Indexed In
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2019) Volume 3, Issue 2
Atypical Posterior Reversible Encephalopathy Syndrome (PRES) in Eclampsia in Primigravida with Twin Pregnancy: A Case Report
Surekha S Chavan, Madhu A Chavan*, Priyanka Gedam, Ishaa Pradhan, Stefen Jebaraj and Priya ChavreReceived: 11-Nov-2019 Published: 02-Dec-2019
Abstract
“Posterior Reversible Encephalopathy Syndrome” (PRES) is a clinico-neuroradiological syndrome of heterogeneous etiologies. The syndrome is characterized by headache, visual disturbances, altered consciousness, seizure disorder, focal neurological signs, lethargy, nausea/vomiting. When areas of brain other than parieto-occipital region are predominantly involved, the syndrome is called atypical PRES, which is a rare clinical entity. The global incidence of PRES is unknown, but high in patients with eclampsia. PRES is a reversible condition but can be fatal. Delay in diagnosis and treatment can lead to cerebral ischemia or haemorrhage leading to permanent neurological damage. Magnetic Resonance Imaging (MRI) remains gold standard for diagnosis. Here we report anaesthesia management of emergency caesarean delivery of twins in primigravida woman with Atypical PRES in eclampsia without any neurological deficit.
Keywords
Atypical PRES; Eclampsia; Anaesthesia management
Introduction
“ Posterior reversible encephalopathy syndrome ” (PRES) is a clinico-radiologicalogical entity. In 1986, Hinchey [1] first described the clinical condition “ reversible posterior leukoencephalopathy” (RPLE). Triggers responsible for PRES are preeclampsia, eclampsia, systemic lupus erythematosus, renal failure, severely high blood pressure, chemotherapy, sepsis, organ transplantation, immunosuppressive agents. PRES is characterized by clinical features headaches, consciousness impairments (confusion, somnolence, lethargy and coma), visual disturbances, seizure, and focal neurological signs. Headache remains common clinical presentation. Visual disturbances which range from blurring of vision to permanent visual field defects are also commonly seen.
Typical PRES involves parieto-occipital lobes. When areas of brain other than parieto-occipital region are predominantly involved, the syndrome is called atypical PRESS, which is rare clinical entity. The global incidence of PRES is unknown, but high in patients with eclampsia. PRES is a reversible condition but delay in diagnosis and treatment can lead to cerebral ischemia or haemorrhage leading to permanent neurological damage. Here we report a case of Atypical PRES in eclampsia with successful anaesthetic management with multidisciplinary approach.
Case Report
Antenatally unregistered, 22 year old primigravida with 36 weeks of twin pregnancy was admitted with episodes of 3 convulsions followed by unresponsiveness at home, BP 220/110 mm Hg and Magnesium sulphate 4 gm intravenous (IV) and labetalol was given at private hospital.
Examination
Weight 60 kg, Height 156 cm, afebrile, confused, altered sensorium, Pulse Rate (PR)-100/min, regular. Blood Pressure (BP)-180/104 mmHg. Pedal oedema present. Correction of hypertension was done with IV Labetalol, Magnesium sulphate (4 gm bolus and then 1 gm/hour infusion).
She was posted for emergency caesarean section. Premedication- IV Inj. glycopyrolate 0.2 mg, inj. Ondansetron 4 mg, Inj. Ranitidine 50 mg. General anaesthesia with rapid sequence induction and cricoid pressure was done with Thiopentone sodium 500 mg and succinylcholine 100 mg for intubation, 6.5 mm portex cuffed EndoTracheal Tubes (ETT). Maintenance of anesthesia with O2, N2O, sevoflurane 2% and vecuronium. Inj. Fentanyl 50 mcg IV given after twin delivery. Intraoperatively PR 110-120/min; BP-144/98 mmHg, ECG-WNLSpO2-99%, BSL-160 mg/dl, 1L Ringers lactate, 1 unit of Packed Red Blood Corpuscles, 2 units of Fresh Frozen Plasma given. Blood loss – 1000 ml, Total urine output –350 ml. Healthy twin delivered successfully.
Post operatively: shifted to ICU for controlled mechanical ventilation due to hemodynamic and Central Nervous System (CNS) instability. Metabolic acidosis corrected.
