Indexed In
- Open J Gate
- JournalTOCs
- The Global Impact Factor (GIF)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
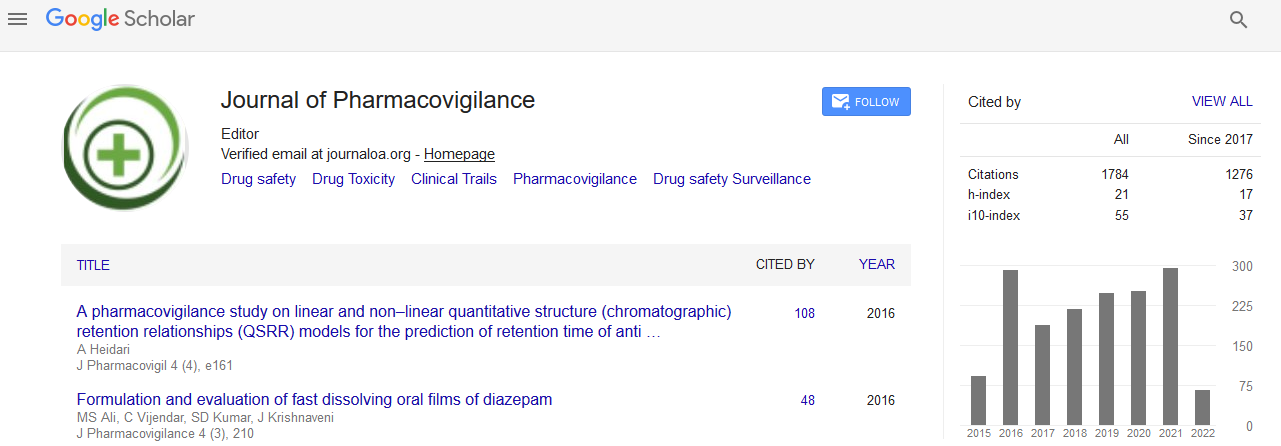
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Case Report - (2021) Volume 9, Issue 9
Amoxicillin /Clavulanic Acid Induced Mixed Hepatocellular-Cholestatic Hepatic Injury- A Rare Case Report
Shreshth Khanna, Vandana Tayal* and Vandana RoyReceived: 06-Sep-2021 Published: 27-Sep-2021
Abstract
Amoxicillin is an extended spectrum acid stable bactericidal beta-lactam antibiotic, commonly used in the treatment and prophylaxis of gram positive and negative bacterial infections. Clavulanic acid, a beta-lactamase inhibitor that is often used in conjunction with amoxicillin (co-amoxiclav) prevents the hydrolysis and re-establishes amoxicillin's activity that binds irreversibly to the catalytic site of susceptible beta-lactamases and has good activity against beta-lactamase producing streptococci, staphylococci, Klebsiella pneumonia, H. influenzae and penicillinase-producing anaerobes and is most commonly used for upper respiratory infections, otitis media and sinusitis to broaden its spectrum further and combat resistance. Commonly reported adverse effects of co-amoxiclav include nausea, vomiting, headache, abdominal pain, skin rashes and oral thrush. Few rare and serious adverse drug reactions associated with its use include anaphylaxis, angioedema, hemolytic anemia, drug rash with eosinophilia and systemic symptoms (DRESS Syndrome), multi-organ dysfunctions, seizures and hepatobiliary injury.
Introduction
Amoxicillin is an extended spectrum acid stable bactericidal betalactam antibiotic, commonly used in the treatment and prophylaxis of gram positive and negative bacterial infections [1].
Clavulanic acid, a beta-lactamase inhibitor that is often used in conjunction with amoxicillin (co-amoxiclav) prevents the hydrolysis and reestablishes amoxicillin's activity that binds irreversibly to the catalytic site of susceptible beta-lactamases and has good activity against beta-lactamase producing streptococci, staphylococci, Klebsiella pneumonia, H. influenzae and penicillinase-producing anaerobes and is most commonly used for upper respiratory infections, otitis media and sinusitis to broaden its spectrum further and combat resistance [2].
