PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Research Article - (2020) Volume 0, Issue 0
A Low Gluten Diet Suppresses Disease Activity of Rheumatoid Arthritis
Kenji Tani1*, Hinako Takagishi2,3, Yoshihiro Okura1, Shingo Kawaminami3, Keisuke Kawahito4, Keisuke Inaba5, Kaori Inaba5, Akiko Miyatake6, Keisuke Kondo3, Yoshinori Nakanishi6, Ryo Tabata3, Teruki Shimizu7 and Harutaka Yamaguchi32Department of Medicine Student Lab, The University of Tokushima, Tokushima, Japan
3Department of General Medicine, Institute of Biomedical Sciences, The University of Tokushima Graduate School, Tokushima, Japan
4Kaifu Tokushima Prefectural Hospital, Tokushima, Japan
5Yoshinogawa Medical Center, Tokushima, Japan
6Taoka Hospital, Tokushima, Japan
7Toyo Hospital, Tokushima, Japan
Received: 10-Nov-2020 Published: 02-Dec-2020, DOI: 10.35248/2157-7560.20.S7:001
Abstract
Background: This study aimed to evaluate the efficacy of a low gluten diet in the disease activity of Rheumatoid Arthritis (RA).
Methods: Among 109 patients with RA enrolled in this study, 98 patients who completed 16 weeks on a low gluten diet regimen were included in the study. At baseline, we gave the patients the information about gluten-free and gluten-contained foods, and asked them to refrain from the daily gluten consumption during the experimental period.
Results: The low gluten diet significantly improved DAS28-CRP and CDAI scores after 16 weeks. The percentages of patients achieving DAS28-CRP and CDAI-defined remission or LDA were significantly increased after 16 weeks. There was a significant increase in the percentage of the responders in EULAR treatment response after 16 weeks. Rheumatoid Factor (RF) but not C-reactive protein was significantly decreased after 16 weeks. When the self-reported level about adherence to the low gluten diet was divided into three categories, a significant decrease in DAS28-CRP, CDAI and RF was detected in the patients with the strict adherence to the low gluten diet.
Conclusion: This study demonstrates that the strict adherence to a low gluten diet results in the decreased disease activity of RA.
Keywords
CDAI; DAS28-CRP; Gluten; Rheumatoid arthritis; Rheumatoid factor
Abbrevations
RA: Rheumatoid Arthritis; NSAIDs: Non-Steroidal Anti- Inflammatory Drugs; DMARDs: Disease-Modifying Anti Rheumatic Drugs; GLG: Greatly Low Gluten; MLG: Moderately Low Gluten; PLG: Poorly Low Gluten; TJC28: 28 Tender Joint Counts, SJC28: 28 Swollen Joint Counts, PtGA: Patient Global Assessment of disease activity; PhGA: physician Global Assessment of disease activity; mHAQ: modified Health Assessment Questionnaire; CRP: C-Reactive Protein; RF: Rheumatoid Factor; CCP: Cyclic Citrullinated Peptide; DAS28: Disease Activity Score assessing 28 joints; CDAI: Clinical Disease Activity Index
Introduction
Rheumatoid Arthritis (RA) is a chronic systemic inflammatory disease characterized by destructive synovial joint inflammation leading to the substantial joint damage, deformity, and functional disability [1,2]. Joint inflammation causes tenderness and pain, which markedly reduce the quality of life of the patients. The cause of RA is unknown, but several studies suggest the importance of complex interactions among the genetic, environmental and hormonal factors, and immune system [3,4].
There is a preclinical period in the development of RA where the genetic and environmental factors interact to initiate and propagate the autoimmune process [5]. Identifying preclinical RA is important as it can help us understand the natural history of RA while developing effective screening and preventive strategies.
Associations between RA and various environmental factors have been studied [6,7], but evidence to show the factors as a causal role is inconclusive. Dietary factors are the major environmental exposure that is considered as an initiator and a risk factor for the development of RA [8]. Micronutrients in the diet may influence the intestinal and systemic immune responses contributing to the pathogenesis of RA though the existing evidence is limited [9].
Our preliminary experiments indicate that patients with RA are more likely to prefer noodles than control patients. Gluten is an important ingredient of wheat, barley, oat and rye, and these gluten-rich cereals constitute the major part of our diet such as noodles, pasta, bread, and snacks [10].
Gluten is a water-insoluble protein, and induces epithelial cell damage within the small bowel, leading to immune reactions in gluten sensitive diseases such as celiac disease [11]. Interestingly, patients with celiac disease are shown to be at increased risk for various autoimmune diseases including RA [12]. However, the direct role of the gluten exposure in the development of associated autoimmune conditions is still a matter of debate.
The possible benefits of special diets for patients with RA have been tested in several trials [13,14]. A few studies demonstrated the effect of gluten-free diet added to vegan diet on the disease activity of RA [15,16], but the actual role which gluten itself plays is not known. The primary aim of this study is to investigate whether a low gluten diet could yield an improvement in the activity of RA comparing the effect among the levels of adherence to a low gluten diet.
Methods
Study design and patients
The present study was conducted at Tokushima Prefectural Kaifu Hospital and Toyo Hospital which had a professional department for RA medical treatment. RA was diagnosed according to the 1987 American College of Rheumatology classification criteria for RA [17] or ACR/EULAR 2010 RA criteria [18]. Patients were allowed to continue on daily doses of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), oral glucocorticoids and conventional synthetic Disease-Modifying Anti Rheumatic Drugs (csDMARDs), biological DMARDs (bDMARDs) and targeted synthetic DMARDs (tsDMARDs).
Patients who either started or discontinued these medications for the previous 8 weeks and during the study were excluded. All medications except NSAIDs were on the same dosage. Patients who already lived on a gluten-free diet due to the gluten allergy were excluded. Between October 2019 and January 2020, 109 patients with RA who had been treated in the hospitals were enrolled in this study.
