PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
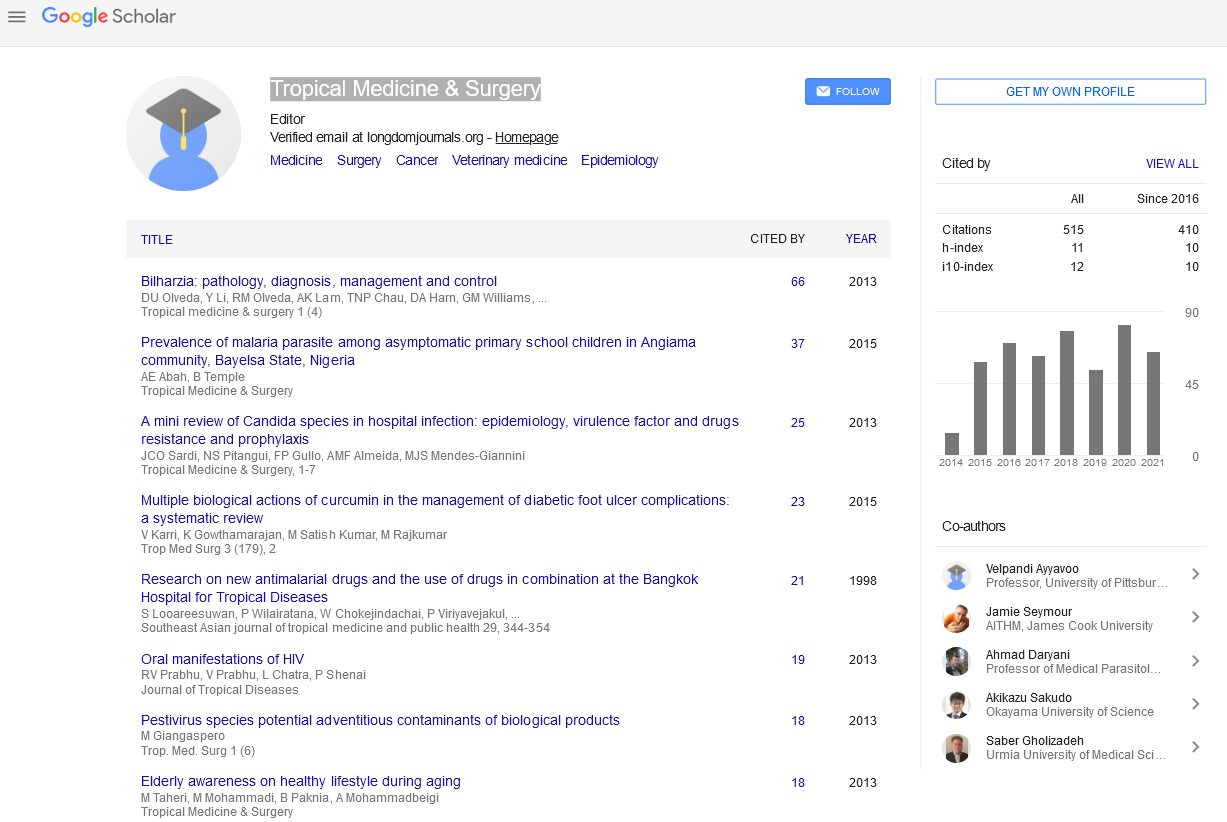
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Social Determinants of the Impact of Surgical Disease on Health
Sara L Doorley, Noemi C Doohan, Sindhura Kodali and Kelly McQueen
Population distributions and patterns have evolved over time to emphasize urbanization and globalization. These realities have not been favorable for public health. Similarly patterns of disease have evolved, causing the global burden of disease to change considerably in the last 20 years. Chronic disease and non-communicable disease has replaced infectious disease as the largest contributor to global disability and death. The leading causes of death now include cardiovascular disease, trauma and cancer, and maternal mortality continues to be unacceptably high. The disease patterns emerging require a new approach to diagnosis, treatment and follow up. Non-communicable disease including trauma and cancer, as well as some infectious disease and maternal conditions may be treated, cured or palliated with surgical intervention. These interventions, when immediately available, decrease disability and premature death associated with these conditions. But a majority of this disease occurs in low-income countries where, up until recently, there were few options for surgery and safe anesthesia. The advent of datum supporting the practical and cost-effective role of surgery within global public health mandates a change in planning and delivery of healthcare services in low-income countries. The social determinants of health are well-identified contributors to the health of a population, and certainly impact the outcomes of surgical disease in low-income countries. These factors, nutrition, education, poverty, governance, gender, housing and transportation must be considered and addressed in a new era of non-communicable disease where emergency and essential surgery must be available to insure population health.