Postoperative day 1: Ventilation continued, PR-110/min, BP-140/100 mmHg, CNS-drowsy, responding to commands, blurring of vision, c/o headache. Investigations were available- Hb-11 gm%, Sr.Creat.1.6 mg/dl, Blood Urea Level-85 mg/dl, Sr. Bilirubin-2.6 mg/dl, Serum Glutamic Oxaloacetic Transaminase (SGOT) 586 IU/L, Serum Glutamic Pyruvic Transaminase (SGPT) 146 IU/L, LDH 320 IU/L, Calcium 11.1 mg/dl, Magnesium 3.7 mg/dl, SE 135/4.5 mili Equivalents, Prothrombin Time/INR-15/1.2. Neurophysician ’ s clinical diagnosis was PRES and advised MRI. Drug Treatment Inj. Mannitol 20 gm, Inj. Lasix 20 mg, Inj. Dexamethasone 8 mg, Tab. Aldomet 500 mg, Tab. Amlo 10 mg.
Postoperative day 2: PR-70/min, BP-140/90 mmHg, Deep Reflexes brisk, Drowsy, obeying, MRI Multiple areas of focal cortical restricted diffusion and subcortical white matter oedema in bilateral parieto-occipital and bilateral frontal region. Venography normal flow in superficial and deep venous sinuses without e/o thrombosis. Diagnosis confirmed of Atypical PRES.
Postoperative day 3: Cardio Vascular System (CVS), CNS, Respiratory System (RS), vitals, Arterial Blood Gas and Investigations–normal. Extubation was done. Patient discharged to ward on 4th postoperative day and to home after 12th day without any neurological deficit.
Discussion
PRES occurs in young middle aged adults; with female preponderance [2,3]. Pathophysiology of PRES focuses two hypotheses. The first, most widely accepted theory rapidly developing hypertension leads to impaired cerebral auto regulation and cerebral hyperperfusion. This leads to extravasation of protein and fluid which produces focal vasogenic oedema [4,5]. The second hypothesis implicates endothelial dysfunction with cerebral hypoperfusion, but this may be relevant with cytotoxic therapy and not in presence of hypertension [3]. Altered cerebral blood perfusion results in blood–brain barrier dysfunction and cerebral vasogenic oedema (Figure 1).
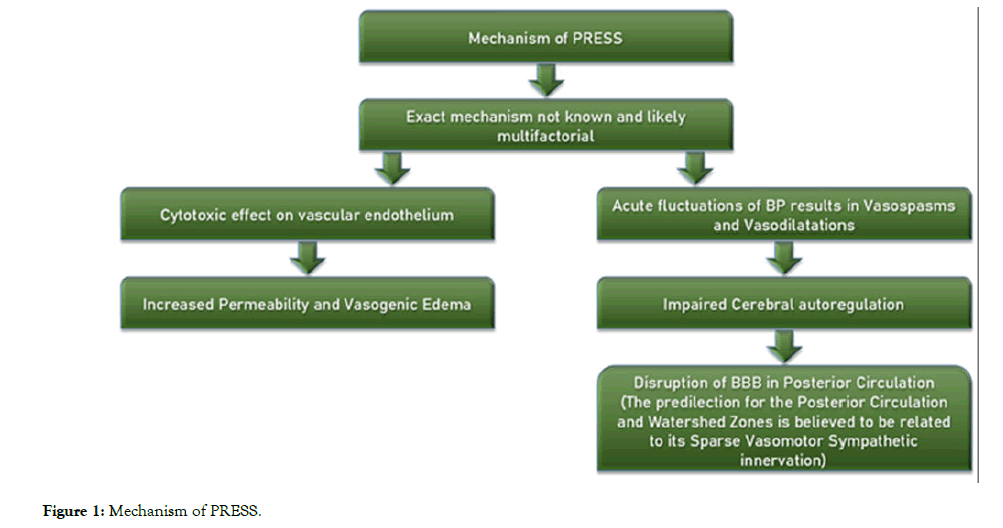
Figure 1. Mechanism of PRESS.
PRES can develop in association with medical conditions including sepsis, autoimmune diseases, high dose chemotherapy, eclampsia, pre-eclampsia and delayed eclampsia (PRES within several weeks after delivery). The length of time taken for symptoms to develop varies from acute onset to several days. Clinical manifestations of PRES vary widely, but typical symptoms include headache, visual disturbances, paresis, nausea and vomiting, impaired consciousness and altered mentation. Generalised seizures are common and may lead to coma. Hypertension is not essential for diagnosis. Cerebral imaging findings vary in symmetrical vasogenic oedema localised to the posterior white matter [6].
