Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Euro Pub
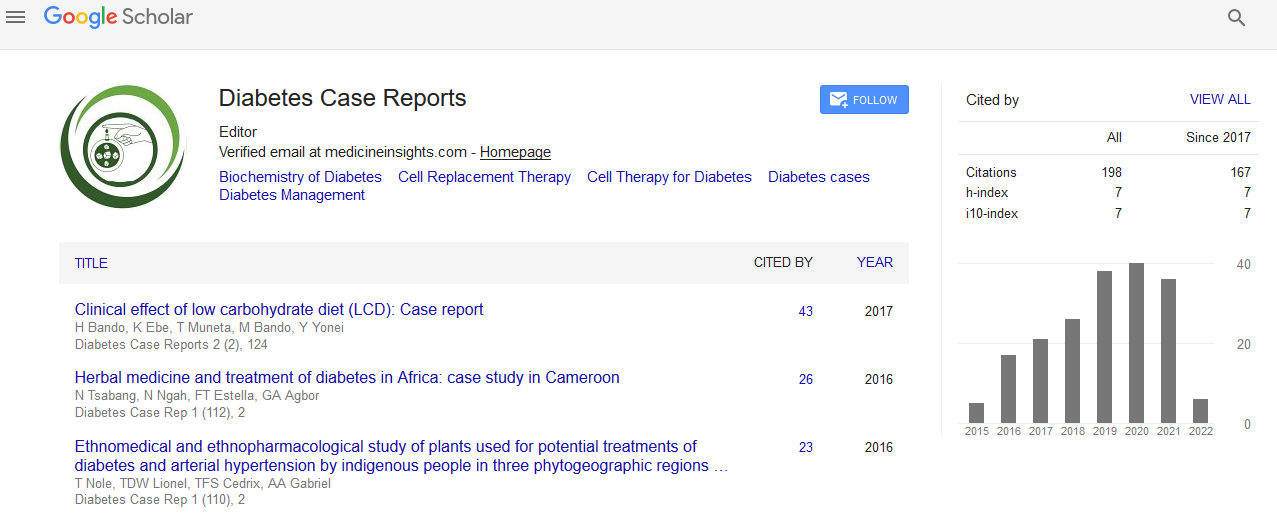
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Safety and efficacy of cord stem cell transplantation forthe treatment of type 2 Diabetes Mellitus
Lipi Singh
Abstract
Background: A combination of insulin resistance and pancreatic beta cell mass defects appears to be involved in the aetiology of Type 2 diabetes (T2DM). Further, glucotoxcity and lipotoxicity leads to increased beta cell apoptosis and affects insulin release associated with an increased oxidative stress and inflammation. This concept has given a way to cellular therapies, particularly stem cell therapies aimed at protecting beta cell mass and its regeneration. Cord stem cell therapies (mesenchymal stem cells) are emerging set of therapies with promising outcomes and very low incidence of adverse effects. Thus, we have speculated in our pilot study that mesenchymal stem cell infusion could be the treatment option for T2DM by stimulating beta cell differentiation and capable of endogenous pancreatic tissue regeneration. The main aim of our pilot investigation was to assess the safety of cord stem cell in T2DM patients and further ascertain the efficacy of mesenchymal stem cell in metabolic control with reduction in HbA1c and with improvement in beta cell function (c-peptide), contributing to reduction of OHA and insulin requirements.
Methods: A total of 10 patients (06 male and 04 female aged 35 years to 62 years) from October 2016 to November 2017 with T2DM for 5-6 years, failure of triple oral anti diabetes drugs, receiving Insulin (> 0.6 U/kg/Day) at least for one year, HbA1c (8.48 ± 0.36) were included in this study. They underwent catheter based target delivery of cord stem cells through a transfemoral route into superior pancreaticoduodenal artery under fluoroscopic guidance. Clinical variables (body mass index, duration of diabetes, insulin requirement, oral hypoglycaemic drugs, duration free from insulin/oral drugs), and laboratory test variables were assessed over period starting at baseline and up to 12 months follow up post stem cell infusion. The primary outcome measures were reduction of insulin requirement by ≥ 50% by the end of 3 months of cord stem cells infusion and improvement in Glucagon stimulated C - peptide levels while secondary endpoints were reduction insulin dosage, HbA1c level at the end of 12 months. Follow ups were performed at the 30, 90,180, 360 days after mesenchymal stem cell infusion.
Results: Six male and four female patients were enrolled in this study. Baseline variables expressed as Mean ± SEs. Clinical variables and laboratory variables were calculated during follow ups in all patients after mesenchymal stem cell therapy and compared to baseline. Six patients (60%) out of ten patients were responders and showed a reduction in insulin requirement by 60% to 75% as compared to baseline in 3 to 6 months post stem cell infusion. Two patients (20%) were able to discontinue insulin completely with suggested nutritional diet and physical exercise with 12 months follow ups. There was a significant improvement in both fasting and stimulated cpeptide level in the group (p≤0.005) and responders (p≤0.005) in 6 months. Mean HbA1c reduction was 1% to 2.4 % as compared to baseline in 45 days to 6 months and 4 out of 16 responders had HbA1C value ≤7 %. HOMA-B increased significantly in the group (p≤0.05) and responders (p≤0.05) whereas HOMA-IR did not change significantly. Fasting plasma glucose reduced significantly from 142±10.5 to 120±7.1; p≤0.05 in whole group and in responders from 135.5+8.5 to 110+4.5; p≤0.05 while, fasting plasma insulin increased non-significantly in group and responders as well. No serious adverse events were noted in our study.
Conclusion: Cord stem cell infusion resulted in a significant decrease (60%-75%) in the insulin requirement, reduction in HBA1C level (2.4 %), increase stimulated C- peptide levels over a period of 3 months to 6 months. The safety and efficacy of cord stem cell is maintained over a period of 12 months without any serious adverse events.