Indexed In
- Open J Gate
- Genamics JournalSeek
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
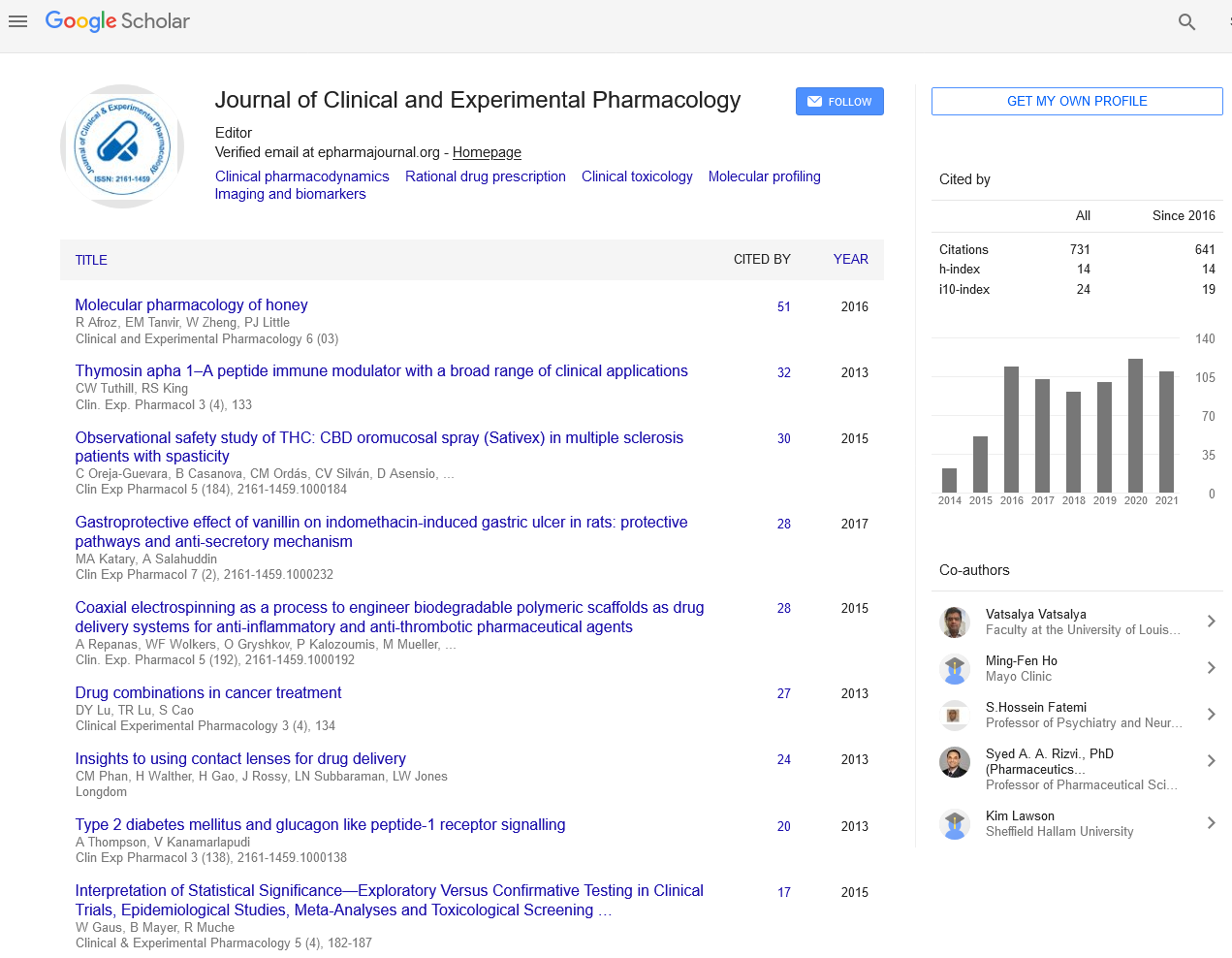
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Commentary - (2021) Volume 11, Issue 6
A Note on Risks of Hemodialysis
Saangi Catherine*Received: 10-Jun-2021 Published: 01-Jul-2021, DOI: 10.35248/2161-1459.21.11.286
About the Study
Ageing is associated with persisting systemic inflammation, both in chronic form and as delayed resolution after acute inflammatory illnesses. The clearest markers of this are raised blood concentrations of pro-inflammatory cytokines and other chemo kinesis that are involved in mediating an inflammatory state, and C-reactive protein as general indicator of inflammation. This condition of “inflammaging” is linked causally in a complex and reciprocal manner with several diseases that are prevalent in older people including a tendency to develop delirium during acute perturbations of brain function, and to a predisposition to dementia and other ageassociated neurodegenerative conditions. There is evidence of a key role of cytokines both in the aetiologies of such diseases and in the immune modulation processes that reduce inflammation, and evidence that interleukin-6 has a particularly complex effect depending on physiological and metabolic context. It is probable that the influence of cytokines on the central nervous system is directly mediated via receptors on neurons, microglial cells and astrocytes, rather than through secondary metabolic effects. The epigenetic mechanisms involved are starting to be understood. Though the descriptive phenomenology of inflammation has produced a large amount of information it is obviously, like the biochemistry of all living organisms, an extremely complex environment that cannot be described adequately using linear pathways, or even 3-dimensional models. To deal with the complexity, fluidity, stability, responses and fluctuations of immune chemistry it is proposed that a better grasp of immune system regulation, its responses to perturbation and its relationship with disease states and aging, including neuropathology, might be better progressed by using a multifactorial conditional logic approach, such as Boolean analysis. Such work will require an iterative collaboration between clinicians, molecular biologists, mathematicians and software engineers.
Low blood pressure (hypotension): A drop in blood pressure is a common side effect of hemodialysis, particularly if you have diabetes. Low blood pressure may be accompanied by shortness of breath, abdominal cramps, muscle cramps, nausea or vomiting.
Muscle cramps: Although the cause is not clear, muscle cramps during hemodialysis are common. Sometimes the cramps can be eased by adjusting the hemodialysis prescription. Adjusting fluid and sodium intake between hemodialysis treatments also may help prevent symptoms during treatments.
