Indexed In
- Open J Gate
- Academic Keys
- ResearchBible
- China National Knowledge Infrastructure (CNKI)
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- CABI full text
- Publons
- Geneva Foundation for Medical Education and Research
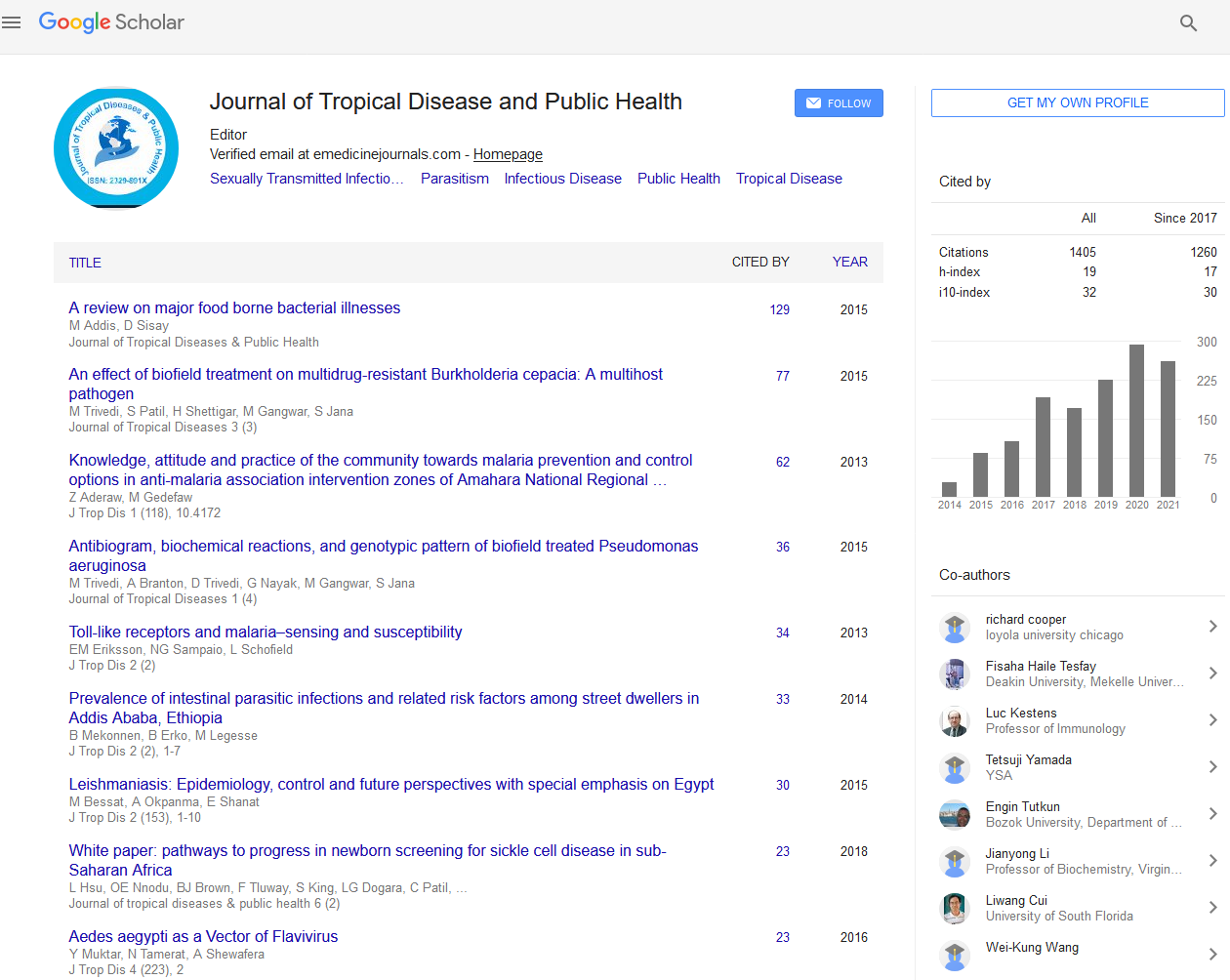
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2019) Volume 7, Issue 6
Assessing the Role of Home-Based Care in Antiretroviral Therapy in Tanzania
Randolph Quaye*Received: 16-Aug-2019 Published: 04-Sep-2019
Abstract
This paper examines the importance of home-based care in delivering ART to people with HIV in Tanzania. While research into self-management of HIV under ART in Africa has focused mostly on adherence to treatment, relatively little has explored the benefits of home-based care as an effective strategy in reaching a targeted population of people with HIV in Dar es Salaam.
