Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Mini Review - (2020) Volume 12, Issue 3
A New Classification of Iatrogenic Peripheral Nerve Injuries
Jordan T Carter*, John J Pisquiy, Michael Polmear, Rami Khalifa and Gilberto GonzalezReceived: 30-Apr-2020 Published: 30-Jun-2020, DOI: 10.35248/0974-8369.20.12.464
Abstract
Iatrogenic causes of nerve injuries make up to 17.4% of all traumatic peripheral nerve injuries. Despite significant medicolegal implications, there is no accepted classification system. In this article we propose a new classification system for iatrogenic peripheral nerve injuries: 1) Injury to the nerve when the nerve was not the target of the treatment; 2) Injury to the nerve when the nerve was targeted for intervention but not repair; 3) Injury to the nerve when the nerve was targeted for harvest or repair of another nerve.
Keywords
Iatrogenic peripheral nerve injuries; Neurosurgery; Peripheral nerves
Introduction
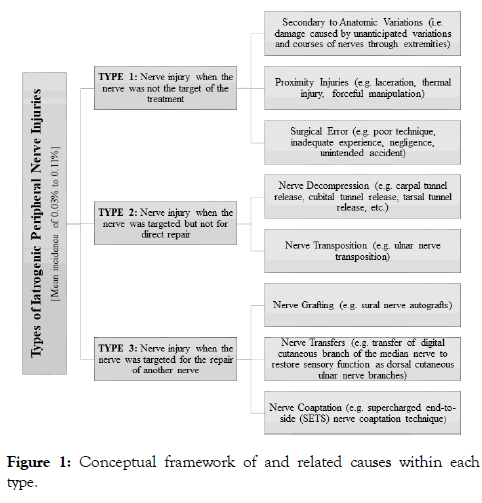
Iatrogenic nerve injuries are defined as nerve injuries caused by medical intervention or accidental damage by a physician during surgical intervention [1]. The incidence of iatrogenic peripheral nerve injuries has been reported to vary from 0.03-0.11% [2]. Peripheral nerve injuries are considered as a potential complication in various non-surgical and surgical procedures including nerve blocks, application of tourniquets, pressure/ traction injuries during preoperative patient positioning, and direct intraoperative damage1. Recent literature has reported that up to 17.4% of all traumatic nerve injuries occur due to iatrogenic causes, and 94% of those iatrogenic causes are associated with a surgical procedure [3]. These injuries carry economic importance as 16% of malpractice litigation is associated with iatrogenic nerve injuries [4]. In literature there is no current accepted classification system for operative iatrogenic nerve injuries, and classification systems are essential in orthopaedics as they characterize problems, provide an avenue for reporting epidemiological data for uniform comparisons, and guide decision making to prevent current or future errors to optimize clinical outcomes [5]. The purpose of this article is to propose a new classification system for operative iatrogenic nerve injuries to identify injury patterns associated with certain procedures. The classification is divided into three types, wherein: 1) Injury to the nerve when the nerve was not the target of the treatment; 2) Injury to the nerve when the nerve was targeted for intervention but not repair; 3) Injury to the nerve when the nerve was targeted for harvest or repair of another nerve (Figure 1).
Figure 1: Conceptual framework of and related causes within each type.
Literature Review
Type 1: Injury to the nerve when the nerve was not the target of the treatment
This type of nerve injury can occur during surgical procedures due to rare anatomic variations, operating in close proximity to a nerve, or surgical error. Anatomic variations may result in iatrogenic injury due to unanticipated courses within planned dissection planes [6]. While these injuries could be potentially avoided with careful dissection, knowledge of anatomic variations is important to avoid intraoperative complications [7]. Furthermore, operating close to a nerve can result in nerve damage either via laceration or thermal injury via electrocautery [8]. These injuries are recognized risks of extremity surgery and are components of the informed consent for the procedure. Surgical errors secondary to technique, inexperience, poor anatomic knowledge, and negligence (e.g. extended tourniquet times, forceful retraction, etc.) are other potential sources of iatrogenic injury and may have medicolegal implications [2].