During the study, 11 patients were removed from this study; eight patients refused to continue the diet, a patient complicated pneumonia, a patient admitted due to bone fracture, and a patient needed bDMARDs changed. Finally, 98 patients with RA were included in this study. All patients gave written informed consent before participating in the study. The present study was approved by the Tokushima University Hospital ethics committee and was performed in accordance with the Declaration of Helsinki.
Intervention
We informed the patients the experimental protocol. Before baseline (Week 0), all patients had been in omnivorous diet. At Week 0, to patients who agreed with the study we explained what gluten-free and -contained foods were, and asked to refrain from the daily gluten consumption during the experimental period. Since gluten is included in wheat, rye, and barley, the patients were informed to avoid food products derived from these cereals, such as bread, pasta, cakes and biscuits. Other wheat-based products, which were common foods in Japan such as Japanese noodles, Japanese Tempura, cutlet, and jiaozi, were recommended to avoid to take. On the other hand, naturally gluten-free foods such as rice, potatoes, vegetables, fruit, unprocessed meat and fishes could be accepted. Manufactured gluten-free versions of wheat-based foods, such as breads, pasta and cereals were included in gluten-free foods.
This designing study was considered to be nutritionally complete. The patients lived in the low gluten diet for 16 weeks, and an interval of visit to the hospital was 8 weeks. We did not strictly prohibit to take any gluten-contained foods when the patients strongly wanted to consume them. At Week 16, the patients were questioned about the level of subjective adherence to the low gluten diet.
The self-reported level about adherence to the low gluten diet during 16 weeks was divided into six categories; “complete”, “excellent”, “moderate”, “fair”, “poor”, “not at all”. Using the information, the level of low gluten diet of each patient was divided into three groups; “complete” and “excellent” were divided into Greatly Low Gluten (GLG) group, “moderate” and “fair” into Moderately Low Gluten (MLG) group, “poor” and “not at all” into Poorly Low Gluten (PLG) group. We avoided providing the patients any information about the previous results about a low gluten diet and about other participants in this study.
Data collection
The following disease parameters were recorded at Week 0, Week 8, and Week 16: The 28 Tender and Swollen Joint Counts (TJC28 and SJC28), patient (PtGA) and physician (PhGA) Global Assessment of disease activity [mm] in which 0=best and 100=worst, and the modified Health Assessment Questionnaire (mHAQ) score [19].
The following laboratory data were assessed: C-Reactive Protein (CRP) and Rheumatoid Factor (RF). Anti-Cyclic Citrullinated Peptide (CCP) antibodies were measured at diagnosis of RA. We did not have records on anti-CCP antibodies when cases were diagnosed prior to its widespread use. The abnormal levels of RF, CRP and anti-CCP antibodies were defined as >20 IU/ml, >0.3 mg/dl, and ≥ 4.5 U/ml, respectively. When data of RF, CRP, and anti-CCP antibodies were under the sensitivity level, data of the detection limit were used (RF=4 IU/ml, CRP=0.05 mg/dl, anti- CCP antibodies=0.5 U/ml).
Definitions of disease activity and clinical assessment
As established definitions in the evaluation of RA disease activity, the Disease Activity Score assessing 28 joints with CRP (DAS28- CRP) and Clinical Disease Activity Index (CDAI) were used in this study. DAS28-CRP was scored, using TJC28, SJC28, PtGA, and CRP [20]. CDAI was scored as: TJC28+SJC28+PtGA+PhGA [21].
Concerning DAS28-CRP, the patients were divided into those in remission (<2.3), and those in non-remission (Low Disease Activity; LDA, ≥ 2.3 and <2.7: Moderate Disease Activity; MDA, 2.7-4.1: High Disease Activity, HDA, >4.1). About CDAI, the patients were divided into those in remission (<2.8), and those in non-remission (LDA, ≥ 2.8 and<10: MDA, 10-22: HDA, >22).
Changes in DAS28-CRP and CDAI scores at Week 8 and Week 16 from baseline data were analyzed and were expressed as DAS28- CRP and CDAI, respectively. Mean rates of remission, LDA, MDA, and HDA in DAS28-CRP and CDAI were calculated and compared at Week 0, Week 8, and Week 16. Clinical responses were defined by the European League Against Rheumatism (EULAR) response criteria [22]. Good response: DAS28-CRP improvement >1.2 in present DAS28-CRP ≤ 2.7. Moderate response: DAS28- CRP improvement >0.6 and ≤ 1.2 in present DAS28-CRP ≤ 2.7, and >2.7 and ≤ 4.1; DAS28-CRP improvement >1.2 in present DAS28-CRP >4.1, and 2.7 and ≤ 4.1. No response: DAS28-CRP improvement ≤ 0.6, and DAS28-CRP improvement >0.6 and ≤ 1.2 in present DAS28-CRP >4.1.The proportion of patients achieving mHAQ scores ≤ 0.5 was considered as functionally remission [23].
Statistical analysis
Median values were calculated for non-normally distributed continuous variables. Data were mainly presented as median and 25th-75th quarter, and count and percentage. Comparison between independent means was made using Mann-Whitney U test or Kruskal-Wallis test. Longitudinal changes of each parameter before and after the diet were examined by the Wilcoxon signed- rank test or Friedman test. The relationship between categorical variables was evaluated by the chi-square test. The results were regarded as significant when p value was <0.05.
All statistical analyses were performed using IBM SPSS statistics version 24 software (Chicago, IL, USA).
