Indexed In
- The Global Impact Factor (GIF)
- CiteFactor
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Virtual Library of Biology (vifabio)
- International committee of medical journals editors (ICMJE)
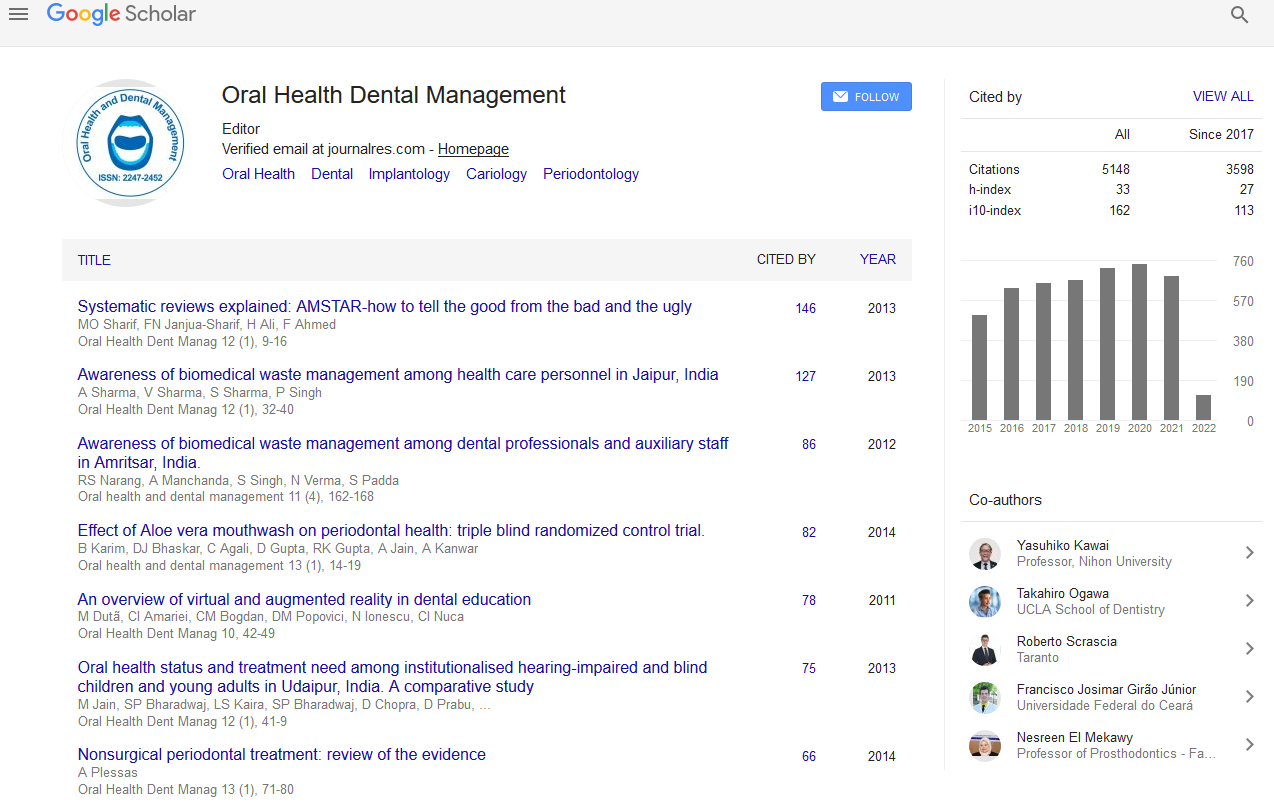
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Short Communication - (2021) Volume 20, Issue 8
A Brief Idea about Oral Tolerance Therapy in an Experimental Model of Colitis
Jerem Smith*, DOI: 10.35248/2247-2452.21.20.1148
Abstract
Oral tolerance can be characterized from an immunological and clinical perspective. Immunologically, oral resistance is an antigenexplicit concealment of cell and humoral reactions to dietary and bacterial antigens after openness in the gastrointestinal lot. Clinically, oral resistance is the capacity to eat food without growing immunologically intervened side effects regardless of the recurrence and amount of food burned-through. There are various aggregates of oral resistance to food sources. Most food-open minded people don't foster immunoglobulin E refinement to food varieties; be that as it may, some do and a subset of these foster clinical food sensitivity.
Keywords
Oral tolerance therapy, Oral management, Oral health.