Type 2: Injury to the nerve when the nerve was targeted but not for direct repair
Nerve decompression and transposition procedures for compressive neuropathies are the primary causes of this type of iatrogenic nerve injury. Traditionally, carpal tunnel releases are reported to have the highest number of iatrogenic peripheral nerve injuries [2]. Other surgical procedures in this category include cubital tunnel decompression of the ulnar nerve, tarsal tunnel decompression of the posterior tibial nerve, or decompression of the superficial peroneal nerve as it crosses the fibular head [3].
Nerve transpositions carry additional risk of ischemia, relative to decompression surgeries because they require adequate dissection to ensure a tension-free transposition [9]. For example, decompression for cubital tunnel syndrome via ulnar nerve transposition results in higher complication rates compared to decompression and does not yield clinically superior results [10]. In one meta-analysis, the incidence of nerve damage after ulnar nerve transposition was 0.17% compared to 0.096% after simple decompression [11]. While these surgeries do directly target the nerve, the nerve is not intended to be internally manipulated for repair or grafting.
Iatrogenic nerve block injuries also fall under this category as specific nerves can be targeted to provide pain relief preoperatively, perioperatively, and postoperatively in orthopaedic surgeries. The incidence of post-nerve block neuralgia (e.g. pain and paresthesia after a peripheral nerve block) has been estimated to vary 0.2% to 12.5% [12]. Nerve injury can occur due to mechanical trauma from the needle, pressure injury, intraneural injection, neuronal ischemia, iatrogenic injury related to surgery, and local anesthetic neurotoxicity [13]. While post-block neuralgia can be transient, some may result in permanent disability (e.g. unremitting pain and paralysis) [12]. Both anesthesia and surgical teams routinely perform peripheral nerve blocks (PNB) and neuraxial blocks (e.g. brachial plexus block) as a therapeutic measure to provide pain relief.
Type 3: Injury to the nerve when the nerve was targeted for the repair of another nerve
Nerve damage can occur when nerves are targeted for harvest or repair during nerve grafting, nerve transfers, and coaptation. Nerve grafting involves repairing a damaged nerve with donor or artificial nerve graft when conventional tension-free repair cannot be achieved. When using autografts for nerve repair, sensory nerves (e.g. sural nerve) are often used despite the risk of causing decreased or complete loss of sensation distally [14].
Nerve transfers involve redirecting a functional nerve to the motor or sensory distribution of an injured nerve [15,16]. These transfer surgeries are performed for muscle reinnervation, following an amputation, or in the repair of penetrating nerve injuries. Targeted Muscle Reinnervation (TMR) has been used to mitigate symptomatic neuroma formation, phantom limb pain, and use of myoelectric prostheses [17,18]. However, damage can occur through the surgical procedure and can cause a loss of sensation in the distribution of the donor nerve (e.g. decreased 3rd web-space sensation when using a digital cutaneous branch of the median nerve to restore sensory function in damaged dorsal or palmar cutaneous ulnar nerve branch) [15,19].
Nerve coaptation is another procedure that can lead to nerve damage within Type 3 iatrogenic nerve injuries. Coaptation involves splicing in a branch of a functional nerve into an injured nerve using an end-to-end or end-to-side technique, it promotes functional motor recovery via axonal regeneration within target muscles. The end-to-side technique is often referred in the supercharged end-to-side (SETS) nerve coaptation of the Anterior Interosseous Nerve (AIN) to the ulnar motor nerve in proximal ulnar nerve injuries [20]. Similar to other nerve repair surgeries, this procedure can augment reinnervation but the risk of sensory and motor deficits in the donor nerve distribution remains. Optimal donor nerves will be in close proximity to the damaged nerve to allow for tension-free constructs, yet have minimal or no clinical sensory and motor deficits in the donor distribution.