Results
Patient baseline characteristics
A total of 98 patients completed 16 weeks on the diet regimen and were included in our analyses. Table 1 shows the basement characteristics of overall patients. Out of the overall patients, 76 (78%) were female and the median age was 67 years old. The median disease duration of RA since diagnosis was 8 years. During this study, TJC, SJC, PtGA, PhGA, mHAQ and CRP were measured in all patients. RF at baseline and anti-CCP antibodies at the diagnosis of RA were measured in 90 patients (92%) and 62 patients (63%), respectively.
| Variables | |
|---|---|
| Sex (male : female) | 22 (22%): 76 (78%) |
| Age (y) | 67 (56 -73) |
| Disease duration (y) | 8 (4-13) |
| TJC, 0-28 | 1 (1-3) |
| SJC, 0-28 | 2 (0-4) |
| PtGA (mm) | 15 (7-27) |
| PhGA (mm) | 18 (8-29) |
| mHAQ | 0.0 (0.0-4.0) |
| Anti-CCP antibodies at diagnosis (U/ml) | 69.2 (12.0-260.3) |
| RF (IU/ml) | 37.0 (9.0-129.3) |
| CRP (mg/dl) | 0.12 (0.05-0.36) |
| DAS28-CRP | 2.6 (1.8-3.1) |
| CDAI | 7.3 (3.6-13.0) |
Note: Values are presented as number (%) and median (interquartile range). TJC; Tender Joint Counts, SJC; Swollen Joint Counts, PtGA; Patient Global Assessment of Disease Activity, PhGA; Physician Global Assessment of Disease Activity, mHAQ; modified Health Assessment Questionnaire (mHAQ), CCP; Cyclic Citrullinated Peptide, RF; Rheumatoid Factor, CRP; C-reactive Protein, DAS28-CRP; Disease Activity Score Assessing 28 joints with CRP, CDAI; Clinical Disease Activity Index. *n=62 (63%), **n=90 (92%).
Table 1: Patient baseline (Week 0) characteristics (n=98).
Efficacy of the low gluten diet in overall patients
Table 2 shows the longitudinal changes in clinical variables associated with disease activity of overall patients. The level of PhGA was significantly improved at Week 8 and Week 16 when compared with data at Week 0. SJC28 was decreased at Week 16 when compared with that at Week 0 though there was no significance. There were no significant changes in the levels of TJC28, PtGA or mHAQ during the course. Concerning hematological data, a significant decrease of RF was detected at Week 16 (p=0.029 vs. at Week 8). CRP did not significantly change during the course. Of the composite measures, DAS28-CRP was significantly improved at Week 16 when compared with that at Week 0 and Week 8. CDAI was also significantly improved at Week 16 when compared with that at Week 0.
| Week 0 | Week 8 | p value | Week 16 | p value | p value | |
|---|---|---|---|---|---|---|
| (vs. Week 0) | (vs. Week 0) | (vs. Week 8) | ||||
| TJC 28 | 1.5 (0.0-3.3) |
1.0 (0.0-3.0) | 0.24 | 1.0 (0.0-2.0) | 0.222 | 1 |
| SJC 28 | 2.0 (0.0-4.0) |
1.0 (0.0-3.0) | 0.374 | 1.0 (0.0-4.0) | 0.061 | 1 |
| PtGA (mm) | 15 (7-27) |
15 (7-26) | 1 | 17 (5-29) | 1 | 1 |
| PhGA (mm) | 18 (8-29) |
10 (4-21) | <0.001 | 10 (4-19) | <0.001 | 1 |
| mHAQ | 0.0 (0.0-3.0) |
0.0(0.0-2.3) | 1 | 0.0 (0.0-3.0) | 1 | 1 |
| RF (IU/L) | 37.0 (9.0-129.3) |
40.5 (10.3-119.8) |
1 | 34.0 (8.8-114.8) | 0.081 | 0.029 |
| CRP (mg/dL) | 0.12 (0.05-0.36) |
0.12 (0.05-0.39) |
1 | 0.12 (0.05-0.42) | 1 | 1 |
| DAS28-CRP | 2.6 (1.9-3.1) |
2.4 (1.7-3.0) | 1 | 2.3 (1.6-2.9) | 0.004 | 0.011 |
| CDAI | 7.1 (3.8-12.5) |
6.5 (2.4-9.9) | 0.08 | 6.1 (2.5-9.9) | 0.02 | 1 |
Note: Values are presented as median (interquartile rage). TJC; Tender Joint Counts, SJC; Swollen Joint Counts, PtGA; Patient Global Assessment of Disease Activity, PhGA; Physician Global Assessment of Disease Activity, mHAQ; modified Health Assessment Questionnaire (mHAQ), RF; Rheumatoid Factor, CRP; C-reactive Protein, DAS28-CRP; Disease Activity Score Assessing 28 joints with CRP, CDAI; Clinical Disease Activity Index.
Table 2: Time course of clinical parameters in overall patients.
Figure 1 shows the longitudinal changes in percentages of overall patients who achieved remission or had LDA, MDA or HDA as determined by DAS28-CRP and CDAI scores. The proportion of patients achieving DAS28-CRP-defined remission or LDA was 56.1% of patients at Week 0, which was significantly increased to 64.3% at Week 8 and 69.4% at Week 16 (Figure 1A). Concerning CDAI disease activity, 61.2% of patients were in remission or LDA at Week 0, which was significantly increased to 74.5% at Week 8 and 74.5% at Week 16 (Figure 1B). We next examined the EULAR treatment response using DAS28-CRP score (Figure 2). The percentage of patients with a good or moderate EULAR response was significantly increased at Week 16 (25.5%) when compared with that at Week 8 (23.5%). There was significantly more percentage of patients with a good EULAR response at Week 16 (9.2%) than that at Week 8 (3.1%).