Commonly reported adverse effects of co-amoxiclav include nausea, vomiting, headache, abdominal pain, skin rashes and oral thrush. Few rare and serious adverse drug reactions associated with its use include anaphylaxis, angioedema, hemolytic anemia, drug rash with eosinophilia and systemic symptoms (DRESS Syndrome), multi-organ dysfunctions, seizures and hepatobiliary injury [3].
Case
We report a case of a 23 year old female who presented to the dental OPD with complaints of fever (documented 99.8F) and swelling of the jaw on the right side of the face since 1 day. Her history revealed that she also had mild jaw pain, on and off since the last 2 weeks for which she took Laung (Clove) at her home and had temporary relief. After examination, her dentist planned a 3rd molar tooth extraction procedure. After the procedure, she was prescribed tablet amoxicillin-clavulanate (500 mg/125 mg) for a period of 10 days to be taken thrice daily to prevent post-operative infection and tablet flurbiprofen 100 mg for pain to be taken on as and when required basis.
During the course of her antibiotic therapy, she felt nauseous, for which she used to take Ajwain (Carom seeds) and recovered. Within 4 days of the completion of the co-amoxiclav course, she started to experience a decrease in her appetite, accompanied with abdominal pain, nausea, 2-3 episodes of vomiting and passage of dark yellow colored urine. Her family also noticed increased somnolence, agitation and confusion in her behavior for which she was brought to the hospital OPD for check-up. On examination, the physician noticed yellowish discoloration of the scleral conjuctiva, upper limbs and the skin showed markings from pruritus. Abdominal examination was normal without any signs of hepatosplenomegaly.
Laboratory tests revealed increased liver transaminases, alkaline phosphatase and total bilirubin (Table 1). Serological screening tests for acute viral hepatitis (hepatitis virus (Subtype A, B, C, E) were negative, cytomegalo-virus (CMV) and Epstein Barr virus (EBV)) were also negative. Ultrasound abdomen revealed biliary tract inflammation. Liver histology showed central lobular retention of bile with mixed infiltrates of lymphocytes, neutrophils and eosinophils in portal areas and in areas of focal spotty necrosis in the liver parenchyma.
| Time after completion of amoxicillin-clavulanate treatment regimen | Aspartate Aminotransaminase (AST) (U/L) | Alanine Aminotransferase (ALT) (U/L) | Alkaline Phosphatase (ALP) (U/L) | Bilirubin (mg/dL) |
|---|---|---|---|---|
| On admission | 554 | 531 | 290 | 12.5 |
| 4 Weeks | 258 | 284 | 376 | 8.4 |
| 8 Weeks | 178 | 175 | 112 | 1.8 |
| 12 Weeks | 76 | 93 | 105 | 1.1 |
| 16 Weeks | 29 | 37 | 92 | 0.9 |
| Normal Values | <40 | <42 | <115 | <1.2 |
Table 1: Liver function Tests at baseline visit and 12 weeks after discharge.
Other than tablet amoxicillin-clavulanate there was no history of consumption of any other long term allopathic/herbal or homeopathic medications, alcohol consumption, smoking or any substance abuse. There was no family history of acute or chronic liver disease, or any other long term illness.
The patient was diagnosed as a case of moderate-severe amoxicillinclavulanate induced liver injury.
The patient was admitted and was provided with supportive care and hydration with IV fluids. Patient improved after 5 days of hospital management and was discharged after 7 days on cholestyramine 4 grams twice daily and was advised follow-up on a monthly basis. Liver function tests (LFT) were repeated at each follow-up visit, which showed a steady decline (Table 1)
After 4 months of discharge, her symptoms had completely resolved and the LFT levels had returned to normal.