Limitations
One important limitation of our proposed classification system is that we cannot directly determine the validity or sensitivity of this classification system as there is no current system in place to measure our classification system against, and no studies have been conducted using this system. We can assume that there will be high interobserver reliability, but further studies are needed to determine each of these parameters. Our study also focused primarily on operative iatrogenic nerve injuries and it did not account for iatrogenic nerve injuries related to non-operative causes.
Conclusion
Iatrogenic causes are a relatively common etiology of peripheral nerve injuries, and they can result in significant functional deficits. Nerve damage like neuropraxia may resolve, but many injuries like neurotmesis and axontmesis may be irreversible. We have composed a classification system for iatrogenic peripheral nerve injuries consisting of three categories: 1) Injury to the nerve when the nerve was not the target of the treatment; 2) Injury to the nerve when the nerve was targeted but not for direct repair; and 3) Injury to the nerve when the nerve was targeted for the repair of another nerve. We anticipate this classification system accompanied by a thorough history and physical exam could allow for improved understanding of the injuries and enhance treatment of the associated neurological deficits in patients. Understanding the risk of neurologic deficits associated with various surgical interventions and applying this classification systemic may optimize the use of electrodiagnostic studies, advanced imaging, and surgical planning (Tables 1 and 2).
Table 1: Iatrogenic Nerve Classification System and Possible Etiologies.
| Categories | Type 1 | Type 2 | Type 3 |
|---|---|---|---|
| Description | Injury to the nerve when the nerve was not the target of the treatment | Injury to the nerve when the nerve was targeted but not for direct repair | Injury to the nerve when the nerve was targeted for the repair of another nerve |
| Etiology | Iatrogenic laceration or transection of the nerve | Iatrogenic laceration or transection during decompression or transposition | Deficit in autologous nerve graft motor or sensory distribution |
| Retraction injury | Ischemia and traction from excess tension following transposition | Deficit in motor or sensory distribution of transferred nerve | |
| Thermal injury | Iatrogenic laceration or transection of the target nerve | Deficit in motor or sensory distribution of coapted nerve | |
| Ischemia from extended tourniquet time | Iatrogenic laceration or transection of recipient nerve | ||
| Example | Lymph node biopsies [18] | Carpal tunnel release [1,2,18] | Nerve graft harvest [10] |
| Fracture fixation [18] | Cubital tunnel release [8,9] | Nerve transfer [11,15,17] | |
| Hernia repair [18] | Tarsal tunnel release [2] | Targeted muscle Reinnervation following BKA or transhumeral amputation [12-14] | |
| Vascular procedures [18] | Nerve sheath tumor excision [18] | AIN SETS [16] | |
| Decompression of the superficial peroneal nerve at the fibular head [2] | Nerve coaptation in high brachial plexus injuries [19] | ||
| Ulnar nerve transposition [7,8] | Nerve coaptation in the repair of ECRB and PIN with branches of the median nerve [20] |
Table 2: Summary of Studies included in Review of Iatrogenic Nerve Injuries.