A total of 41 respondents were interviewed. Questions detailed treatment-seeking behavior and how best to improve the care the patients receive.
Findings: Majority of respondents see a greater benefit in accessing treatment through home-based care. Several touted cost savings, ease of access, privacy, and less stigmatization as clear benefits over currently clinic-based programs.
The study concludes that home-based programs should be scaled-up because of its feasibility, preferability, and importance of HBC in the dissemination of ART.
Keywords
Home-based care; HIV; Treatment; Tanzania
Introduction
This study examines the complex interrelationship between home-based care, HIV treatment providers, and people with HIV in Tanzania. Specifically, this study explores using Home- Based Care (HBC) as an effective strategy for a sample of residents in Dar es Salaam who are undergoing Anti-Retroviral Therapy (ART).
Research into self-management of HIV under ART in Africa has tended to focus exclusively on adherence to treatment [1]. Relatively little research has focused on how health care providers‘ attitudes and the choices provided by these providers impact self-management by users of health care services. We also explore how these services are internalized by patients and how that affects their self-management [2].
Self-management of long-term illness is a “complex, dynamic, and interactive process, involving practical task, psychological, and social adjustments” [3]. Studies suggest that a patient’s success in chronic-illness self-management addresses three processes: “the work of managing illness needs, by recognizing symptoms, taking treatment, adopting healthier behaviors, making use of resources (e.g. in health systems and social networks), and the more complex process of living with the condition. To assist in this, health care providers can offer specific language, adaptive skills, and practical knowledge that shape how individuals make sense of their environment and living conditions. Informing HIV patients about their rights and helping to empower them will go a long way in encouraging them to develop strategies to access resources and treatment and help them adhere to treatments as responsible patients.
The vision of President George Bush’s United States Presidential Emergency Fund for AIDS Relief (PEPFAR) was to “promote greater global investments and programmatic impact in the fight against AIDS” [4]. Its key objectives were, among others things, to work with partner countries, donor nations, civil society, and people with HIV to effectively mobilize, coordinate, and efficiently utilize resources to expand high–impact strategies to save lives. Further, it was envisaged that this approach would focus on women and girls and end stigma and discrimination against people with HIV by improving access to HIV services [5].
HIV/AIDS situation in Tanzania
Tanzania is chosen for this study because of my familiarity with the health challenges facing the country and the relative success the country has had in reducing the high prevalence of HIV from 14% in the early 1980s to its lowest prevalence rate of 4.5% [6].
Since the first three AIDS cases reported in Tanzania in 1983, the HIV epidemic had spread rapidly to all Tanzanian districts and communities and has affected all sectors of Tanzanian society. In 2003, a total of 18,929 full-blown AIDS cases were reported to the National AIDS Control Program (NACP) from the 21 regions of Tanzania, bringing the cumulative total of reported AIDS cases since the epidemic broke out to 176,102. In 2007 about 2 million Tanzanians were estimated to be infected with HIV and AIDS with approximately 600,000 (30%) in need of ART.