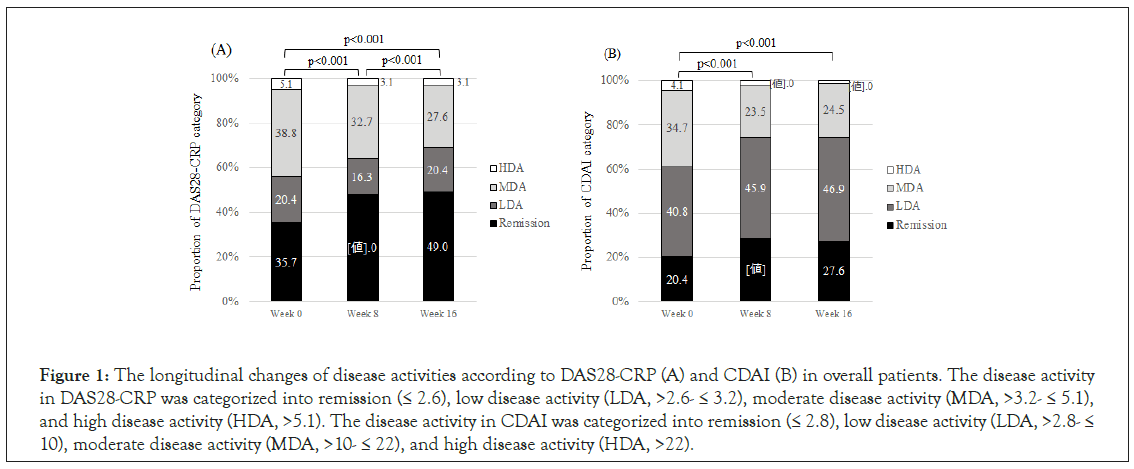
Figure 1: The longitudinal changes of disease activities according to DAS28-CRP (A) and CDAI (B) in overall patients. The disease activity in DAS28-CRP was categorized into remission (≤ 2.6), low disease activity (LDA, >2.6- ≤ 3.2), moderate disease activity (MDA, >3.2- ≤ 5.1), and high disease activity (HDA, >5.1). The disease activity in CDAI was categorized into remission (≤ 2.8), low disease activity (LDA, >2.8- ≤ 10), moderate disease activity (MDA, >10- ≤ 22), and high disease activity (HDA, >22).
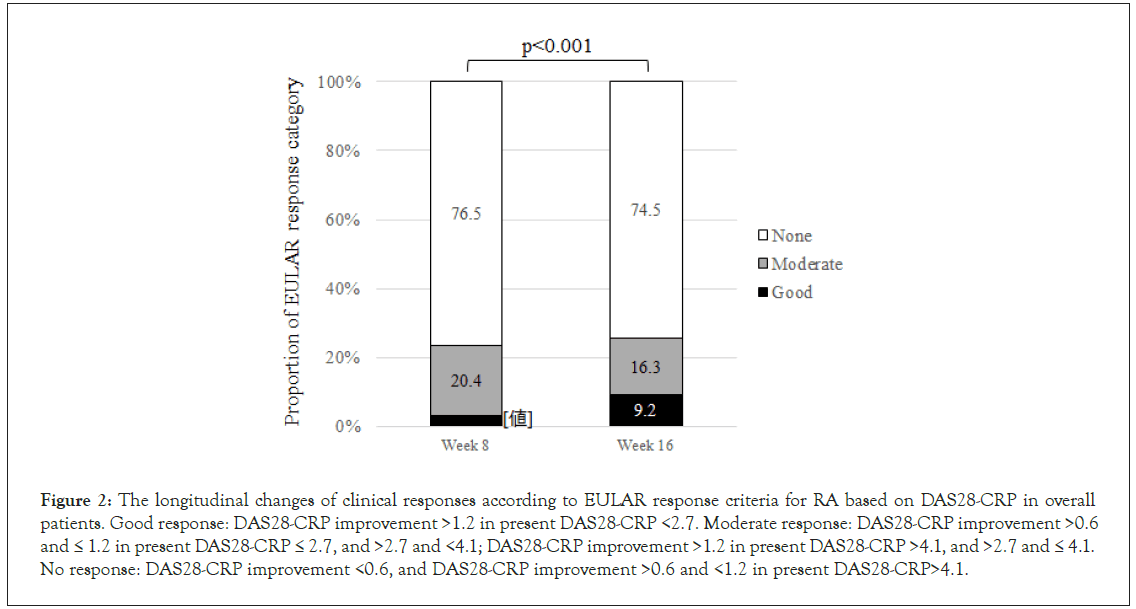
Figure 2: The longitudinal changes of clinical responses according to EULAR response criteria for RA based on DAS28-CRP in overall patients. Good response: DAS28-CRP improvement >1.2 in present DAS28-CRP <2.7. Moderate response: DAS28-CRP improvement >0.6 and ≤ 1.2 in present DAS28-CRP ≤ 2.7, and >2.7 and <4.1; DAS28-CRP improvement >1.2 in present DAS28-CRP >4.1, and >2.7 and ≤ 4.1. No response: DAS28-CRP improvement <0.6, and DAS28-CRP improvement >0.6 and <1.2 in present DAS28-CRP>4.1.