| Author | Journal | Article Title | Major Points and Findings |
| Altay et al. [9] | Ortop Traumatol Rehabil | Comparison of Simple Decompression and Anterior Subcutaneous Transposition of the Ulnar Nerve for the Treatment of Cubital Tunnel Syndrome. | Postoperatively, paraesthesia regressed in 17 (85.7%) and 30 (85%) patients in Group 1 (Transposition) and Group 2 (Decompression), respectively |
| Both simple decompression and anterior subcutaneous transposition of the ulnar nerve are effective and safe for the treatment of cubital tunnel syndrome, so we would favour simple decompression as it is a less extensive procedure. | |||
| Antoniadis et al. [3] | Dtsch Arztebl Int. | Iatrogenic nerve injuries: prevalence, diagnosis and treatment | 17.4% of the traumatic nerve lesions treated were iatrogenic. 94% of iatrogenic nerve injuries occurred during surgical procedures. |
| A thorough knowledge of the anatomy of the vulnerable nerves and of variants in their course can lessen the risk of iatrogenic nerve injury. | |||
| Armangil et al. [8] | Acta Orthop Traumatol Turc | Posterior tibial nerve as a tendon transfer for drop foot reconstruction: a devastating complication | The various operative and non-operative mechanisms of iatrogenic injury are well known and include transection, stretching, compression, injections, heat, radiation, and the use of anticoagulant agents. |
| Iatrogenic transection of a major nerve during surgery is an avoidable problem and negative outcomes can be minimized with early recognition and treatment. | |||
| Bowen et al. [16] | Plast Reconstr Surg | Targeted Muscle Reinnervation Technique in Below-Knee Amputation | Previous studies prove that targeted reinnervation successfully treats and, in some cases, resolves peripheral neuropathy and phantom limb pain in patients who have undergone previous amputation (i.e., secondary targeted reinnervation). |
| This study extends the success of targeted muscle reinnervation to below-knee amputations and provides a description for this technique. | |||
| Bowen et al. [17] | Adv Wound Care | Targeted Muscle Reinnervation to Improve Pain, Prosthetic Tolerance, and Bioprosthetic Outcomes in the Amputee | Primary Targete Muscle Reinnervation (TMR) aims to optimize efficacy and efficiency and demonstrates great potential for establishing a new standard of care for amputees. |
| Primary TMR performed at the time of amputation suggests that it may prevent neuroma formation while avoiding the risks associated with a delayed procedure. | |||
| Carter et al. [7] | Cureus | Bilateral Congenital Absence of Small Finger Flexor Digitorum Superficialis Tendons in a Trauma Patient | Anatomical variations of the forearm flexor muscles are common, and there are several documented variations of the Flexor Digitorum Superficialis (FDS). Variations in the FDS are clinically important for the assessment of injuries and pre-surgical planning for harvesting the small finger FDS tendon. |
| Davidge et al. [20] | J Hand Surg Am | Median to radial nerve transfers for restoration of wrist, finger, and thumb extension | By providing a dense source of motor axons with synergistic function and in close proximity to the motor end-plates of the extensor musculature, the FDS and Flexor Carpi Radialis (FCR) branches of the median nerve are ideal donors for reinnervation of the Extensor Carpi Radialis Brevis (ECRB) and Posterior Interosseous Nerve (PIN), respectively. |
| It is important to dissect the recipient nerves as proximally as possible and the donor nerves as distally as possible, to ensure sufficient redundancy so that the nerve coaptation remains completely tension free in all ranges of motion of the arm. | |||
| den Brave et al. [6] | J Orthop Trauma | Anatomical Variations of the Lateral Femoral Cutaneous Nerve and Iatrogenic Injury After Autologous Bone Grafting From the Iliac Crest | All 9 known anatomical variations of the Lateral Femoral Cutaneous Nerve (LFCN) in the literature are reviewed, and the importance of these anatomical variations for surgeons and anesthetists is stressed. |
| For every trauma, orthopedic, plastic, and cranio-maxillofacial surgeon and anesthesiologist it is important to know the anatomy of the LFCN and its known variations. | |||