Now Tanzania is facing its most critical health and development crisis to date. The mainland faces a generalized HIV/AIDS epidemic. Of the 38 million Tanzanians, an estimated 1.5 million individuals have HIV; approximately ten percent are children. An estimated 140,000 Tanzanians die each year from AIDS, resulting in disruption of family structures [7]. Recent data based on household surveys estimate the seroprevalence in adults aged 15-49 years in Tanzania to be 7%, with a wide variation across its regions [8] and between genders, with females having a slightly higher rate (7.7%) than males. A recent study by Mmbaga et al. [7] reported that in Dar es Salaam, Tanzania’s largest city with a population of about 4 million, the prevalence of full-blown AIDS is 9.3% against the nation’s average of 5.7%. On the other hand, the city of Zanzibar has a concentrated HIV prevalence of just under 1 percent [7].
There is a much higher prevalence rate of 26% among intravenous drug users [9]. Men who have sex with Men (MSM), the prevalence rates across the African continent is between two to twenty times higher than the general population [7]. Such high prevalence rates can arrest the economic and social development of any country. After all, HIV/AIDS burdens the communities of both poor and affluent. It renders families vulnerable, ends marriages, and leads to a high number of children and adults orphaned or abandoned by those disabled or deceased from the disease or taken from them by others. It can cause “profound disruption to people’s lives and identity” [3].
It is from such a perspective that creating opportunities for HIV victims to find and utilize resources against this scourge is a welcome relief for African and other developing countries of the world. After all, “access to ART providers can significantly improve and prolong the lives of people by creating a setting where HIV people can have access to life-saving ART is the goal of such efforts by PEPFAR and other NGOs [4].
The Care and Treatment Centers (CTC) 2004 and the availability of free ART clinics since 2004 has helped to reduce the spread of the disease. Yet, despite a number of CTCs for AIDS in Tanzania, their numbers are woefully inadequate given the prevalence of infected Tanzanians. Furthermore, for those who have access to such potential treatment centers, far more patients do not attend these centers on a regular basis and a great many of the infected show up at these clinics only at later stages of their disease [10,11]. Recent studies suggest that where these health care services at clinics and/or at home been provided to communities, they have been receptive to using such services [10]. Yet, the evidence suggests that Tanzanians, especially those in urban centers, have not utilized these HIV/ AIDS health services at the level that anyone would like to see [10].
In sum, the number of clients who attend the CTC in Tanzania is still very low. It is estimated that there are about two to three hundred thousand Tanzanians who are already enrolled [7]. There is still a great number of potential clients out there who need to be enrolled but are not. The most relevant question is “why?”
In an attempt to expand the pool of services to HIV victims in Tanzania, we wanted to ascertain whether more HIV-infected individuals, especially those who routinely visit these ART clinics would be inclined to receive ART treatment at home rather than at the clinic. Research by Ahmed S, et al. [10] suggests that rather seeing users of the ART as non-compliance and less likely to adhere to ART, we argue that the users employ complex sets of networks and resources to overcome such barriers to care. After all, as eloquently pointed out by Russell S, et al. [3], “In a setting where providers exert power to control patients. It might create docile patients at ART clinic.” We believe as they do that the dramatic recovery of health on ART… might transform subjectivities and create more empowered HIV patients able to self-manage their condition in a disciplined way” [3].
Methods and Material
This study was conducted in Dar es Salaam, Tanzania’s largest city, which is also one of Tanzanian’s 26 administrative regions. It has the second-highest HIV prevalence in Tanzania’s regions; 9.3% against a national average of 5.7% [7], as already noted. The city is divided into three municipalities: Kinondoni, Ilala, and Temeke. These districts were selected for convenience and also because they have more than 25 health facilities where ART services are provided. Sample of respondents was selected nonrandomly and from those who visited the clinic and are already using ART services. To be eligible for the interview, participants had to have been on ART for a year or more. Those interviewed included farmers, the unemployed, business owners, and those in other economic enterprises in the informal market economy. A total of 41 respondents were interviewed. Following a structured questionnaire prepared and provided by the author, the interviews were conducted face-to-face by two undergraduate students from the University of Dar es Salaam at the health clinics and private locations like homes and offices to ensure confidentiality for respondents. The interview questions were translated into Swahili by the interviewers and the results transcribed and translated back into English by them. The interview questions were grouped under five headings: demographic information about respondents, namely, their age, gender, occupation. education, and whether they preferred home-based care or continued treatment at the ART clinic, and then what they perceived to be the benefits or drawbacks for using either treatment options; detailed treatment-seeking behavior and how best to improve the care provided to patients and to assess the impact of such treatment options on confidentiality and stigmatization of the patient’s health condition, as well as challenges and solutions envisaged for such programs.