Comparison in efficacy among levels of adherence to the low gluten diet
To evaluate the effect of the low gluten diet on the disease activity of RA, patients were divided by the level of the low gluten into three categories; GLG, MLG, and PLG, and the longitudinal changes in the disease activities were compared among them. Of 98 patients, 39 (40%) were included in GLG, 39 (40%) in MLG, and 20 (20%) in PLG. There were no significant differences among three groups in gender, age, duration of disease, and clinical parameters at baseline (data not shown). Of the changes in composite measures, the level of DAS28-CRP was significantly decreased in patients with GLG and MLG but not in those with PLG at Week 16 when compared with that at Week 0 (Figure 3A). A significant improvement in DAS28-CRP was detected in patients with GLG (-0.18) and MLG (-0.21) but not in those with PLG (+0.17) at Week 16 when compared with at Week 0. An improvement in DAS28- CRP at Week 16 was significantly greater in GLG and MLG than in PLG (Figure 3B). A significant decrease in CDAI at Week 16 was detected only in patients with GLG when compared with that at Week 0 (Figure 3C). A significant improvement in the level of CDAI at Week 16 was detected in patients with GLG (-1.20) but not in those with MLG (-0.50) or PLG (+0.15) when compared with that at Week 0 (Figure 3D). These results indicated that the magnitude of improvement in the disease activity of RA was found to be dependent on the level of adherence to the low gluten diet. The serum levels of RF were significantly decreased at Week 16 in GLG [14.0 (5.3-82.8) IU/L] but not MLG or PLG when compared with those at Week 0 [16.0 (5.3-93.8)] (Figure 4). On the other hand, there was no significant difference in the serum level of CRP among all three diet groups during the course. PhGA at Week 16 was significantly decreased in GLG (p<0.001) and MLG (p=0.044) but not in PLG. Concerning other clinical parameters, TJC28, SJC28, PtGA and mHAQ, there were no significant changes during the course when the patients were divided into three diet categories (data not shown).
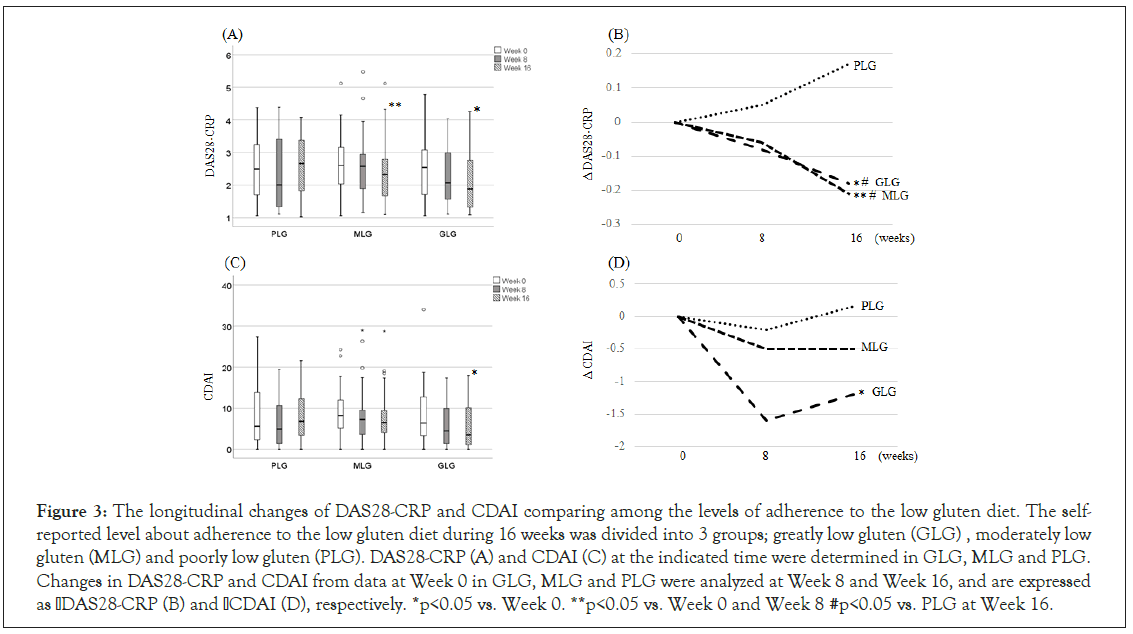
Figure 3: The longitudinal changes of DAS28-CRP and CDAI comparing among the levels of adherence to the low gluten diet. The self- reported level about adherence to the low gluten diet during 16 weeks was divided into 3 groups; greatly low gluten (GLG) , moderately low gluten (MLG) and poorly low gluten (PLG). DAS28-CRP (A) and CDAI (C) at the indicated time were determined in GLG, MLG and PLG. Changes in DAS28-CRP and CDAI from data at Week 0 in GLG, MLG and PLG were analyzed at Week 8 and Week 16, and are expressed as DAS28-CRP (B) and CDAI (D), respectively. *p<0.05 vs. Week 0. **p<0.05 vs. Week 0 and Week 8 #p<0.05 vs. PLG at Week 16.
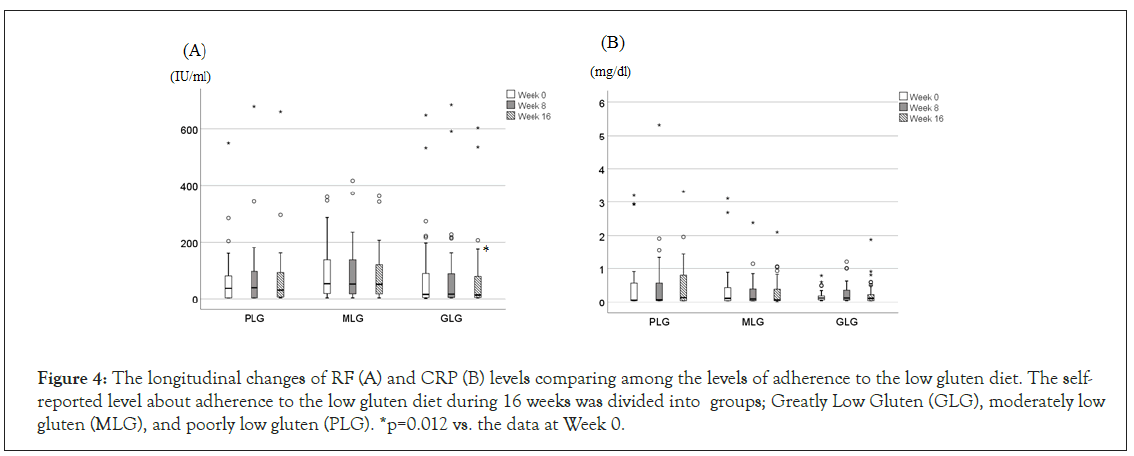
Figure 4: The longitudinal changes of RF (A) and CRP (B) levels comparing among the levels of adherence to the low gluten diet. The self- reported level about adherence to the low gluten diet during 16 weeks was divided into groups; Greatly Low Gluten (GLG), moderately low gluten (MLG), and poorly low gluten (PLG). *p=0.012 vs. the data at Week 0.
