a great opportunity to do an ADW, given the experience of care they went through. In followup appointments, it would be interesting to question these patients is they would like to be readmitted in intensive care [25,26].
Conclusions
During this study in Hospital de Braga, patients were insufficiently informed about the natural evolution of their conditions, namely the possibility of admission in intensive care and invasive technics they might have to be subjected. According to the reviewed literature, this information deficit is described all over the world.
The respect for patient’s autonomy must be considered an opportunity for better care; it will contribute to avoiding fixation therapy and will certainly improve communication and strengthen doctor-patient relationship.
With nowadays epidemiologic and demographic challenges, the respect for autonomy is a crucial principle in medical practice. The risk of excessive exaltation of this principle is to consider autonomy as a way of not holding the doctor responsible for clinical decisions. As Walter Oswald said “No one can deny that autonomy is an important value, but it is nor reasonable to attribute such a relevant axiological meaning that it overcomes all other values and principles.” Finally, as health professionals, we want to stress that it is in the hands of all of us to transform the aging in the continuation of a journey of full life.
REFERENCES
- Sandman L, Munthe C. Shared decision making, paternalism and patient choice. Health Care Anal. 2010;18:60-84.
- Shapiro MF. Challenges and opportunities for general internal medicine, J Gen Intern Med. 2004; 19: 95-96.
- Mercer SW, Smith SM, Wyke S, O Dowd T, Watt GC. Multimorbidity in primary care: Developing the research agenda. Fam Pract. 2009;26:79.
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet. 2012;380:37.
- Wilmoth JR. Demography of longevity: Past, present, and future trends. Exp Gerontol. 2000;35:1111-1129.
- Fried TR, Mecca MC. Medication appropriateness in vulnerable older adults: Healthy skepticism of appropriate polypharmacy. J Am Geriatr Soc. 2019;30.
- Ferretto S, Zorzi A, Dalla Valle C, Migliore F, Leoni L, De Lazzari M, et al. Implantable cardioverter-defibrillator in the elderly: Predictors of appropriate interventions and mortality at 12-month follow-up. Pacing Clin Electrophysiol. 2017;40:1368-1373.
- Schell JO, Patel UD, Steinhauser KE, Ammarell N, Tulsky JA. Discussions of the kidney disease trajectory by elderly patients and nephrologists: A qualitative study. Am J Kidney Dis;59:495-503.
- Thorsteinsdottir B, Swetz KM, Tilburt JC. Dialysis in the frail elderly-A current ethical problem, an impending ethical crisis. J Gen Intern Med. 2013;28:1511-1516.
- Osnabrugge RL, Mylotte D, Head SJ, Van Mieghem NM, Nkomo VT, Le Reun CM, et al. Aortic stenosis in the elderly: Disease prevalence and number of candidates for transcatheter aortic valve replacement: A meta-analysis and modeling study. Journal of the American College of Cardiology. 20132;62:1002-1012.
- Robert R, Skrifvars MB, Ranzani OTR. Is this critically ill patient elderly or too old? Intensive Care Med. 2017;43:1884-1886.
- Silva CB, Alves D, Lopes F, Freitas A, Goncalves AM. Elderly mortality in portuguese ICU-an 11-year survey. Journal of Critical Care.2015;30:836-837.
- Boumendil A, Angus DC, Guitonneau AL, Menn AM, Ginsburg C, Takun K, et al. Variability of intensive care admission decisions for the very elderly. PLoS One. 2012;7:e34387.
- Flaatten H, De Lange DW, Artigas A, Bin D, Moreno R, Christensen S, et al. The status of intensive care medicine research and a future agenda for very old patients in the ICU. Intensive Care Med. 2017;43:1319-1328.
- Heyland D, Cook D, Bagshaw SM, Garland A, Stelfox HT, Sangeeta M, et al. The very elderly admitted to ICU: A quality finish? Crit Care Med. 2015;43:1352-1360.
- Guidet B, Leblanc G, Simon T, Woimant M, Quenot JP. Effect of systematic intensive care unit triage on long-term mortality among critically ill elderly patients in France: A randomized clinical trial. JAMA. 2017;318:1450-1459.
- Mukhopadhyay A, Tai BC, See KC, Ng WY, Lim TK, Onsiong S, et al. Risk factors for hospital and long-term mortality of critically Ill elderly patients admitted to an intensive care unit. Biomed Res Int. 2014.
- Lauridsen C. Ethics of shared decision-making for advanced heart failure patients. Online Journal of Health Ethics. 2013;9.
- Wiskar K, Toma M, Rush BK. Trends in cardiovascular medicine. 2018;28:445-450.
- Monteiro J. Life-sustaining treatments in end-stage chronic respiratory failure: A single-centre study. Clinical Ethics. 2017;13:26-33.
- Haq AU. Ethical dilemma in multiple co-morbid respiratory failure patient: Patient autonomy against family wishes? Anaesth Pain & Intensive Care. 2012;16:280-282.
- Pope TM. Legal duties of clinicians when terminally Ill patients with cancer or their surrogates insist on ‘Futile’ treatment. The ASCO post. 2018.
- Koch A, Checkley W. Do hospitals need oncological critical care units? J Thorac Dis. 2017;9.
- Mentzelopoulos SD, Haywood KL, Cariou A, Mantzanas M, Bossaert L. Evolution of medical ethics in resuscitation and end of life. Trends in Anaesthesia and Critical Care. 2016;10:7-14.
- Andreu P, Dargent A, Large A, Meunier Beillard N, Vinault S, Rojas UR, et al. Impact of a stay in the intensive care unit on the preparation of advance directives: Descriptive, exploratory, qualitative study. Anaesthesia Critical Care & Pain Medicine. 2017;37:113-119.
- Walter Osswald. On death and dying. Francisco Manuel dos Santos Foundation, Lisbon, Portugal. 2013.
Citation: Goncalves AM, Coelho E, Pacheco A, Barbosa C, Jacomo A (2019) Autonomy in Advanced Chronic Disease. J Clin Res Bioeth 10:332.
Copyright: © 2019 Goncalves AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.