Ethical considerations
Approval for this study was obtained from The Tanzanian Commission of Science and Technology (COSTECH), under their guidelines for its ethical conduct. Both written and verbal consent was obtained from all participants. Participants were informed of the voluntary nature of their participation and told that they could stop the interview at any time if they felt uncomfortable or unwilling to continue. All participants were offered transportation costs and bottles of soda. They were also encouraged to adhere to their ART regimen and to report any changes in their condition to the clinics of their choice.
Results
Distribution of sociodemographic characteristics of respondents are described in Table 1 (Age, Gender, Occupation, Education level, and Choice of Treatment).
| Criteria | Number | % | |
|---|---|---|---|
| Age | 28-38 | 25 | 49 |
| 39-50 | 15 | 37 | |
| 51-70 | 5 | 12 | |
| 71-84 | 1 | 2 | |
| Total | 41 | 100 | |
| Gender | Male | 13 | 32 |
| Female | 28 | 68 | |
| Total | 41 | 100 | |
| Occupation | Small business | 26 | 63 |
| Employee | 7 | 17 | |
| Unemployed | 8 | 20 | |
| Total | 48 | 100 | |
| Education level | No formal education | 14 | 34 |
| Primary education | 15 | 37 | |
| Secondary | 12 | 29 | |
| Total | 41 | 100 | |
| Choice of Treatment | Home-based care | 25 | 61 |
| Health facility | 16 | 39 | |
| Total | 41 | 100 |
Table 1: Distribution of sociodemographic characteristics of respondents (n=41).
Views of patients choosing home-based care
The majority of participants (61%) interviewed expressed the desire to use and have used home care treatment. A 45-year-old female patient responded to the question, “What are your opinions about ART home delivery program?”
Stating: First of all, it is good since he/she (HBC staff) may come here and you may just direct him/her to bring them (medications) to my house. In the beginning, I thought that this is not effective but later I asked myself some questions and realized that it is effective. When you (HBC staff) come to my home, you measure our body weight and do the blood check-up. It may happen that one day you forget your clinic date and miss it. So according to this program, someone will bring you your ART at home, though I am asking myself can we get the same health education at home that we will get at the clinic?
Adherence to ART
Seventy-five percent of the respondents clearly demonstrated their adherence to the ART regimen. From their responses, a high level of adherence was mentioned by the respondents. For example, in another discussion, a 56-year-old female asserted that: Those on HBC will maintain good adherence to their therapy since they will not feel shy (as they might) about coming to the facility because they will be receiving their ART secretly at home, and when their ARTs are finished, the HBC staff will just call them and ask, “Are you home, eh ? I am coming there to bring your medication, and you just reply, “Yes, I am at home, you will find me here.”
Another benefit mentioned by patients included that staff members provide very detailed information about the program, and the required regimen for the medications provided. Though health care providers were viewed as having a monopoly over knowledge with treatment management, yet the participants felt they were respected and that their concerns were addressed with such visits. As one respondent asserted, “ I get more education because there are issues which I have not thought of, but when they visit me at home, they teach me many things.” Others mentioned that the program (HBC) improves the health conditions of the patient as the patient becomes close to HBC providers, so even if he/she has a problem, it is easier to explain to him/her.
A point made by one of the respondents is that HBC staff needs to be better trained and equipped with the professional tools and habits to be sensitive to the needs of their clients. One respondent declared that “They (HBC staff) should be competent and provide quality services in order to enroll more people in this program.”