Discussion
This is a study composed of 16-week dietary interventions comprising a low gluten diet to patients with RA, and demonstrates that the low gluten diet improves the disease activity of RA. Two previous reports demonstrated that gluten free vegan diet significantly induces a clinical benefit for patients with RA [15,16]. However, their studies represented the combined effect of vegetarian diet and gluten-free diet. As far as we know, the present study is the first formal investigation which shows the efficacy of the diet with gluten-selective reduction for the suppression of the disease activity of RA.
The present study showed that the low gluten diet improved the clinical parameters concerning the activity of RA in overall patients. When the patients were further grouped into three categories (GLG, MLG and PLG) according to the level of subjective gluten exposure, a significant improvement in DAS28-CRP and CDAI at Week 16 was detected at in GLG and MLG, in GLG, respectively when compared with the data at baseline. These results suggest that intensively strict adherence to the low gluten diet leads to an improvement in the activity of RA.
The low gluten diet significantly improved composite measures concerning the activity of RA; DAS28-CRP and CDAI. Of the separate disease activity measures within DAS28-CRP and CDAI, the low gluten diet significantly improved PhGA but not PtGA. It decreased more SJC than TJC though the difference was not significant. Previous reports showed that main determinants for PtGA are pain, and those for PhGA are the number of SJC which contribute to the discrepancies between PtGA and PhGA in their perceptions [24,25]. Moreover, the present study showed that the low gluten diet did not decrease mHAQ score. These results suggest that the low gluten diet does not seem to lead to the improvement of joint pain or activities of daily life in patients with RA.
In laboratory tests, the low gluten diet resulted in a significant improvement in RF but not in CRP. RF is an autoantibody that binds to the Fc portion of human IgG and is frequently detected in patients with RA [26]. The positivity of RF as well as anti-CCP antibodies is used in the diagnosis of RA, and has been shown to predict a poor prognosis of joint damages and an inadequate response to therapy [27]. Thus, a decrease of RF observed in the low gluten diet may be related to an improvement of the disease activity and joint prognosis of RA. Although the mechanism of the decrease of RF by the low gluten diet is unknown, it is consistent with previous studies which showed that gluten-free diet confer some degree of protection from developing various autoantibodies [10,15]. Concerning CRP, the previous two studies investigated the change during gluten-free vegan diet [15,16]. A significant decrease in CRP with higher response rate at ACR20 is observed in RA patients with gluten free vegan diet after 1 year [15]. Similarly, gluten-free vegan diet reduces CRP at 12 months but not at 3 months though DAS28 and HAQ scores are decreased since 3 months [16]. Although these are studies which examined the combined effect of gluten-free and vegan diet, a decrease in CRP may need longer period diet such as one year than a period examined in the present study.
Gluten intake is a well-known triggering antigen that initiates immune reactions against small bowel cells in gluten sensitive diseases such as celiac disease [28,29]. Celiac disease is a genetically mediated autoimmune disease that can lead to malabsorption, infertility, osteoporosis, lymphoproliferative malignancy, and other autoimmune diseases [30,31]. Patients with celiac disease have been shown to be associated with various autoimmune disorders such as RA [12,31,32]. Increased prevalence of RF and anti-CCP antibodies positivity in patients with celiac diseases indicates that patients with celiac disease might be at a higher risk of developing RA [12]. Inversely, patients with autoimmune diseases have a significantly higher prevalence of celiac disease than the healthy population [31]. Thus, there are several similarities in the clinical findings between celiac disease and RA.
Since a lifelong gluten free diet has been considered the only effective treatment to celiac disease, several studies have investigated the mechanism of a gluten-free diet in the disease control of celiac disease [9,30,33,34]. Gluten-free diet is associated with reduced auto-inflammatory process and altered inflammatory cytokine response [33,34]. Strict adherence to gluten-free diet prevents the development of further autoimmune diseases in patients with celiac disease [9], and early exposure to gluten results in modifying the immunological response [30,31]. In RA, [15] showed that the IgG antibody levels against gliadin and betalactoglobulin decreased in the responder subgroup in the vegan diet free of gluten [15]. The gut may have a primary role in the inflammatory process in RA, and the change of the intestinal microflora and its metabolism may significantly contribute to the diminution of the rheumatoid symptoms [34]. These results suggest that immunological abnormalities in gastrointestinal tract due to gluten may be responsible for not only the development of celiac disease but also that of RA. However, whether the direct role of gluten exposure is directly associated with the development of autoimmune conditions in RA is still a matter of debate. Further studies are needed to clarify the mechanism of beneficial effect for the activity of RA due to a low gluten diet.
