PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
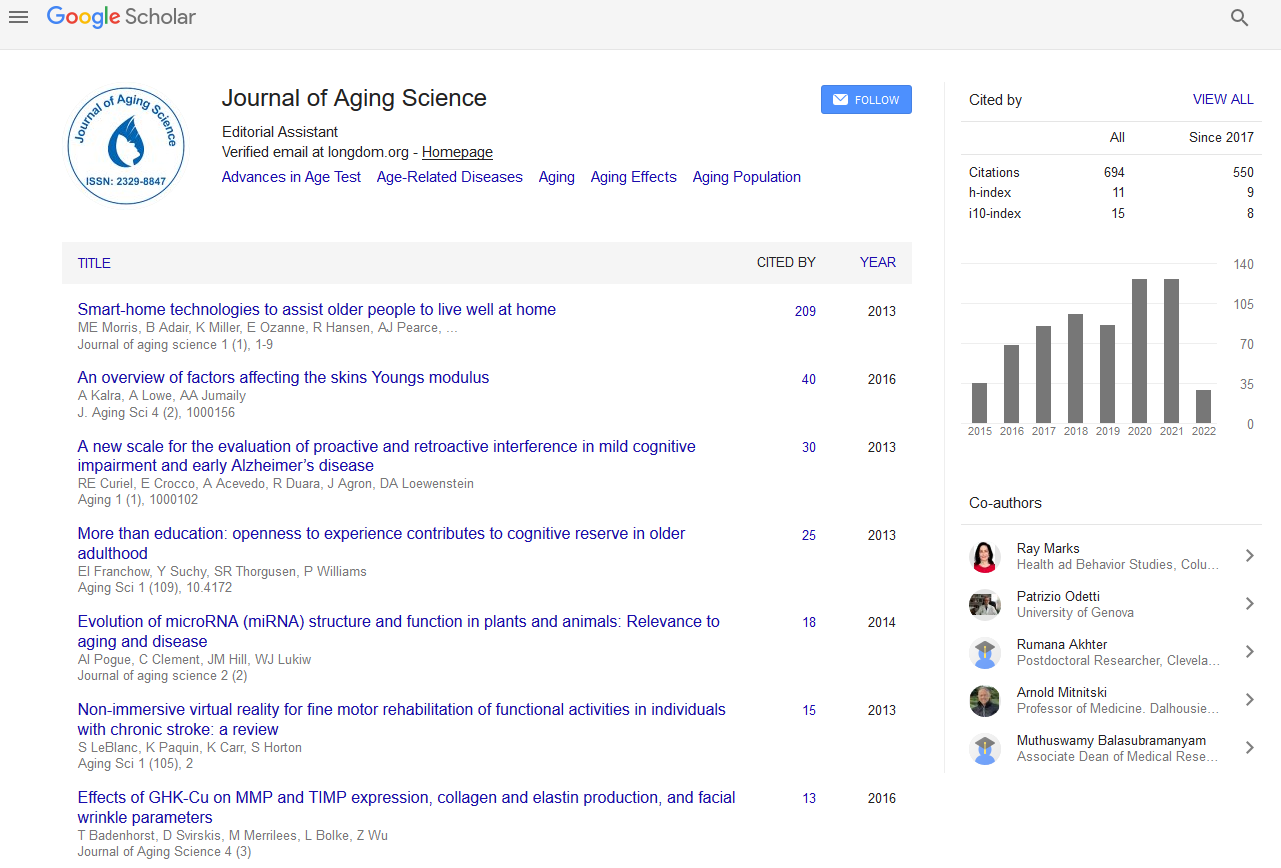
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Review - (2019) Volume 7, Issue 3
Adapting to Dying and Bereavement of Geriatric Palliative Care
Mohammed Abduh Al-Shaqi*Received: 20-Sep-2019 Published: 11-Oct-2019
Abstract
Palliative care has recognized the power of suffering of life threatening illness and is concerned with helping people to cope and adapt with these chronic illness. Our fear of death and the loss of a loved one are two of the most monumental emotional challenges of human existence and suffering. This is incorporated into a philosophy of care that has resulted in the principles of palliative care. This anxiety is usually suppressed and is only exposed when the reality of a possible death is confronted. Fear of death stems from different sources, for example, the thought of our non-existence and the fear of the unknown of what lies beyond death. By understanding how societies deal with death, it is possible to explore the more specific issues of how patients cope, the problems that can arise and how carers should respond. This includes care of both the patient and those important to them (significant others). Bereavement support of some kind has become a fundamental aspect of palliative care, although there is a view that it continues to be a marginalized service, with reports of inequitable distribution of services.