Furthermore, as another respondent put it, “Those people who are responsible for providing this home-based care should be kind and volunteer their services) to make home-care visits instead of working only from the health care centers.” Another respondent mentioned the importance of HBC staff maintaining their sensitivity to patients’ situation by avoiding stigmatizing the patients by suggesting that, ”HBC staffs should try to be good as much as they can, and should avoid using words which can stigmatize the patients so that they can be motivated to stay in the program.”
Convenience
Half of the respondents mentioned the ease with which they are able to access the ART drugs delivered to their home rather than going to the clinic as this is more convenient and less costly and saves time. From the perspective of a 51-year-old female who gets her ART through Home-Based Care (HBC), “This scheme is very good as it will help both HBC and the patients as they will not have to come to the clinic frequently since medicine will be delivered to their homes.” She argued further that they will receive treatment on time because even the busy patients who cannot go to the clinic will have their medications easily available. So in her opinion, it is a good thing. A 48-year-old man echoed the same sentiment: I thank those who initiated this project of delivering medicine at home. They have done a great thing. This approach will also save time and money. For example, in accessing the medications, all I will need to do is to inform you by phone that the medicines are finished and you ask, “where are you?” I am home. The service provider comes and hands me the parcel (of medications). Don’t you see that I have saved money and time?
From the perspective of an 83-year-old male on HBC
First, it reduces problems from visiting the clinic regularly. Therefore on your clinic date, the health provider visits you at home and brings you your medicine because she/he also knows your clinic date and therefore she/he visits the clinic and picks up your medicines and brings them to you. This reduces the congestion of people at the hospital. The program saves money because the bus fare I use from my home to the clinic will be better spent on other expenses of my health care.
A 32-year-old female patient, when asked to comment on her use of HBC argued that: The HBC is good because when we come to the hospital you find it overcrowded with many patients. As a result, we go home late, for you may come to the clinic eight hours ahead but sometimes you may still stay until one o’clock in the afternoon without going back home so you do your things at home late.
A respondent already quoted on HBC staff’s avoiding stigmatizing patients also added that I can say that for example, if many patients opt for home-based services, it will mean that there will be fewer people receiving facility-based services so it will minimize the crowd here at the facility and among other things, improve the quality of services one receives. After all, it will be a great advantage because when there are lots of patients coming to the facility to take ARTs you get the services late. So if there are fewer people, it will be better since you can even ask for permission (to be excused) from your job and you can just come and pick up your ART quickly, but when there are many patients, it can take hours. This is a real problem, but with the introduction of this program (HBC), it will be an advantage having fewer patients at the clinic since a patient can go and pick up his/her ART quickly.
In a nutshell, the use of HBC reduces the population at the facility and at the same time allow time for individuals’ work at home.
Confidentiality
Another point raised by some of the respondents is the lack of privacy and confidentiality associated with ART clinic visits as compared to at-home or at-work visits by HBC staff.
As one respondent puts it, “The ART home delivery program is very confidential because the only people who know about my health status are the health provider and me. Therefore we know how to talk confidently because of the secret that we share and hence we can avoid many possibilities for other people to discover the reasons for her/his visit.”
Another respondent described the privacy-maintaining methods of the HBC staff: Nowadays, when the HBC staff comes, we meet in my room so no one can discover what is going on because sometimes when she brings ARTs, she carries some oranges with it and when she arrives she just calls me, “Mom, I have brought some oranges for you. Next time, I will bring you vegetables” So when the neighbors hear that they believe she is my daughter and they are not aware of what is going on.
The respondent who wanted HBC staff to be “kind” also wanted them: To consider the situation of the people they are serving ,because you may find a person brings ARTs to you in a way that even the more distantly related neighbors and those living in more distant parts of a compound will realize that in your household there is an HIV patient. Thus the HBC staff should be trained to know what kind of words they should use and the type of clothing they should appear in when providing this care.
Further she states: With HBC we will not be meeting at the facility where we can be seen and known that each one there is taking ART because many times when we meet at the facility some people discuss about others and sometimes when they go back to the street they tell others that they have seen you taking ART at the facility. However, if you take your ART at your own place no one will see you or know.
