PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
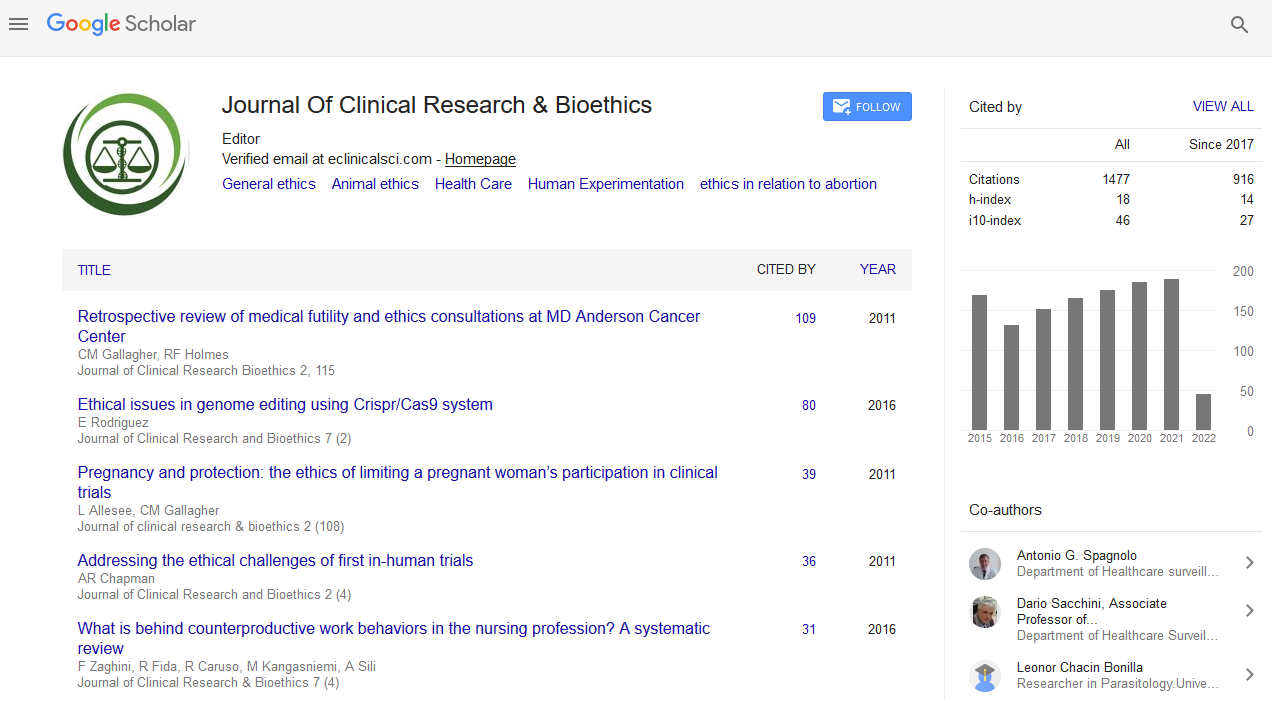
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Safety, Efficacy, Regulations and Bioethics in Herbal Medicines Research and Practice
David Nzioka Mutua, Juma KK, Munene M and Njagi ENM
Herbal medicines are used by about 80% of the populations in Africa. Despite being the main management strategy for a number of medical conditions, few studies have been done to suggest their toxicity and efficacy. Moreover, herbal medicines are not prescriptive. Users commonly find information from relatives, and friends. The classification of plant herbal medicines as complementary and alternative medicines also remains to be recognised as nutritional products. This therefore presents a special bioethical challenge in both research and practice for both researchers and medical physicians. Research on herbal medicines also demonstrates the lack of consistency in repeatability and reproducibility of their findings. Some studies have also established efficacy while others demonstrate otherwise. Variation in their findings has been attributed to variations in geographical locations of sources of plant materials and soil diversity. Moreover, ethical consideration in research may not have the appropriate social value, validity in research, risk benefit ratio and collaborations required for ethical sustainability. This may be as a result of the different cultures and traditions in the use of plant materials among different communities. In addition, ethical principles such as beneficence and no malfeasance may not be sustainable for all the medical physicians using plant herbal medicines in the management diseases in patients. The patient autonomy is also not valid table from the existing toxicity and safety studies. More research on bioethics is needed to bridge the gap between ethics, research and practice for herbal medicines.