| Dunn et al. [10] | J Shoulder Elbow Surg | Retrospective, nonrandomized analysis of subcutaneous anterior transposition versus in situ decompression of the ulnar nerve of military service members | In comparing functional outcomes of subcutaneous anterior transposition (SAT) vs. in situ decompression (SD) of the ulnar nerve for the treatment of cubital tunnel syndrome, SD patients had a statistically significantly lower minor complication rate than SAT patients (45% vs. 70%) and no difference in major complications. |
| There is no advantage to SAT over SD in primary surgically treated CuTS even in a high-demand, physically active population. | |||
| Flores et al. [21] | J Reconstr Microsurg | Comparative Study of Nerve Grafting versus Distal Nerve Transfer for Treatment of Proximal Injuries of the Ulnar Nerve | In patients with nerve injuries, pain may be relevant and causes extreme discomfort. The pain can be attributed to neurotmesis which results in traumatic neuroma formation. |
| Pain and damage cannot be alleviated until neuroma formation is transected. | |||
| Garbuz et al. [5] | JAAOS | Classification systems in orthopaedics | Classification systems help orthopaedic surgeons characterize a problem, suggest a potential prognosis, and offer guidance in determining the optimal treatment method for a particular condition. |
| Classification systems also play a key role in the reporting of clinical and epidemiologic data, allowing uniform comparison and documentation of like conditions. | |||
| Jarvie et al. [22] | J Orthop Case Rep | Supercharge End-to-Side Anterior Interosseous Nerve to Ulnar Motor Nerve Transfer for Severe Ulnar Neuropathy: Two Cases Suggesting Recovery Secondary to Nerve Transfer | Supercharged end-to-side (SETS) nerve transfer for severe cubital tunnel syndrome is a recently described technique, which involves augmenting the ulnar motor branch with the terminal branch of the anterior interosseous nerve (AIN). |
| Karamanos et al. [15] | Perm J | Nerve Transfer Surgery for Penetrating Upper Extremity Injuries | Nerve transfer is a safe, effective technique for correcting penetrating trauma-related nerve injury. Nerve transfer surgery involves taking nerve branches from a neighboring nerve and redirecting them to the distal end of the injured nerve. |
| In nerve grafting the body then regenerates axons along the new path, and the motor cortex subsequently rewires itself to relearn muscle functions. The process can take months or years to produce good results. The disability can become permanent. | |||
| Kornfeld et al. [14] | Wien Med Wochenschr | Nerve grafting for peripheral nerve injuries with extended defect sizes | Autologous nerve graft is still the gold standard for reconstruction of peripheral nerve tissue. Although, autologous donor material is highly limited in number and often mismatch the nerve defects of the reconstruction side. |
| Allografts are nearly a perfect alternative to the current gold standard technique, especially because immunosuppression is not indicated anymore to avoid a foreign body reaction. Nerve grafting with cell suspensions e.g. with Schwann cells shows promising results on small defect sizes in animals but is limited on translation to human organism by highly regulated local laws for transplantation of human stem cells. | |||
| Kumar et al. [2] | Neurol India | Iatrogenic peripheral nerve injuries | Iatrogenic nerve injuries can occur during many surgical procedures and prevention remains the mainstay of the management of such injuries. |
| The incidence of peripheral nerve injury remains uncertain and can range from 0.03% to 0.11%. | |||
| Direct nerve injury; mechanical factors, such as compression, or retractor induced stretch; ischaemia; toxicity of injected solutions; double crush syndrome; or, a combination of the above factors. Nerves may be unduly vulnerable to trauma as a result of pre-existing predisposing factors. | |||
| Rasulíc et al. [1] | World Neurosurg | Iatrogenic Peripheral Nerve Injuries-Surgical Treatment and Outcome: 10 Years' Experience | In the case of peripheral nerve trauma, 17.4% were due to iatrogenic injuries, with the majority (94%) being secondary to a surgical procedure. |
| The most common causes of iatrogenic nerve injuries among patients in the study were the operations of bone fractures (23.9%), lymph node biopsy (19.7%), and carpal tunnel release (18%). | |||