Roussel Uclaf Causality Assessment Method (RUCAM) or its previous synonym Council for International Organizations of Medical Sciences (CIOMS) scale is used to establish causality in cases of idiosyncratic Drug Induced Liver Injury (DILI) [4]. The total score was 6 on the scale in this case. Thereby, determining the association as probable between amoxicillin-clavulanate use and liver injury. The causality assessment of the adverse drug reaction came out to be probable using the Naranjo Causality Assessment Scale [5]. The case was then reported to the ADR monitoring center under the Pharmacovigilance program of India (PvPI).
The idiosyncratic DILI can also be sub-classified according to the R ratio [6]. The ratio is typically ≥ 5 in hepatocellular injury, < 2 in cholestatic liver injury and between 2 and 5 in mixed hepatocellular/cholestatic liver injury. In this case the R ratio was calculated to be 5.
Discussion
Amoxicillin-clavulanate is one of the most prescribed antimicrobial agents (41% of total antibiotics use) and is among the most prescribed drugs in both adults and pediatric patients. Increase in the prescriptions of amoxicillin-clavulanate from 7.3 Defined Daily Doses (DDD) in 2007 to 9.4 DDD in 2015 has been observed, whereas in the same time frame amoxicillin use has decreased from 3.9 to 2.1 [7].
DILI is a rare entity with an estimated annual incidence between 10 and 15 per 100,000 persons exposed to prescription medications [8].
There is no gold standard laboratory or diagnostic test for drug induced liver injury. One of the scoring systems is RUCAM (CIOMS) scale, which classifies DILI based on the alterations in the levels of ALT, AST, ALP and the ratio of ALT/ALP into hepatocellular, cholestatic or mixed hepatocellular-cholestatic type. The scale takes into account numerous risk factors (time of onset of event, time from drug intake until reaction onset, course of ALT after drug cessation, age, alcohol consumption, previous hepatotoxicity of the drug, underlying diseases, alternative causes, response to unintentional re-exposure and concomitant use of drugs etc.) to link the association of drug use with hepatotoxicity [9]. In this case, the total score was calculated to be 6 on the RUCAM/CIOMS scale, suggesting a probable association of the drug use with hepatotoxicity.
Amoxicillin-clavulanate induced liver injury can present with all the three patterns of DILI [10].
In this case, the ALT and the ALP were raised ≥3 times & ≥2 times the upper normal limit respectively and the ALT/ALP ratio was calculated to be 5. This pattern of alteration in liver enzymes according to the RUCAM/CIOMS criteria as well as history and the histological findings in the absence of any other cause of liver injury are suggestive of mixed pattern of amoxicillin-clavulanate induced hepatocellular-cholestatic liver injury (Table 1). A mixed hepatocellular and cholestatic injury is seen with many drugs and is most characteristic of DILI as was also observed in this patient; in the mixed pattern of DILI, liver biopsy generally shows the presence of hepatocyte injury, lobular disarray, lobular inflammation which is usually accompanied by biliary stasis [11].
The incidence and risk of co-amoxiclav induced liver injury is very low, hence there’s a scarcity of literature for the same. The exact mechanism of co-amoxiclav induced hepatitis remains obscure, but the frequent association with hypersensitivity reactions (i.e. skin rash, hypereosinophilia, anti-tissue antibodies) are suggestive of auto-immune-allergic idiosyncratic response to the drug. However, the available literature also highlights a probable association of genetics to co-amoxiclav induced liver injury in population with high risk HLA alleles [12].
The hepatic injury appears to be due to the clavulanate component of the combination, as re-exposure to amoxicillin alone has rarely been associated with idiosyncratic liver injury [13]. Moreover, the amoxicillin component of the drug is primarily excreted by renal system, whereas clavulanic acid is excreted by both the kidney and liver.