About the Study
Oral organization of protein antigens instigates fundamental invulnerable resistance [1,2]. The two instruments hypothesized to intervene oral resistance are energy and dynamic insusceptible concealment. The acceptance of energy is best shown in the wake of taking care of high-portion oral antigen, which brings about practical inactivation or potentially erasure of antigen-explicit T cells. By correlation, concealment is seen after numerous low-portion antigen taking care of. Exploratory information propose that insusceptible concealment is accomplished through administrative cytokines, for example, TGF-b, IL-10, and IL-4. Immune system microorganisms creating these administrative cytokines may down regulate autoreactive T cells in an antigen vague way. This is useful in conditions like provocative inside infection (IBD), in which pathogenic autoantigens have not been recognized. In the recent concern, Ilan et al. [3] address whether oral organization of colonic antigens downregulates inflammationin a rodental model of Trinitrobenzene Sulfonic corrosive (TNBS)- instigated colitis.
The creators reason that taking care of colonic concentrate proteins (CEP) prompts silencer T cells that intercede resilience to tissue antigens. The end depended on the regulation of TGF-b in tolerized rodents and the supposition that exchange of T cells from "lenient rodents" smothered exercises of endogenous T cells in beneficiary rodents. In any case, it is hard to decide the number of endogenous T cells stayed in lighted beneficiaries. Without endogenous T cells, it is conceivable that giver T cells from "lenient mice" neglected to incite colitis in view of prior energy or safe deviation of cells toward a less pathogenic, T assistant sort 2 aggregate (e.g., one that makes IL-4 and IL-10). For concealment to be illustrated, they will need to show proof that cytokines from benefactor cells downregulated effector cells significant for colitis. Moreover, if concealment happened in beneficiary mice, the job of TGF-b should be concentrated in more detail. By and large, the receptive exchange information are reminiscent of a suppressive instrument yet will require more investigation if unthinking ends are to be reached.
In the article, homogenized colonic proteins from colitic rodents were utilized to actuate oral resistance. Organization of TNBS and ethanol douches initiates broad mucosal harm portrayed by edema, discharge, epithelial shedding, and invasion of polymorphonuclear leukocytes [4]. Albeit the creators didn't break down colonic concentrates, one accepts that follower microorganisms were likewise present in a combination of proteins containing mucosal fiery cells and epithelial cells alongside TNBS itself. Proof to help a job of inside verdure in the pathogenesis of IBD is growing [5]. In this manner, one chance is that bacterial proteins in the CEP blend assisted with inciting resilience to pathogenic bacterial strains. Further investigation will be expected to decide the significance of bacterial antigens in the pathogenesis just as resistance of intestinal irritation in patients with IBD.
In the article by Ilan et al. [3], it is conceivable that resilience was produced to the hapten used to create illness, as this was in all probability in the CEP. Beforehand, Neurath et al. utilized TNBS-haptenized colonic proteins to incite oral resistance in TNBS-instigated colitis [6]. In the Neurath study, numerous taking care of haptenized colonic proteins forestalled weight reduction in mice given CD41 lamina propria T cells from colitic mice. The significance of these prior information was the showing that oral resistance could downregulate exercises of beforehand enacted T cells. Be that as it may, these past creators didn't prompt oral resistance in mice with continuous colitis. The aftereffects of the current paper by Ilan et al. [3] add to our comprehension of the space, as theshow that oral resistance treatment downregulates colitis after illness beginning. This development is clinically pertinent, as it proposes that oral resistance might be valuable as a treatment for dynamic IBD patients. Generally speaking, the original copy by Ilan et al. [3] gives significant insights to the quest for a kindhearted, nontoxic treatment that utilizes oral proteins to downregulate ruinous tissue irritation in the inside.
Conclusion
The significance of these prior information was the showing that oral resistance could downregulate exercises of beforehand enacted T cells. Be that as it may, these past creators didn't prompt oral resistance in mice with continuous colitis.
REFERENCES
- Weiner HL. Oral tolerance: Immune mechanisms and treatment of autoimmune diseases. Immunology Today. 1997;18(7):335-343.
- Mowat AM, Faria AM, Weiner HL. Oral tolerance: Physiologic basis and clinical applications. InMucosal immunology. Academic Press. 2005;487-537.
- Ilan Y, Weksler-Zangen S, Ben-Horin S, Diment J, Sauter B, Rabbani E, et al. Treatment of experimental colitis by oral tolerance induction: A central role for suppressor lymphocytes. Am J Gastroenterol Suppl. 2000;95(4):966-973.
- Morris GP, Beck PL, Herridge MS, Depew WT, Szewczuk MR, Wallace JL. Hapten-induced model of chronic inflammation and ulceration in the rat colon. Gastroenterology. 1989;96(2):795-803.
- Sartor B. The role of luminal bacteria in colitis: More than an antigenic drive. European Journal of Clinical Investigation. 1998;28(12):1027-1029.
- Neurath MF, Fuss I, Kelsall BL, Presky DH, Waegell W, Strober W. Experimental granulomatous colitis in mice is abrogated by induction of TGF-beta-mediated oral tolerance. Exp Med. 1996;183(6):2605-2616.