PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
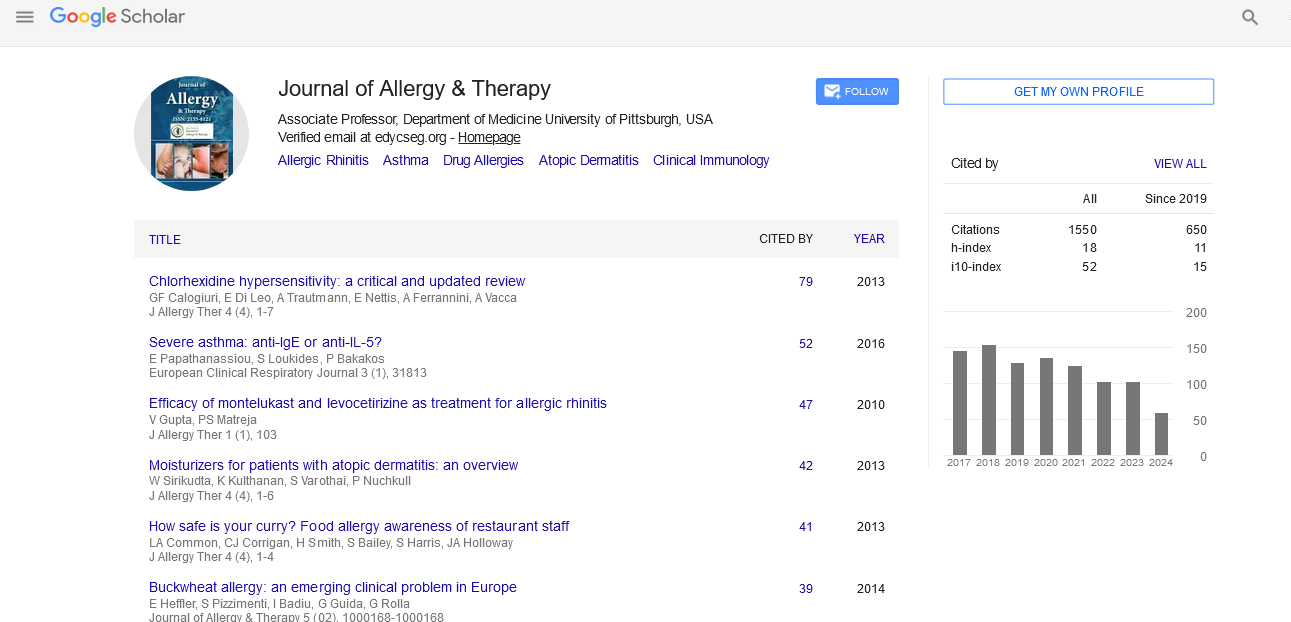
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Treatment after Accidental Injection with Epinephrine Autoinjector: A Systematic Review
Background: Epinephrine (adrenaline) autoinjectors are increasingly prescribed for the emergency management of severe allergic reactions. There is an increasing incidence of unintentional administration of these devices, typically into a digit. Digital epinephrine has theoretical dangers of ischemia and gangrene and multiple interventions have been advocated in the treatment of these unintentional administrations of epinephrine.
Objective: This systematic literature review examines available evidence about unintentional epinephrine digital injections, in order to advise appropriate treatment.
Methods: Systematic searches were made of electronic databases (Medline, EMBASE, Scopus), reference screening and forward citation searching. Application of inclusion and exclusion criteria: Findings of included articles were summarized and data analyzed.
Results: This literature review found limited published material on the topic. Four observational studies (retrospective cohort studies) and seven case series have been published, along with a number of single case reports. The data described complete recovery of almost all (greater than 99%) patients exposed to a digital epinephrine injection by autoinjector- regardless of treatment. Most patients received no pharmacological treatment. Case reports suggest that recovery may be quicker with use of subcutaneous phentolamine or terbutaline than with observation or conservative treatment. A small number of patients (from one database and one case series) suffered long term or severe effects from the digital epinephrine injection.
Conclusion: There is a growing body of evidence suggesting that accidental injection with epinephrine autoinjector may be managed conservatively in most cases. Evidence to date suggests conservative treatment (observation and/or local heat) will result in full recovery in the vast majority of patients. Treatment with locally injected phentolamine or terbutaline appears to rapidly reverse vasconstriction. There have been a small number of reports of incomplete recovery. This limited evidence needs to be interpreted with caution due to potential selection bias and misclassification. Further observational and randomized experimental research is needed to determine when pharmacological treatment is indicated and if it improves patient outcomes. Patient and carer education about proper use of individual autoinjector devices is the best prevention for these events.