Similar findings have also been observed from the Italian spontaneous reporting system database which highlighted that co-amoxiclav use was associated with a much higher frequency of liver injuries compared with amoxicillin alone. Hepatotoxicity usually follows a temporal association and generally occurs upto 8 weeks after consumption of the antibiotic. Increase in the levels of transaminases within a week of consumption of amoxicillinclavulanate was observed in this case also.
Amoxicillin-clavulanic acid induced hepatotoxicity usually follows a benign course and has a good prognosis, although there have been incidences of fulminant hepatitis associated with its use [13]. DILI is a usually diagnosed after exclusion of all the other causes of liver injury. Once the drug is identified, the patient should not be prescribed the same drug again, as the re-introduction of the drug can result in recurrence of the problem. A detailed history of all the other medications taken before the onset of symptoms is fundamental in eliminating the other causes of liver injury and delineating as a case of DILI. Recognition and removal of the offending medication and symptomatic management is the cornerstone in the treatment.
This case report highlights the association of amoxicillin-clavulanate with hepatic injury. Hence, there is a need of monitoring especially in predisposed individuals for early recognition of the hepatic injury. In view of widespread use of amoxicillin-clavulanate combination in the recent years it thus becomes imperative to take into consideration the various risk factors before prescribing.
REFERENCES
- Akhavan B, Khanna N, Vijhani P. Amoxicillin. Ncbi.nlm.nih.gov. 2021
- Bucher HC, Tschudi P, Young J, Périat P, Welge-Lüussen A, Züst H, et al. Basel Sinusitis Study Investigators. Effect of amoxicillin-clavulanate in clinically diagnosed acute rhinosinusitis: a placebo-controlled, double-blind, randomized trial in general practice. Arch Intern Med. 2003 125;163(15):1793-1798.
- Sharifzadeh S. Antibacterial antibiotic-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: a literature review. Eur J Clin Pharma. 2021; 77:275–289.
- Danan G, Benichou CJ. Causality assessment of adverse reactions to drugs--I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. Clin Epidemiol. 1993; 46(11):1323-30.
- Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharacol Ther. 1981; 30:239–45.
- Aithal GP, Watkins PB, Andrade RJ, Larrey D, Molokhia M, Takikawa H, et al. Case definition and phenotype standardization in drug-induced liver injury. Clin Pharmacol Ther 2011; 89:806–815.
- Kaur A, Bhagat R, Kaur N, et al. A study of antibiotic prescription pattern in patients referred to tertiary care center in Northern India. Ther Adv Infect Dis. 2018; 5(4):63-68.
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson. Incidence, presentation, and outcomes in patients with drug-induced liver injury in the general population of Iceland Gastroenterology. 2013; 144(7):1419.
- Bethesda. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury: National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Amoxicillin-Clavulanate.
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterol. 2015; 148:1340–52-57.
- Lucena MI, Molokhia M, Shen Y, Urban TJ. Spanish DILI Registry; Eudragene; Dilin; Diligen; International SAEC. Susceptibility to amoxicillin-clavulanate-induced liver injury is influenced by multiple HLA class I and II alleles. Gastroentero. 2011; 141(1):338-347.
- Donati M, Motola D, Leone R, Moretti U, Stoppa G, Arzenton E et al. Liver Injury due to Amoxicillin vs. Amoxicillin/Clavulanate: A Subgroup Analysis of a Drug-Induced Liver Injury Case-Control Study in Italy. J Hepat Gastroin Disor. 2017;03(01).
- Fontana RJ, Shakil AO, Greenson JK, Boyd I, Lee WM. Dig Dis Sci. 2005; 50(10):1785-1790.
Citation: Khanna S, Tayal V, Roy V. (2021) Amoxicillin /Clavulanic Acid Induced Mixed Hepatocellular-Cholestatic Hepatic Injury- A Rare Case Report J Pharamacovigil 9:334. doi-10.35248/2329-6887.21.9.334.
Copyright: © 2021 Tayal V. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.