This paper will review how to improve the understanding of the processes involved during dying and bereavement, the damaging consequences that can occur and the role of health professionals in caring for the dying and the bereaved.
Keywords
Palliative care; Adaptation; Psychiatric morbidity; Bereavement
Introduction
Our fear of death and the loss of a loved one are two of the most emotional challenges of human being. The anxiety status is usually suppressed and is only exposed when the reality of a possible death is confronted. Fear of death stems from different sources, for example, the thought of our non-existence and the fear of the unknown of what lies beyond death [1,2].
Palliative care has recognized the power of suffering of life threatening illness and is concerned with helping people to cope and adapt with these chronic illness. This is incorporated into a philosophy of care that has resulted in the principles of palliative care [3].
This paper will review literature that has improved the understanding of the processes involved, the damaging consequences that can occur and the role of health professionals in caring for the dying and the bereaved.
Fear Of Death In Society
Humanity‘s fear of death has interested artists, scientists and many philosophers, whom have considered death in terms of fear of extinction and insignificance. Psychologists and sociologists have devised models that explain death related emotion, and observed how death anxiety can bind groups (e.g. armies, religions, societies, etc.) [4].
Freud claimed that social life was formed and preserved out from fear of death. In technological and industrialized societies, death has been removed from the family home into institutions with care provided by health care professionals.
This has resulted in a lack of familiarity with the dying process, which may lead to a fear of death and dying within society. In life individuals contain such fears; death anxiety can be seen as hugely influential on behavior. Factors such as those illustrated in Table 1 illustrates the potency of death anxiety and help explain how people react when faced with death [5-7].
| Drivers of death anxiety affecting males and females [nayatanga] | Dependency |
| Pain in dying process | |
| Isolation | |
| Indignity of dying process | |
| After Life concerns | |
| Leaving loved ones | |
| Fate of the body | |
| Rejection | |
| Separation | |
| Factors affecting the general public [Diggory and Ruthman] | Grief of relatives and friends |
| End of all plans and projects | |
| Dying process being painful | |
| One can no longe care for dependents | |
| Fear of what happens if there is life after death | |
| Fear of what happens to ones body | |
| Death fears as advanced by [Chonnon] | Fear of what happens after death |
| Fear of the act of dying (eg. Pain, Loss of control and rejection | |
| Fear of ceasing to be |
Table 1: Factors that induce fear of death.
Secrets Of Death System
Not people differ in how they respond to the prospect of death, but also differ in caring for the dying and bereavement. It is useful to learn and understand the different factors that influence these behaviors.
Although personal factors are very important (e.g. age, gender, nature of disease and treatment, coping mechanisms, social support, personality, etc.), these partly relate to what is known as the 'death system' in the society. This phenomenon varies between societies and depends on the following different four factors [8]:
1. Exposure to death prior experience, which has a strong influence on the approach to subsequent deaths, including our own.
2. Life expectancy-society, which holds an estimate for what is considered a reasonable life span, based on observations of the community.
3. Perceived control over the forces of nature-beliefs about the ability to influence destiny (fate vs. control), which will affect perceptions of death.
4. Perception of human-'meaning' in this context, which relates to a variety of belief systems that constitute spirituality.