There are four radiological patterns of PRES, according to distribution of oedema:
1. Holohemispheric watershed pattern
2. Superior frontal sulcus pattern
3. Dominant parieto-occipital pattern
Partial/asymmetric expression of the primary patterns (Atypical PRES)
The involvement of parieto-occipital regions is more common. MRI is superior to Computed Tomography (CT) for this purpose [3]. CT findings are often normal or non-specific; however, there is some evidence to suggest that repeated CT scanning may be helpful when MRI is unavailable [7] PRES is typically reversible once the underlying cause is removed. Therefore repeated imaging several weeks later is recommended.
Radiological characteristics of PRES
The typical MRI appearance of PRES includes hyper intensities in the parieto-occipital and posterior frontal cortical and subcortical white matter. Most common atypical location involves brain stem and includes abnormalities in midbrain, pons and medulla. Basal ganglia, including thalamus and caudate nucleus, have also been identified as atypical locations [3]. Atypical MRI findings include restricted diffusion on “Diffusion Weighted Images ” (DWI) images, post-gadolinium contrast enhancement on “T1 Weighted” (T1W) images, and haemorrhage [3-5].
PRES can cause a fatal outcome, following cerebral ischemia or haemorrhage. Haemorrhage is becoming more widely recognized as an atypical manifestation of PRES. It appears in 5%-30% of cases. The possible anatomical locations for its occurrence are the brain parenchyma, appearing as a focal hematoma or petechial gyral bleeding.
Management
PRES is reversible. Although there have been reports of only partial resolution or fatal outcome [2,8], the application of an adequate multidisciplinary treatment usually completely resolves it in few days/weeks [5]. The recommended treatment of eclampsia includes delivery of baby and placenta. Treatment for PRES includes Antihypertensive therapy for management of arterial hypertension, use of magnesium sulphate or phenytoin for prevention/control of eclamptic seizures and withdrawal of the offending agent. General measure should focus supportive therapy and must be aimed to maintain ABC of patient. We have followed all these aspects during our case management [9].
Vasodilators (nitroglycerin) can widen cerebral arteries and change the brain blood flow. This may lead to disturbances of auto-regulation. Though, nitroglycerin is established therapy for hypertensive encephalopathy, one should be very careful with its application in cases of PRES which are initially presented as hypertensive encephalopathy, when brain imaging is not available or not typical. The distinction between hypertensive encephalopathy and hypertensive PRES is based on the radiological findings, but is subtle. If neurological symptoms occur or worsen or typical radiological signs appear, nitroglycerin should be stopped.
Conclusions
1. Clinical presentation of PRES is nonspecific, associated with combination of symptoms.
2. It is of particular importance not to exclude PRES as a possible diagnosis when we have clinical presentation which is not accompanied by typical radiological features since this clinical-radiological syndrome can also manifest with atypical MRI findings.
3. The success of the treatment lies in early recognition and resolution of underlying cause.
4. Awareness about this syndrome in practitioners and education for ANC registration in women in developing countries is keystone.
5. Management in tertiary care hospitals can prevent occurrence of any single maternal mortality due to atypical PRES.
REFERENCES
- Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996; 334:494-500.
- Burnett MM, Hess CP, Roberts JP, et al. Presentation of reversible posterior leukoencephalopathy syndrome in patients on calcineurin inhibitors. Clin Neurol Neurosurg. 2010; 112:886-891.
- Legriel S, Pico F, Azoulay E. Understanding posterior reversible encephalopathy syndrome. In: Vincent JL, ed. Annual update in intensive care and emergency medicine. Springer. 2011:631-653.
- Lubarsky SL, Barton JR, Friedman SA, et al. Late postpartum eclampsia revisited. Obstet Gynecol. 1994; 83:502.
- Ehtisham S, Hashmi HA. Posterior reversible encephalopathy syndrome. J Coll Physicians Surg Pak. 2012; 22:398-400.
- Garg RK. Posterior leukoencephalopathy syndrome. Postgrad Med J 2001; 77:24–8.
- Bartynski WS, Boardman JF. Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol. 2007; 28:1320-1327.
- Schwartz RB, Bravo SM, Klufas RA, et al. Cyclosporine neurotoxicity and its relationship to hypertensive encephalopathy: CT and MR findings in 16 cases. AJR Am J Roentgenol. 1995; 165:627-631.
- Pedraza R, Marik PE, Varon J. Posterior reversible encephalopathy syndrome: a review. Crit Care Shock. 2009; 12:135-143.
Citation: Chavan SS, Chavan AM, Gedam P, Pradhan I, Jebaraj S, Chavre P (2019) Atypical Posterior Reversible Encephalopathy Syndrome (PRES) in Eclampsia in Primigravida with Twin Pregnancy: A Case Report. J Surg Anesth 3:2. doi: 10.35248/2684-1606.19.3.125
Copyright: © 2019 Chavan SS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.