| Evaluation of patients with iatrogenic nerve injuries is mandatory, including preoperative clinical, neurologic, electrophysiologic, and neuroradiologic examinations, as well as intraoperative exploration. | |||
| Said et al. [11] | J Hand Microsurg | Ulnar Nerve In Situ Decompression versus Transposition for Idiopathic Cubital Tunnel Syndrome: An Updated Meta-Analysis | In comparing in site simple decompression (SD) versus ulnar nerve transposition (UNT) for cubital tunnel syndrome, there is no statistically significant difference in clinical outcomes or rate of revision surgery between SD versus UNT. However, there were significantly more complications with UNT. |
| In addition to the type of approach, proper surgical technique with attention to avoiding iatrogenic injury, meticulous hemostasis, and adequate decompression is just as important to improve clinical outcomes. | |||
| Sakellariou et al. [23] | ISRN Orthop | Treatment options for brachial plexus injuries. | The incidence of brachial plexus injuries (BPI) has rapidly increased over the last 50 years, and developments in microsurgery now offer use new modalities to improve the clinical outcome of brachial plexus injuries. |
| One treatment option includes Functioning free muscle transplantation (FFMT) is the transfer of a muscle using microvascular anastomoses for revascularization and subsequent neural coaptation to the recipient motor nerve for reinnervation. | |||
| Sallam et al. [19] | J Hand Surg Am | Nerve Transfer Versus Nerve Graft for Reconstruction of High Ulnar Nerve Injuries | The study results show better outcomes when nerve transfer (NT) was used to manage cases of proximal ulnar nerve injuries versus sural nerve grafting. |
| Overall, there was more improvement in motor power and grip functions of the hand at final follow-up in the (NT) group, and complications consisted of loss of sensation in the 3rd web space. | |||
| Souza et al. [18] | Clin Orthop Relat Res | Targeted muscle reinnervation: a novel approach to post-amputation neuroma pain. | Targeted Muscle Reinnervation (TMR) offers a novel and effective therapy for patients who suffer from postamputation neuroma pain. Neuroma formation is secondary to damaged peripheral nerves. |
| All 26 patients who underwent TMR demonstrated no evidence of new neuroma pain after the procedure, and 14 of 15 patients who had preoperative neuroma pain experienced complete relief of pain in the distribution of the transferred nerves. | |||
| Zhang et al. [4] | ANZ J Surg | Iatrogenic upper limb nerve injuries: a systematic review. | In a review of 4000 adverse anaesthetic outcomes from the files of 35 professional liability insurance companies, investigators identified nerve damage as the second commonest category of claims, accounting for 16% of all cases. |
| Iatrogenic peripheral nerve injuries are a major source of distress and disability and figure prominently in litigation. Minimal access surgery does not mean minimal risk of peripheral nerve injury. | |||
REFERENCES
- RasuliÃÂ?? L, SaviÃÂ?? A, VitoševiÃÂ?? F. Iatrogenic Peripheral Nerve Injuries-Surgical Treatment and Outcome: 10 Years' Experience. World Neurosurg. 2017;103:841-851.e846.
- Kumar A, Shukla D, Bhat DI, Devi BI. Iatrogenic peripheral nerve injuries. Neurol India. 2019;67(Supplement):S135-S139.
- Antoniadis G, Kretschmer T, Pedro MT, König RW, Heinen CPG, Richter HP. Iatrogenic nerve injuries: prevalence, diagnosis and treatment. Dtsch Arztebl Int. 2014;111(16):273-279.
- Zhang J, Moore AE, Stringer MD. Iatrogenic upper limb nerve injuries: a systematic review. ANZ J Surg. 2011;81(4):227-236.
- Garbuz DS, Masri BA, Esdaile J, Duncan CP. Classification systems in orthopaedics. The Journal of the American Academy of Orthopaedic Surgeons. 2002;10(4):290-297.
- den Brave PS, Vas Nunes SE, Bronkhorst MWGA. Anatomical Variations of the Lateral Femoral Cutaneous Nerve and Iatrogenic Injury After Autologous Bone Grafting From the Iliac Crest. J Orthop Trauma. 2015;29(12):549-553.
- Carter JT PM, Herrera F, Gonzalez G. Bilateral Congenital Absence of Small Finger Flexor Digitorum Superficialis Tendons in a Trauma Patient. Cureus. 2020;12(2).
- Armangil M, Basat HÇ, Bilgin SS. Posterior tibial nerve as a tendon transfer for drop foot reconstruction: a devastating complication. Acta Orthop Traumatol Turc. 2015;49(1):111-114.