Personal Spirituality
Spirituality is concerned with how individuals understand the purpose and meaning of their existence within the universe. An individual require developing a harmonious intellectual connection between themselves and their spiritual thought and believes.
Some individuals possess a set of beliefs that adequately answer this challenge, but others can suffer as they strive to attain an inner peace, and death poses a challenge to these personally held belief systems. The spiritual component of health is an important theme in the palliative care philosophy, and is recognized as one of the four components of holistic approaches and assessment in palliative care [9].
On the same time, hospice has developed a standard for the assessment, delivery and evaluation of spiritual care, which includes three levels of assessment; routine assessment for all patients, multidisciplinary assessment particularly sensitive to spiritual issues, and specialist assessment undertaken by a chaplain as an example [10].
The multidisciplinary professionals should remain aware of this when considering the spiritual needs of patients and spiritual health can be encouraged in several ways:
1. Eliminate the distraction of physical suffering.
2. Encourage the expression of repressed emotion.
3. Assist patients to attain spiritual growth, either by personal reflection or with the help of an adviser.
4. Respect the individuals and their cultures in all interactions.
Adapting To Dying
By understanding how societies deal with death, it is possible to explore the more specific issues of how patients cope, the problems that can arise and how carers should respond. This includes care of both the patient and those important to them (significant others).
Various psychological models have been developed which provide insight into patients' responses to their impending death. The most celebrated work was performed by Kubler-Ross [11], who described a five-stage model of dying: denial, anger, bargaining, depression and acceptance.The main advantage of these theories is that they allow us to make sense of people's behavior more constructively.
In 1993, Parkes submit and sums it all up succinctly: It is not enough for us to stay close and open our hearts to another person's suffering: valuable as this sympathy may be, we must have some way for stepping aside from the maze of emotion and sensation if we are to make sense of it [2].
However, these models have some limitations. They should only be used to assist in the understanding of patients. In addition to that, those models allow the carers not to be overwhelmed by the emotions observed, and may prevent the individual needs of the patient and carers being assessed and met.
Particular problems in adapting to dying
In many cases, the psychosocial needs of the patient and carers are met with honest information given sensitively. But in more complex instances, the debilitating effects of the adaptive process require more intense professional support. Physical symptoms can be influenced by the emotional state of patients. This is because of concepts such as 'total pain' is at the core of the palliative care philosophy. Consequently, emotional distress can be an important component in physical suffering, as well as, in its management. When facing death, there is a group of emotional responses that can occur; this can be difficult for patients to bear. These include anger, anxiety, guilt, depression, and feelings of isolation from the environment. In addition, the enormity of the adaptive process can be overwhelming and result in psychiatric morbidity, such as depression, anxiety, panic and even suicidal behavior.
Not surprisingly, family and friends are subjected to a series of actual and potential losses. Examples of these challenges include the following:
• Concerns about the burden of caring
• Loss of a certain future
• Loss of role within the family and the outside world
• Loss of financial security
• Issues about sexuality
In many cases these problems provoke emotions in carers that are similar to those experienced by their dying loved one. Such emotional strain can result in significant levels of, anxiety, weight loss and even sleeplessness. The multidisciplinary team has an important role in recognizing the potential dangers of caring for a loved one and should try to prevent those problems.
How can we manage the adaptation process to dying?
Assessment of the emotional needs of dying patients and significant others requires an empathic attitude complemented by adept communication skills and familiarity with the issues surrounding the subject. Certain factors may be inherently influential on the process of adaptation (age, gender, interpersonal relationships, the nature of disease, past experience and culture).
Symptom control: Symptom management is a key requirement of the adaptation process, which then facilitate the management of emotional needs.
Communication: Skills in communication are important to effective and sensitive care. Counseling is concerned with enabling individuals to attain solutions to an emotional challenge by using particular techniques. This approach can be especially helpful in unusually difficult situations.
