Indexed In
- Open J Gate
- JournalTOCs
- The Global Impact Factor (GIF)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
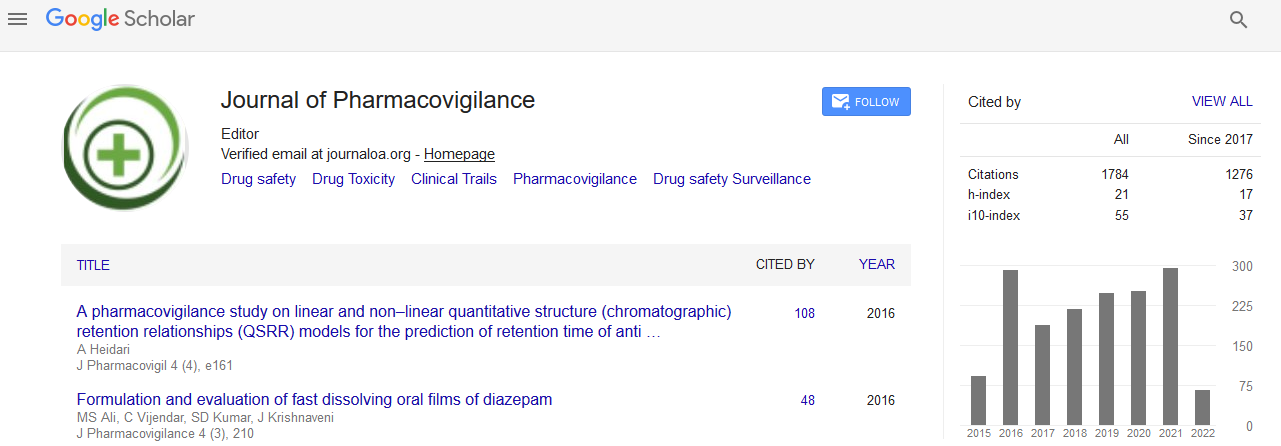
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Serious Adverse Events Reporting and Follow-Up Requirements in the European and Developing Countries Clinical Trials Partnership-Funded Clinical Trials: Current Practice
Jean Marie Vianney Habarugira, Antonia Agustà and Michael Makanga
Background: This study aimed to assess the current pharmacovigilance practice and compliance with the International Committee for Harmonization Good Clinical Practice (ICH-GCP) requirements within a range of clinical trials funded by the European and Developing Countries Clinical Trials Partnership (EDCTP).
Methods: A combination of a retrospective desk review of projects documentation as of June 2014 and a prospective survey among EDCTP-funded clinical trials investigators were used.
Results: The overall survey response rate was 64.3%. Among the 54 trial investigators who responded to the survey, 64% are sponsored by academic institutions, 25% by public research institutions, and 6% by Product Development Partnerships (PDPs). 77% of the Sponsors are based in Europe, 17% in Africa and 6% are globalbased institutions. 75% of the respondents confirmed occurrence and reporting of Serious Adverse Events (SAEs) in their trials. The primary reference document for SAEs reporting and follow up reported as % of clinical trials are clinical trial protocols (81.5%), SOPs for handling SAEs (50%) and investigator brochure (11%). The average SAE reporting time by 81% of respondents within 24 hours, 11% within 48 hours, 4% within 7 days and 2% between 7 and 15 days. Majority (79.6%) of investigators report SAEs directly to the their trial Sponsors, 62.3% to National Ethics Committees (NECs) and Institutional Review Boards (IRBs), 33.3% to the national regulatory authorities (NRAs), 22.2% to the safety monitors, and 3.7% to the Contract Research Organisations (CROs). Combinations of these recipients were reported by several respondents. Among the 41 respondents who reported SAEs occurrence in their trial, only 22 confirmed that they are required to report to their NECs and IRBs. 85% of respondents send SAEs reports by e-mail, 27.8% by Fax mail, 11.1% by telephone and 9.3% as printed hard copies.
Conclusion: A majority of respondents (75%) confirmed that SAEs have occurred in their trials; in this group, 45% of respondents did not confirm the requirement of reporting SAEs to local oversight bodies. It is important that both NECs and NRAs in all countries where clinical trials are conducted clearly make available their reporting requirements to the investigators to ensure adequate compliance with local reporting requirements. Further studies are necessary to better understand the magnitude of this problem and to strengthen capacity of local trial oversight by NECs and NRAs.