- Altay T, Yamak K, Koyuncu ÃÂ??, Kayali C, Sözkesen S. Comparison of Simple Decompression and Anterior Subcutaneous Transposition of the Ulnar Nerve for the Treatment of Cubital Tunnel Syndrome. Ortop Traumatol Rehabil. 2018;20(6):475-481.
- Dunn JC, Goddard R, Eckhoff MD, Waterman BR, Nesti LJ, Kilcoyne KG. Retrospective, nonrandomized analysis of subcutaneous anterior transposition versus in situ decompression of the ulnar nerve of military service members. J Shoulder Elbow Surg. 2019;28(4):751-756.
- Said J, Van Nest D, Foltz C, Ilyas AM. Ulnar Nerve In Situ Decompression versus Transposition for Idiopathic Cubital Tunnel Syndrome: An Updated Meta-Analysis. J Hand Microsurg. 2019;11(1):18-27.
- Kaufman BR, Nystrom E, Nath S, Foucher G, Nystrom A. Debilitating chronic pain syndromes after presumed intraneural injections. Pain. 2000;85(1-2):283-286.
- Helander EM, Kaye AJ, Eng MR. Regional Nerve Blocks-Best Practice Strategies for Reduction in Complications and Comprehensive Review. Current pain and headache reports. 2019;23(6):43.
- Kornfeld T, Vogt PM, Radtke C. Nerve grafting for peripheral nerve injuries with extended defect sizes. Wien Med Wochenschr. 2019;169(9-10):240-251.
- Karamanos E, Rakitin I, Dream S, Siddiqui A. Nerve Transfer Surgery for Penetrating Upper Extremity Injuries. Perm J. 2018;22:17-156.
- Bowen JB, Ruter D, Wee C, West J, Valerio IL. Targeted Muscle Reinnervation Technique in Below-Knee Amputation. Plast Reconstr Surg. 2019;143(1):309-312.
- Bowen JB, Wee CE, Kalik J, Valerio IL. Targeted Muscle Reinnervation to Improve Pain, Prosthetic Tolerance, and Bioprosthetic Outcomes in the Amputee. Adv Wound Care (New Rochelle). 2017;6(8):261-267.
- Souza JM, Cheesborough JE, Ko JH, Cho MS, Kuiken TA, Dumanian GA. Targeted muscle reinnervation: a novel approach to postamputation neuroma pain. Clin Orthop Relat Res. 2014;472(10):2984-2990.
- Sallam AA, El-Deeb MS, Imam MA. Nerve Transfer Versus Nerve Graft for Reconstruction of High Ulnar Nerve Injuries. J Hand Surg Am. 2017;42(4):265-273.
- Davidge KM, Yee A, Kahn LC, Mackinnon SE. Median to radial nerve transfers for restoration of wrist, finger, and thumb extension. J Hand Surg Am. 2013;38(9):1812-1827.
- Flores LP. Comparative Study of Nerve Grafting versus Distal Nerve Transfer for Treatment of Proximal Injuries of the Ulnar Nerve. J Reconstr Microsurg. 2015;31(9):647-653.
- Jarvie G, Hupin-Debeurme M, Glaris Z, Daneshvar P. Supercharge End-to-Side Anterior Interosseous Nerve to Ulnar Motor Nerve Transfer for Severe Ulnar Neuropathy: Two Cases Suggesting Recovery Secondary to Nerve Transfer. J Orthop Case Rep. 2018;8(5):25-28.
- Sakellariou VI, Badilas NK, Stavropoulos NA. Treatment options for brachial plexus injuries. ISRN Orthop. 2014;2014:314137-314137.
Citation: Carter JT, Pisquiy JJ, Polmear M, Khalifa R, Gonzalez G (2020) A New Classification of Iatrogenic Peripheral Nerve Injuries. Biol Med (Aligarh) 12:464. doi: 10.35248/0974-8369.20.12.464
Copyright: © 2020 Carter JT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.