Maintaining hope: Patients require hope to be sustained. This is achieved either by setting achievable goals. The hope should reflect or be based in the reality of the situation; otherwise the goals may not be achieved.
Drugs: Appropriate use of psychotropic medicines (antidepressants, anxiolytics or antipsychotics) is occasionally useful. Various complementary modalities can be helpful in relieving emotional distress. However, it is usually necessary to make a detailed individual assessment with incorporation the opinions of the multi-disciplinary team.
Emotional Crises
Emotional crises do not arise without a trigger and pre-morbid factors of vulnerability and understanding both of these for patient and family. This will help in management of the distress. What is important here is that, vulnerable patients and families should be identified in order to try to prevent crises through proactive access to additional support. Table 2 illustrates various risk factors have been identified for emotional crises [12].
| For the patient | Pre-morbid factors in the family at diagnosis |
| Strong dependency issues; hostility; ambivalence | |
| Other stresses within the family, eg. Relationship problems, poor housing | |
| Illness and bereavement history-previous experiences of death and loss are important both in the quantity of experience and cping mechanisms | |
| Poor coping mechanisms | |
| Psychiatric history | |
| For the family | Poor patients adjustment compounds their risk of distress |
| Nature of illness affecting families, Example of older male patients dying from lung cancer and of young women dying from cancer of the cervix are more at risk of becoming overwhelmed and distressed |
Table 2: Various risk factors have been identified for emotional crises.
How can we manage the Emotional Crises?
It is important to have a team approach, with more than one professional available to a family in acute distress. In addition to that, the distress needs to be acknowledged and space must be given for the patient and/or family to regain control. In order to facilitate this, the cause of the distress should be explored, and 'cues' to this may need to be picked up from the patient. Once the background and the triggers have been understood a plan can be negotiated. Many crises arise because the patient and/or family feel trapped, with no control and with no choices and options. Any physical and practical input required should be provided in order to reduce concerns and facilitate a sense of control over the situation. Discussing options that they have not perceived can diminish distress. Follow-up is essential to review, modify the plan when necessary, and to explore any unresolved issues. A sense of security for the patient and family, and also trust in the professional team are important therapeutic components.
Adapting To Bereavement
There has been considerable research into the adverse health consequences of bereavement [13,14]. The bereaved are at greater risk of death themselves, although this risk remains low in absolute terms. Table 3 illustrates the different example of abnormal bereavement reactions [15]. On the other hand, adapting to bereavement has been difficult to perform, and the bereaved persons are at risk of the following complications [13,14]:
| Absent | Delayed | Chronic |
|---|---|---|
| Individuals show no evidence of the emotions of grief developing, inspite of the reality of the death. His can appear as an automatic reaction or the result of active blocking. | This initially presents in a similar way to absent grief. However, this avoidance is always a conscious effort and the full emotions of grief are eventually expressed after a particular trigger. This may be seen in more compulsively self-reliant individuals. | In this instance, the normal emotions of grief persist without any diminution over time. It is postulated that is most often seen in relationships that were particularly dependent. |
Table 3: Example of abnormal bereavement reactions.
Anxiety
Depression
Alcohol abuse
Increased use of prescribed drugs
Suicidal tendencies and behavior.
How can we manage the bereavement needs?
As in other aspects of palliative care, accurate assessment is a necessary part of management. This could be performed by any member of the multi-disciplinary team and is best achieved by someone with the following attributes:
Good communication skills to facilitate expression of emotion.
An ability to screen for psychiatric disease (e.g., anxiety, depression suicidal intent).
An understanding of the social background.
Familiarity with events surrounding death.
An awareness of risk factors of pathological grief, which are illustrated on Table 4.
| Risk factors for pathological bereavement |
| Younger age |
| Poor social support |
| Sudden death |
| Previous poor physical health |
| Previous mental illness |
| Poor coping strategies |
| Multiple losses |
| Stigmatized death |
| Economic difficulties |
| Previous unresolved grief |
Table 4: Example of abnormal bereavement reactions.
