PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
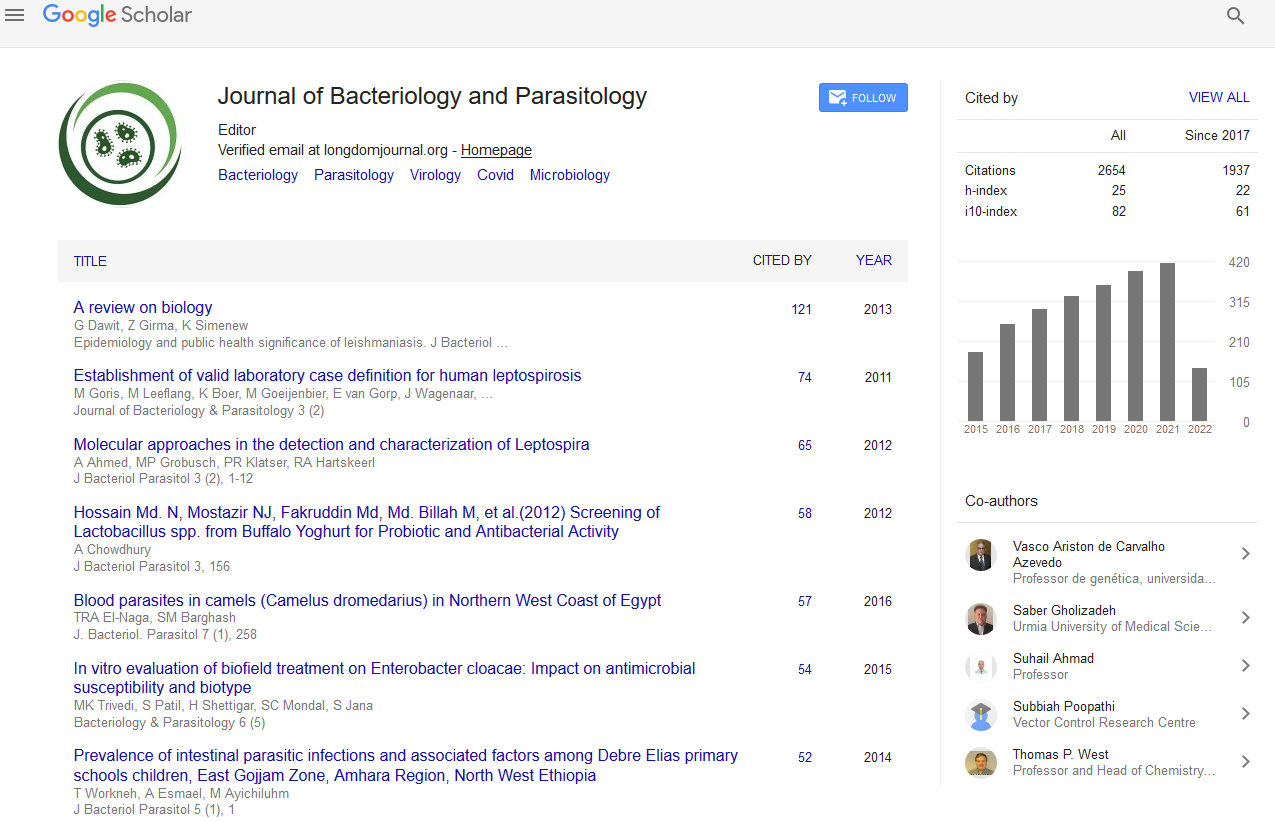
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Treatment Outcome of Tuberculosis Patients and Associated Risk Factors at Dessie and Woldiya Town Health Institutions, Northeast Ethiopia: A Retrospective Cross Sectional Study
Asmamaw Malede, Agumas Shibabaw, Elifaged Hailemeskel, Mulugeta Belay and Seyfe Asrade
Background: Ethiopia introduced directly observed therapy short-course (DOTS) strategy for TB in 1995; reaching its full coverage in 2005. Treatment success rate (TSR) was 84% in 2009 and dropped to 83% in 2010. Despite the progress made in tuberculosis control throughout Ethiopia, risk factors leading to poor treatment outcome have not been assessed in Dessie and Woldiya town health institutions. Therefore, this study aimed to determine treatment outcome of TB patients and risk factors for poor treatment outcome in Dessie and Woldiya town health institutions, Northeast Ethiopia.
Methods: A three years (September 2010 to August 2012) retrospective study was conducted from medical records of 1511 TB patients at Dessie and Woldiya town health institutions. Data were collected using a questionnaire that consists of patients’ age, sex, weight, TB history, TB type, HIV status, availability of supporter, availability of mobile number, drug type and TB treatment outcomes in treatment cards and TB logbook from February, 2013 to April, 2013. Pearson chi-square test and logistic regression were employed for data analysis.
Results: From 1511 TB patients, 1,331(88.1%) were successfully treated, 123 (8.1%) died, 45 (3.0%) defaulted and 12 (0.8%) failed from treatment. In terms of TB type, 57.4% were pulmonary TB, 40.5% were extra pulmonary TB and 2.1% were both smear negative pulmonary and extra pulmonary TB. In addition, TB-HIV co-infection rate was 42.9% in 2010, with significant reduction in 2012 (33.7%) (P<0.01). Multivariate logistic regression showed the odds of successful treatment outcome was higher among females (AOR=2.09, 95% CI: 1.27-3.45), new TB patients (AOR=10.52, 95% CI: 3.96-27.93), patients with unknown HIV status (AOR=7.16, 95% CI; 1.56-32.75) and HIV negative (AOR=1.80, 95% CI: 1.09-2.99) when compared with the respective comparison groups. The odds of defaulting was higher among TB patients started treatment in Dessie Health Center (AOR=4.09, 95% CI: 1.33-12.60) and combined smear negative pulmonary and extra pulmonary TB disease (AOR=8.87, 95% CI: 2.53-31.02) compared with the respective comparison groups.
Conclusions: Treatment success rate of TB patients in this study was very encouraging for TB control through DOTS strategy. Nevertheless, TB patients with HIV/AIDS, combined smear negative pulmonary and extra pulmonary TB and with previous history of TB were found to be at risk of poor treatment outcome. Correspondingly, male TB patients and those who attend health centers should be encouraged for successful treatment outcome. Generally, to reduce poor treatment outcome, patients should be strictly followed by health extension workers or trained community health workers in Dessie and Woldiya town health institutions.