On the question, what else do you like about the HBC, she responded by saying that, The other thing I like about HBC is that I do not have to worry because if I were to go to the clinic, I may find someone who knows me. Some other people when they come to the clinic they always feel worried because there are other people who when they see others in the facility they go and tell others in the street that they have seen a certain person taking ART at the facility.
The 56-year-old woman said, “My opinions are not negative about (HBC) because when you go to the clinic (instead) you are likely to meet someone who may know about your HIV status.”
The 48-year-old male responded when asked about his opinions about the HBC alternative, “It is very good because you know others are known in places like this, then coming to show up your face is not good.”
Another responded to the question as to whether HBC improves the health conditions of the patients stated that, This scheme improves people’s health. For example, when staff members bring medicine to us and find us with a particular problem, it becomes simpler because there are referrals and when we need a referral, we are likely to get it so I think it is a good thing.
Patients choosing to go to a health facility
About one-third of the respondents opted to continue treatment at health facilities. They expressed a number of reasons for this preference.
Effectiveness: One respondent stated that she preferred facility based care because she gets good service. She followed that by stating that, “ If it happens that I am sick, say, maybe I have a fever and HBC brings me my medicines, how can he /she explain my condition (?) So it is better to go to see the doctor at the health facility because I can explain to him/her if I have gotten skin diseases. It will be easy for me to tell the doctor since the doctor knows what to advise me.”
Convenience: A respondent declared that I personally chose it because if I had my own place it would be better, but since I work in a company, I chose this option (of visiting the health facility). There is a gate (at work), there are guards, and if you (HBC) staff members come, I will be told I have visitors. I find that to be a bit of a nuisance. That is why I said it is better for me to keep going to the hospital. If I am able to own my own place, then I will be comfortable having staff come to my house.
A 35-year-old female stated, “I prefer the normal protocol (of visiting the health facility) because of my work schedule, and thus waiting for medicines to be delivered to me at home is impractical.”
Confidentiality: Two-thirds of the respondents mentioned the likelihood that their HIV status might be known by other family members or co-workers or friends if they were visited at home by HBC workers. As one puts it, “Having someone come to my house every month to bring me medicine might raise suspicion among my neighbors as to why that person comes every month and wonder what that person is delivering.”
A 33-year-old female in response to the same question responded that “I live with a man who is very harsh and if he realizes that I am HIV positive, he may use any means to kill me. Thus, when my partner goes to work, I just come to the clinic to pick up my ARTs and go back home without him being aware of it.”
Patient adherence to the program
As to whether HBC might compromise patients’ adherence to their medication regimen, overwhelmingly our respondents said “No.” As one respondent puts it: Personally, I can say that the provision of medication at home cannot affect my adherence to the medications because I follow my timetable and the procedures agreed upon when I started at the clinic. Therefore there is no effect on how I use the medications.
Patient stigmatization: David Cort and Hsin Tu [11] define HIV stigma “As an ideology, set of beliefs, or discourse which suggests that people with HIV are different from others in “normal society” Cort and Tu argue using the Demographic and Health (DHS) and World Bank Group data contend that “stigmatizers in general populations are less likely to practice protective sexual behaviors and this negative relationship is strongest in Southern Africa, where HIV prevalence is highest.”
One cannot be sure how such stigmatizing will affect the decision to use either HBC or health facility care. In this study, the evidence was not conclusive. More than eighty percent of respondents stated that their choice of care has a little direct bearing on how they are perceived, as they believed that the way both programs are structured guaranteed at the very minimum, their confidentiality and that the patients’ status was less likely to be revealed through these approaches. As already reported here, one respondent puts it, “The ART home delivery will not lead to anyone finding out about my HIV status as no one can find out except me and the HBC staff.”
As eloquently put by another respondent, “I prefer the home delivery program because it has helped me to hide my health status and no one can realize it. But previously, there was no privacy since we used to get the service in an open space to the extent that we were feeling very shy.” As another puts it, “What is great about HBC is that it has helped me to avoid the stigma I used to experience when I came to the facility.” Majority of the respondents mentioned that HBC will help reduce the stigma associated with the disease.