Although there are known adverse health consequences of bereavement, many bereaved individuals adapt to their loss with minimal assistance from health care professionals. There are potential dangers in overmedicating grief. For instance, bereavement can promote emotional growth within individuals and families. However, accurate assessment of risk remains the key component of appropriate bereavement management [16]. The recently developed Supportive and Palliative Care Guidelines outlines a three-component model of bereavement support, as illustrated on Table 5.
| Elements of the three-component model of bereavement support | |
| Component 1 | Grief is normal after bereavement and most people manage without professional intervention. |
| All bereaved people should be offered information about the | |
| Component 2 | Some people may require a more formal opportunity to review and reflect on their loss experience. |
| Volunteer bereavement support workers, self-help groups, faith groups and community groups provide much of the support at this level. | |
| Component 3 | A minority of people will require specialist interventions. This will involve mental health services, psychological support services, specialist counselling/psychotherapy services, specialist palliative care services andgeneral bereavement services. |
Table 5: Elements of the three-component model of bereavement support.
Bereavement services
As a result of the assessment it may be necessary to provide some emotional support. This could involve brief intervention by the professional making the assessment or by using the array of bereavement services available.
The services listed below do not include the very important help provided by religious advisers. Besides the bereavement services, various communities have developed social groups designed to overcome loneliness.
Written information: For those with low risk, providing written information may be all that is needed. This could range from pamphlets on where to get help should problems arise, to practical guides on what to do after a death and self-help books that normalize the bereavement process.
Primary care team (GPs): Promotes continuity of care and encourages primary care involvement in bereavement support. Although bereavement visits are made, GP input tends to be variable and in many cases is only reactive to requests for help.
GP bereavement care could include such things as a bereavement visit, brief emotional support, referral to practice counselor, and use of psychotropic drugs or the involvement of other services. The key worker may have an ongoing supportive role for some time and should assess the need for referral to other agencies.
Specialist palliative care services: The hospice/palliative team has seen bereavement care as integral to its service and has adopted a proactive approach. They can provide many services, including: one-to-one support; telephone contact; written information; social activities; group work; and memorial services [17].
In general, trained volunteers who are supervised by hospice staff perform this work.
Voluntary services: In the United Kingdom (UK) the main voluntary service is CRUSE Bereavement Care. This national organization takes referrals from any source and can provide one-to-one or group work.
It is staffed by trained volunteers and functions with a system of formal supervision. They prefer to take self-referrals and are contactable by phone. The experience of some volunteers makes them able to tackle complex bereavement reactions.
Hospital-based services: Most hospitals have bereavement officers to assist with certain aspects of the arrangements following the death of an in-patient. Some departments provide other aspects of support for particular bereavements.
Some casualty departments have a role following sudden deaths brought to them. Midwives or maternity units may provide support to their patients who suffer loss. In addition, psychiatric teams are involved in the more damaging bereavement reactions, particularly those resulting in major psychiatric illness.
Funeral directors: Some funeral directors are beginning to consider bereavement support as part of their service.
Specialist palliative care services: Supporting the bereaved involves the application of the communication skills (e.g. active listening, empathy, setting limits, clarification).
Generally these have been based on the concept of 'grief work', of which Worden's [18] suggests that it is helpful to separate counseling (helping people facilitate normal grief) from therapy (specialist techniques that help with abnormal grief).
Central to this approach is the need for the bereaved to work through the four 'tasks of mourning‘, starting by task 1 (accepting the reality of the loss) till task 4 (relocating emotionally the deceased and moving on with life), as illustrated on Table 6.
| Absent | Action |
|---|---|
| Task 1 | To accept the reality of the loss |
| Task 2 | To work through the pain of grief |
| Task 3 | To adjust to the environment in which the deceased is missing |
| Task 4 | To emotionally relocate the deceased and move on with life |
Table 6: The four “tasks of mourning”.