Itching: Many people who undergo hemodialysis have itchy skin, which is often worse during or just after the procedure.
Sleep problems: People receiving hemodialysis often have trouble sleeping, sometimes because of breaks in breathing during sleep (sleep apnea) or because of aching, uncomfortable or restless legs.
Anemia: Not having enough red blood cells in your blood (anemia) is a common complication of kidney failure and hemodialysis. Failing kidneys reduce production of a hormone called erythropoietin, which stimulates formation of red blood cells. Diet restrictions, poor absorption of iron, frequent blood tests, or removal of iron and vitamins by hemodialysis also can contribute to anemia.
Bone diseases: If your damaged kidneys are no longer able to process vitamin D, which helps you absorb calcium, your bones may weaken. In addition, overproduction of parathyroid hormone-a common complication of kidney failure-can releases calcium from your bones.
High blood pressure (hypertension): If you consume too much salt or drink too much fluid, your high blood pressure is likely to get worse and lead to heart problems or strokes.
Fluid overload: Since fluid is removed from your body during hemodialysis, drinking more fluids than recommended between hemodialysis treatments may cause life-threatening complications, such as heart failure or fluid accumulation in your lungs (pulmonary edema).
Inflammation of the membrane surrounding the heart (pericarditis): Insufficient hemodialysis can lead to inflammation of the membrane surrounding your heart, which can interfere with your heart's ability to pump blood to the rest of your body.
High potassium levels (hyperkalemia): Potassium is a mineral that is normally removed from your body by your kidneys. If you consume more potassium than recommended, your potassium level may become too high. In severe cases, too much potassium can cause your heart to stop.
Access site complications: Potentially dangerous complicationssuch as infection, narrowing or ballooning of the blood vessel wall (aneurysm), or blockage-can impact the quality of your hemodialysis. Follow your dialysis team's instructions on how to check for changes in your access site that may indicate a problem.
Amyloidosis: Dialysis-related amyloidosis develops when proteins in blood are deposited on joints and tendons, causing pain, stiffness and fluid in the joints. The condition is more common in people who have undergone hemodialysis for more than five years.
Depression: Changes in mood are common in people with kidney failure. If you experience depression or anxiety after starting hemodialysis, talk with your health care team about effective treatment options.
Citation: Catherine S (2021) A Note on Risks of Hemodialysis. J Clin Exp Pharmacol. 11: 286.
Copyright: © 2021 Catherine S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.