Challenges: One recurring theme mentioned by a majority of respondents was the need for HIV sufferers’ greater sensitization to the benefits of HBC as an effective way of reaching the broader community. Some patients decried the fact that some HBC staff are not adequately trained and require more training than the 10 to 14 days training program provided. HBC staff members, too, mentioned their need to have regular training and knowledge about the HIV medications, their side effects, and the proper protocol to follow when dealing with patients who might not be adhering to the treatment regimen.
They also mentioned the need for the program to provide income-generating activities for their clients. More than half of the patient respondents were thankful for the program in providing them with seeds for cultivation and also providing proper nutritional programs as part of the program. As one respondent puts it, “ There are so many people here in the village who have a very difficult life and from time to time they tell you that they have taken their medications but they have nothing to eat, so giving them even petty cash will at least motivate them a lot.”
Another issue raised by respondents is the way HBC staff carry their weighing scale to their appointments at patients’ homes. Some of the respondents were of the opinion they themselves have to be careful not to let the staff’s carrying of a scale expose the patients to the potential that others may learn about their HIV status. A few of the respondents also mentioned that HBC staff when visiting homes should bring along other medications like anti-malaria tablets and urine-tract testing equipment because some of the clients have stayed at home for three months or so without visiting the hospital as some may not have the money to pay for bus fare or clinic user fees.
Providers were also encouraged by respondents to be more sensitive to the health needs of their patients and to provide very detailed information when needed. Some also decried the negative attitudes of nurses at their health facility.
One respondent asserted: For the nurses, I would like all the nurses to have mercy because sometimes they are harsh and respond harshly. For example, when you cough, they tell you ‘akhara’, I did not infect you.” Another stated, “I was coughing at the time the nurse was attending to me, She said, ‘don’t cough at me. ‘But I did not infect you. ‘ In fact, it pained me so much for her to criticize me. ”
On the question of what difficulties respondents face in accessing care, one replied that Some patients are fearful that their status will be revealed, while they know that if they come to the dispensary their secret will stay between them and the doctor. Furthermore, we face challenges in taking the medicines them as we normally take without food when and end up not having the energy to farm or go to work. We face this challenge frequently.
About 9 percent of respondents when asked to reflect on the services provided stated that, some of them (patients) like this scheme but only a few do not because they thought that using this service will reveal their HIV status. Those who agree think that this scheme makes it easy for them because of the places they live in. For example, there is a dispensary in Buza and on Fifth street. From the street of Machine ya Maji, you have to take a motorcycle to get to the dispensary which cost 2000tz ($1) so they feel HBC eases their lives.
Others called for more available treatment centers and more HBC staff members with requisite training.
Discussion and Conclusion
This paper has examined the potential benefit of using ART home-based care as an alternative to the use of health center services as a way of reaching people with HIV. Our findings suggest that a large majority of respondents believe that such an approach offers a way out of the current long queues and cost associated with seeking care from designated ART clinics. Among the strongest points raised for the support of this program is that it guarantees at the very minimum, the expected patient treatment, safety, and confidentiality. It also has a positive income effect on families since they save not only time but money with HBC visiting them at home. None of the respondents suggested that this new treatment approach has affected their ability to adhere to their treatment regimen. In fact, overwhelmingly, they contend that home-based care has allowed them to better manage their care as they can always count on a regular supply of ART and also can still be counseled during the visit by the BHC staff.
The minority of respondents who were opposed to HBC visits raised concerns about their privacy and the fear that their HIV status would be known at home. They, therefore, preferred facility-based care. As reported by Russell et al. [3], “Given the burden of HIV in Sub-Saharan Africa, and the need for lifelong motivation to sustain ART adherence, there remains a need to expand low-cost interventions that encourage people living with HIV to talk, learn and re-conceptualize the disease.” I could not have agreed more.