This model has recently been criticized for not allowing denial, lacking evidence of effectiveness, and inconsistencies with crosscultural historical perspectives.
Conclusion
Death, dying and bereavement challenges the fundamental values and meaning of the human experience. Such a threat has the potential to provoke considerable distress and has therefore interested health professionals. As a consequence, it has been possible to identify mal-adaptations and formulate responsive patterns of care. This has considerable implications for the work of health care professionals.
It is important while providing care that we do not lose sight of the individual patient involved and the individuality of each experience of dying, death and bereavement.
REFERENCES
- Heidegger M. Basic writings: From Being and Time (1927) to the task of thinking (1964). In: Krell FD (ed) Being and Time (2nd edn), Harper Collins Publishers New York, USA, 1972; pp: 37-88.
- Parkes CM. Bereavement as a psychosocial transition; Process adaptation and change. In: Dickinson D, Johnson M, Katz JS (eds) Death, Dying and Bereavement (2nd edn), Sage publications Ltd, 6 Bonhill street, London EC2A 4PU UK, 1993; pp: 323-331.
- World Health Organisation, Cancer Pain Relief and Palliative Care: Report of the WHO Expert Committee, Geneva: WHO, 1990.
- Kastenbaum R. Death in the midst of life. In: Gold H, Lankas P (eds) The Psychology of Death (3rd edn), Springer Publishing Company, New york, USA,1972; pp: 97-160.
- Nyatanga B. Why is it so Difficult to Die? (2nd edn) Wiltshire: Quay Books, London UK, 2001.
- Diggory J, Rothman D. Values destroyed by death. J Abnorm Soc Psychol. 1961; 63(1): 205-210.
- Chonon J. Death and the Modern Man. Macmillan publishing group, New York, USA,1974.
- Pattison EM. The living-dying process. In: Garfield CA (ed) Psychological Care of the Dying Patient. McGraw-Hill, New York, USA,1978; pp: 133-167.
- Narayanasamy B. Spiritual Care: A Resource Guide. Nottingham: BKT Information Services, 1991.
- Hunt J, Cobb M, Keeley VL, Ahmedzai SH. The quality of spiritual care: Developing a standard. Int J Palliat Nurs 2003;9(5): 208-215.
- Kubler-Ross E. Attitude towards death and dying. On Death and Dying. Macmillan, New York, USA,1969; pp: 11-36.
- Wellisch DK, Fawzy F, Landsverk JA, Pasnau RO, Wolcott DL. Evaluation of psycholsocial problems of the homebound cancer patient: the relationship of the disease and the sociodemographic variables of patients to family problems. J Psychosoc Oncol. 1983;1(3): 1-15.
- Woof WR, Carter YH. The grieving adult and the general practitioner: A literature review in two parts (part 1). Br J Gen pract. 1997; 47(420): 443-448.
- Woof WR, Carter YH. The grieving adult and the general practitioners: A literature review in two parts (part 2). Br J Gen pract. 1997; 47(421): 509-514.
- Middleton W, Moylan A, Raphael B, Burnett P, Martinek N. An International perspective on bereavement and related concepts. Aus NZ J Psych. 1993; 27(3): 457-463.
- Milliar-Smith C. The risk assessment of bereavement in a palliative care setting. Int J Palliat Nurs. 2002;8(6): 281-287.
- Payne S, Relf M. The assessments of need for bereavement follow up in palliative and hospice care. Palliat Med. 1994;8(4): 291-297.
- Worden JW. Grief counselling and grief therapy. Springer Publishing Company, New York, uSA,1992; pp: 7-23.
Citation: Al-Shaqi MA (2019) Adapting to Dying and Bereavement of Geriatric Palliative Care. J Aging Sci. 7: 213. Doi: 10.35248/2329-8847.19.07.213.
Copyright: © 2019 Al-Shaqi MA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.