There is a previous report by [15] which investigated a long-term (1 year) trial of a vegan diet free of gluten, showing significantly higher ACR20 improvement in the diet group [15]. In their study, however, there were some limitations about the effect of gluten. Firstly, high rate of drop-outs (16 of 38, 42.1%) in the diet group was observed. Secondly, patients who changed the treatment of DMARDs and glucocorticosteroids during the study were included. Thirdly, their study may represent the combined effects of elimination in vegan diet and in gluten-free diet. Vegan (vegetarian) diet is a diet which include intake of only fruits and vegetables, eliminating any animal product or by-products [13,35]. It was shown to have the beneficial effect on disease activity of RA, and the mechanism has been well discussed [8,13,36-38]. The vegan diet decreases the counts of neutrophils, monocytes, complement components, CRP and RF in patients with RA, resulting in contributing to the pathogenesis of this disorder [13,36,37]. The improvements in the disease activity of RA by vegetarian diet might result from the reduction in the immune-reactivity to certain food antigens in the gastrointestinal tract [9]. These include the reduction of the bowel intraluminal antigenic load, alteration of the intestinal flora. All ultimately reduce the migration of lymphocytes from the intestinal lymphoid tissue to the synovium [38], and the changes in the gut system can influence the course of joint inflammation in RA [13]. Since vegan diet is associated with the low gluten to some extent, we speculate that the beneficial effect by the vegan diet on RA may result, at least in part, from the reduction of gluten.
There are several limitations to this study. Firstly, complete avoidance of gluten is difficult to be performed during the low gluten diet study. Plenty of products contain hidden gluten, such as soups, sausages, soy sauce and ice cream, and moreover there are traces of gluten even in gluten-free labeled products. Secondary, since this study was not double blind, the patients inevitably knew the level of a low gluten diet in them. Since the level of adherence to the low gluten diet was recorded by the patients subjectively but not objectively, it was difficult to avoid the pose of the patients in the study. Compliance in the diet trials is more difficult to verify than in drug ones [39].
Conclusion
RA is associated with a high health-care burden due to the expensive medical treatment. RA causes significant costs for society due to the increased use of healthcare resources, sick leaves and early retirements. Especially, costs of bDMARDs and tsDMARDs for RA are remarkably high though these medications have proven to be an effective treatment for this disorder. This study demonstrates that a low gluten diet suppresses the disease activity of RA which may encourage more research into the development of preventive strategies. Further longer time studies are needed to clarify the beneficial effect by a low gluten diet on the disease activity and joint prognosis of RA.
Author´s Contributions
KT, HT, YO and HY designed the study. KT, YO, SK, KK, KI, KI, AM, KK, and YN collected the data. KT, RT, TS and HY analyzed and interpreted the data. KT, HT, TS and HY performed statistical analyses. YO, SK and HY supervise the study. All authors have read and approved the final manuscript.
Ethics and Consent to Participate
The study protocol was approved by the Tokushima University Hospital Research Ethics Board. All patients provided written informed consent to participate.
Acknowledgements
The authors thank Ms. Yayoi Tagawa for her valuable secretarial support.
REFERENCES
- Shimizu T, Tani K, Hase K, Ogawa H, Huang L, Shinomiya F, et al. CD13/aminopeptidase N-induced lymphocyte involvement in inflamed joints of rheumatoid arthritis. Arthritis Rheum. 2002;46(9):2330-2338.
- Tani K, Shimizu T, Motoki Y, Sone S. Chemokines in synovial inflammation in rheumatoid arthritis: Basic and clinical aspects. Mod Rheumatol. 2002;12(2):93-99.
- Paul BJ, Kandy HI, Krishnan V. Pre-rheumatoid arthritis and its prevention. Eur J Rheumatol. 2017;4(2):161-165.
- Zamanpoor M. The genetic pathogenesis, diagnosis and therapeutic insight of rheumatoid arthritis. Clin Genet. 2019;95(5):547-557.
- Liao KP, Alfredsson L, Karlson EW. Environmental influences on risk for rheumatoid arthritis. Curr Opin Rheumatol. 2009;21(3):279-283.
- Honda K, Littman DR. The microbiota in adaptive immune homeostasis and disease. Nature. 2016;535(7610):75-84.
- Tani K, Kanamori M, Nagase Y, Okura Y, Kawaminami S, Kawahito K, et al. Past infections are associated with low levels of anti-citrullinated protein autoantibodies in rheumatoid arthritis. J Med Invest. 2020;67(1.2):182-188.
- Badsha H. Role of diet in influencing rheumatoid arthritis disease activity. Open Rheumatol J. 2018;12:19-28.
- Semerano L, Julia C, Aitisha O, Boissier MC. Nutrition and chronic inflammatory rheumatic disease. Joint Bone Spine. 2017;84(5):547-552.
- Lauret E, Rodrigo L. Celiac disease and autoimmune-associated conditions. Biomed Res Int. 2013.
- Sainsbury K, Halmos EP, Knowles S, Mullan B, Tye-Din JA. Maintenance of a gluten gree diet in Coeliac disease: The roles of self-regulation, habit, psychological resources, motivation, support, and goal priority. Appetite. 2018;125:356-366.
- Lerner A, Matthias T. Rheumatoid arthritis-celiac disease relationship: joints get that gut feeling. Autoimmun Rev. 2015;14(11):1038-1047.
- Kjeldsen-Kragh J, Mellbye OJ, Haugen M, Mollnes TE, Hammer HB, Sioud M, et al. Changes in laboratory variables in rheumatoid arthritis patients during a trial of fasting and one-year vegetarian diet. Scand J Rheumatol. 1995;24(2):85-93.
- Sköldstam L, Hagfors L, Johansson G. An experimental study of a Mediterranean diet intervention for patients with rheumatoid arthritis. Ann Rheum Dis. 2003;62(3):208-214.
- Hafström I, Ringertz B, Spangberg A, von Zweignergk L, Brannemark S, Nylander I, et al. A vegan diet free of gluten improves the signs and symptoms of rheumatoid arthritis: The effects on arthritis correlate with a reduction in antibodies to food antigen. Rheumatology (Oxford). 2001;40(10):1175-1179.
- Elkan AC, Sjoberg B, Kolsrud B, Ringertz B, Hafström I, Frostegard J. Gluten-free vegan diet induces decreased LDL and oxidized LDL levels and raised atheroprotective natural antibodies against phosphorylcholine in patients with rheumatoid arthritis: A randomized study. Arthritis Res Ther. 2008;10(2):R34.
- Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315-324.
- Kasturi S, Goldstein BL, Malspeis S, Karlson EW, Costenbader KH. Comparison of the 1987 American College of Rheumatology and the 2010 American College of Rheumatology/European League against Rheumatism criteria for classification of rheumatoid arthritis in the Nurses’ Health Study cohorts. Rheumatol Int. 2014;34(3):407-411.
- Nozaki Y, Inoue A, Kinoshita K, Funauchi M, Matsushima I. Efficacy of iguratimod vs. salazosulfapyridine as the first-line csDMARD for rheumatoid arthritis. Mod Rheumatol. 2020;30(2):249-258.
- Matsumoto T, Matsui T, Hirano F, Tohma S, Mori M. Disease activity, treatment and long-term prognosis of adult juvenile idiopathic arthritis patients compared with rheumatoid arthritis patients. Mod Rheumatol. 2020;30(1):78-84.
- Harigai M, Ishiguro N, Inokuma S, Mimori T, Ryu J, Takei S, et al. Safety and effectiveness of abatacept in Japanese non-elderly and elderly patients with rheumatoid arthritis in an all-cases post-marketing surveillance. Mod Rheumatol. 2019;29(5):747-755.
- Van Gestel AM, Prevoo ML, Hof MA, Van Rijswijk MH, Van de Putte LB, Van Riel PL. Development and validation of the European League Against Rheumatism response criteria for rheumatoid arthritis. Comparison with the preliminary American College of Rheumatology and the World Health Organization/International League against Rheumatism Criteria. Arthritis Rheum. 1996;39(1):34-40.
- Takahashi N, Kojima T, Kida D, Kaneko A, Hirano Y, Fujibayashi T, et al. Clinical effectiveness and long-term retention of abatacept in elderly rheumatoid arthritis patients: Results from a multicenter registry system. Mod Rheumatol. 2019;29(6):910-918.
- Kaneko Y, Takeuchi T, Cai Z, Sato M, Awakura K, Gaichi C, et al. Determinants of patient's global assessment of disease activity and physician's global assessment of disease activity in patients with rheumatoid arthritis: A post hoc analysis of overall and Japanese results from phase 3 clinical trials. Mod Rheumatol. 2018;28(6):960-967.
- Studenic P, Radner H, Smolen JS, Aletaha D. Discrepancies between patients and physicians in their perceptions of rheumatoid arthritis disease activity. Arthritis Rheum. 2012;64(9):2814-2823.
- Ingegnoli F, Castelli R, Gualtierotti R. Rheumatoid factors: Clinical applications. Dis Markers. 2013;35(6):727-734.
- Santos-Moreno P, Sanchez G, Castro C. Rheumatoid factor as predictor of response to treatment with anti-TNF alpha drugs in patients with rheumatoid arthritis: Results of a cohort study. Medicine. 2019;98(5).
- Rostami K, Bold J, Parr A, Johnson MW. Gluten-free diet nidications, safety, quality, labels, and challenges. Nutrients. 2017;9(8):846.
- Itzlinger A, Branchi F, Elli L, Schumann M. Gluten-free diet in celiac disease-Forever and for all? Nutrients. 2018;10(11):1796.
- El-Chammas K, Danner E. Gluten-free diet in nonceliac disease. Nutr Clin Pract. 2011;26(3):294-299.
- Sategna-Guidetti C, Solerio E, Caglione N, Aimo G, Mengozzi G. Duration of gluten exposure in adult coeliac disease does not correlate with the risk for autoimmune disorders. Gut. 2001;49(4):502–505.
- Koning F, Thomas R, Rossjohn J, Toes. Coeliac disease and rheumatoid arthritis: similar mechanisms, different antigens. Nat Rev Rheumatol. 2015;11(8):450-461.
- Fayyaz B, Gunawan F, Rehman HJ. 'Preclinical' rheumatoid arthritis in patients with celiac disease: a cross-sectional study. J Community Hosp Intern Med Perspect. 2019;9(2):86-91.
- Podas T, Nightingale JMD, Oldham R, Roy S, Sheehan NJ, Mayberry JF. Is Rheumatoid arthritis a disease that starts in the intestine? A pilot study comparing an elemental diet with oral prednisolone. Postgrad Med J. 2007;83(976):128-131.
- Rostami K, Bold J, Parr A, Johnson MW. Gluten-free diet indications, safety, quality, labels, and challenges. Nutrients. 2017;9(8):846.
- McDougall J, Bruce B, Spiller G, Westerdahl J, McDougall M. Effects of a very low-fat, vegan diet in subjects with rheumatoid arthritis. J Altern Complement Med. 2002;8(1):71-75.
- Lederer AK, Maul-Pavicic A, Hannibal L, Hettich M, Steinborn C, Grundemann C, et al. Vegan diet reduces neutrophils, monocytes and platelets related to branched-chain amino acids-A randomized, controlled trial. Clin Nutr Actions. 2020.
- Khanna S, Jaiswal KS, Gupta B. Managing rheumatoid arthritis with dietary interventions. Front Nutr. 2017;4:52.
- Yuasa S, Yamaguchi H, Nakanishi Y, Kawaminami S, Tabata R, Shimizu N, et al. Treatment responses and their predictors in patients with rheumatoid arthritis treated with biological agents. J Med Invest. 2013;60(1.2):77-90.
Citation: Tani K, Takagishi H, Okura Y, Kawaminami S, Kawahito K, Inaba K, et al. (2020) A Low Gluten Diet Suppresses Disease Activity of Rheumatoid Arthritis. J Vaccines Vaccin. S7:001.
Copyright: © 2020 Tani K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.