The sample for this study is non-random sample in that all of them have tested HIV positive and were receiving care from a specific health facility’s staff at home or at the clinic. The small and geographically limited sample size makes generalizations to the entire HIV/AIDS population worldwide, in Africa, Tanzania, or even Dar es Salaam difficult. What is clear, though, is that the city’s HBC is an innovative approach to bringing care to those whose circumstances and financial status have rendered them less capable of using the well-established ART health facilities. It was also observed that a positive patient-staff relationship is critical to effective self-management of care. Having HBC staffs recognized as respectable members of the community they serve may go a long way to improve acceptance of the services they provide. They are in a sense the gateway to services so urgently needed by individuals dealing with the management of their HIV health care.
As observed by Russell et al. [3], “The harsh economic and social circumstances faced by many patients (has) mediated their self-management strategies in fashioning of their therapeutic citizenship.” This was observed to be the case among the sample interviewed.
By all indications, this pilot study was informative and illustrative of what should be done in order to scale up these services to other regions in Tanzania. As we better understand the role of HBC in addressing the needs of people with HIV/ AIDS, the Tanzanian (Dar es Salaam) experience may provide a window into how to successfully expand HBC in HIV health care.
Acknowledgment
The author is grateful to all the study participants for sharing their experiences with the research team. I am indebted to J. Mori and L. Mohammed for their work in spending countless hours interviewing the participants and also translating the interview questions and interview responses from Swahili to English. My sincere thanks go to COSTECH, Illala Municipal Medical Officer of Health and Illala Municipal Council for approving the study. Grant support came from the Ohio Wesleyan University TEW Presidential Discretionary Fund.
Declaration of Conflicting Interests
The author declares no conflict of interest with respect to the research, authorship, and publication of this paper.
REFERENCES
- Martin F, Kawuma R, Zalwango F, Seeley S. Tasks and strategies of self-management of living with anti-retroviral therapy in Uganda. AIDS Patient Care STDs. 2013;27:697-706.
- Allen C, Mbonye M, Seeley J, Birungi J, Wolff B, Coutinho A, et al. ABC for people with HIV: Responses to sexual behavior recommendations among people receiving antiretroviral therapy in Jinja, Uganda. Culture Health Sexuality. 2011;13:529-543.
- Russell S, Zalwango F, Seeley J. The framing and fashioning of therapeutic citizenship among people living with HIV taking antiretroviral therapy in Uganda. Qual Health Res. 2015;1:1-12.
- UNAIDS. Report on the Global AIDS Epidemic July 2004, Geneva. 2004.
- Blandine B, Marc E. Gender asymmetry in healthcare-facility attendance of people living with HIV/AIDS in Burkina Faso. Social Sci Med. 2009;2:1212-1234.
- United Republic of Tanzania. Health sector strategic plan (HSSP IV) July 2015-June 2020. Ministry of Health and Social Welfare, Dar es Salaam. 2015.
- Mmbaga E, Dodo M, Leyna H, MoenK, Leshabari M. Sexual practices and perceived susceptibility to HIV infection among men who have sex with men in Dar es Salaam, Mainland Tanzania. AIDS Clin Res. 2012;S1-012.
- National AIDS Control Program. Tanzania HIV/AIDS and Malaria indicator survey calverton, Maryland. 2008.
- Ministry of Health and Social Welfare. Health sector reform the United Republic of Tanzania, Dar Es Salaam. 2008.
- Ahmed S, Autrey J, Katz IT, Fox MP, Rosen S, Onoya D, et al. Why do people living with HIV not initiate treatment? A systematic review of qualitative evidence from low- and middle-income countries. Social Sci Med. 2018;213:72-84.
- Cort D, Tu Hsin. Safety in stigmatizing? Instrumental stigma beliefs and protective sexual behavior in Sub-Saharan Africa. Social Sci Med. 2018;197:144-152.
Citation: Quaye R (2019) Assessing the Role of Home-Based Care in Antiretroviral Therapy in Tanzania. J Trop Dis. 7:334. doi: 10.35248/2329-891X.19.7.334
Copyright: © 2019 Quaye R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.