PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
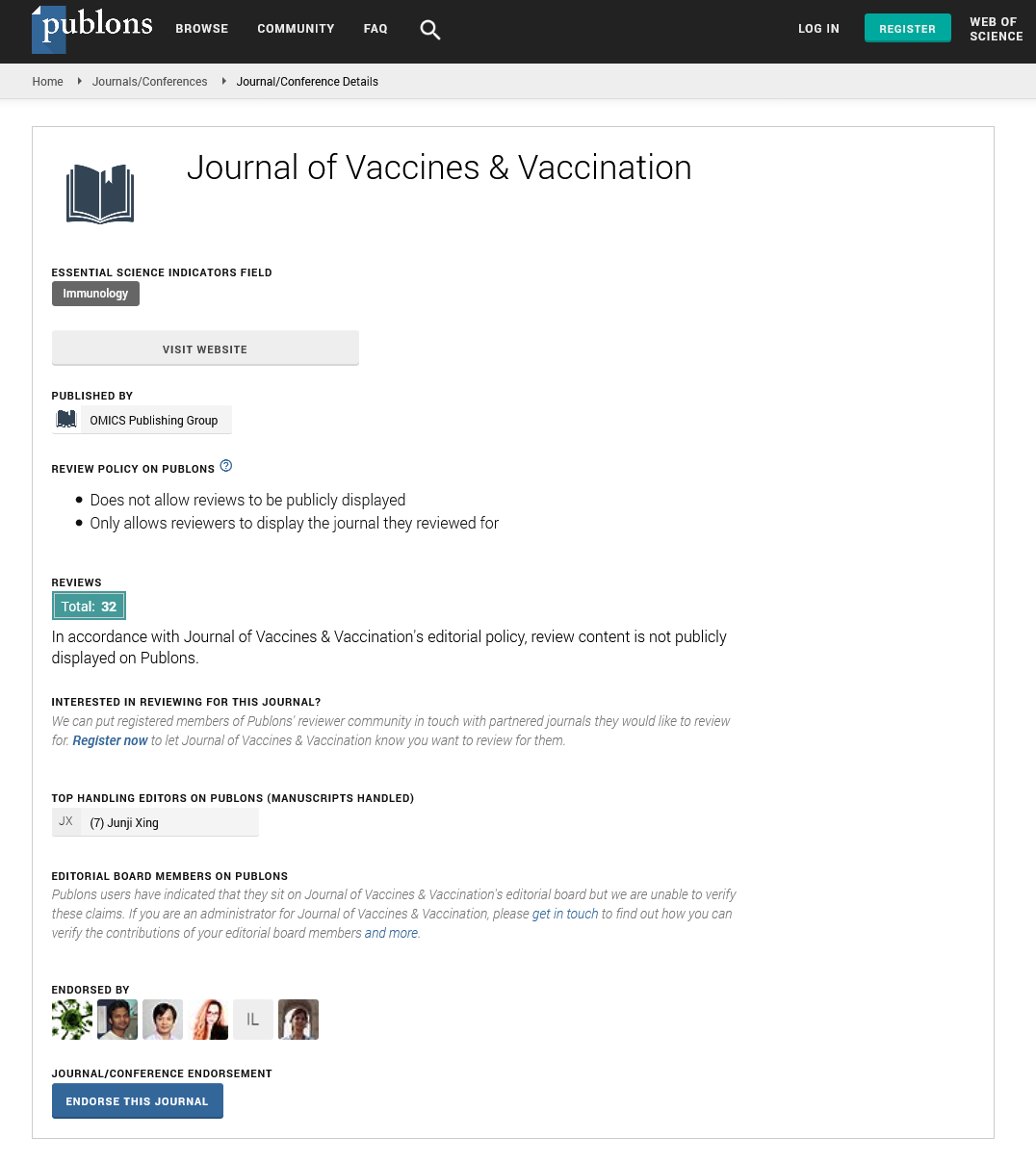
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
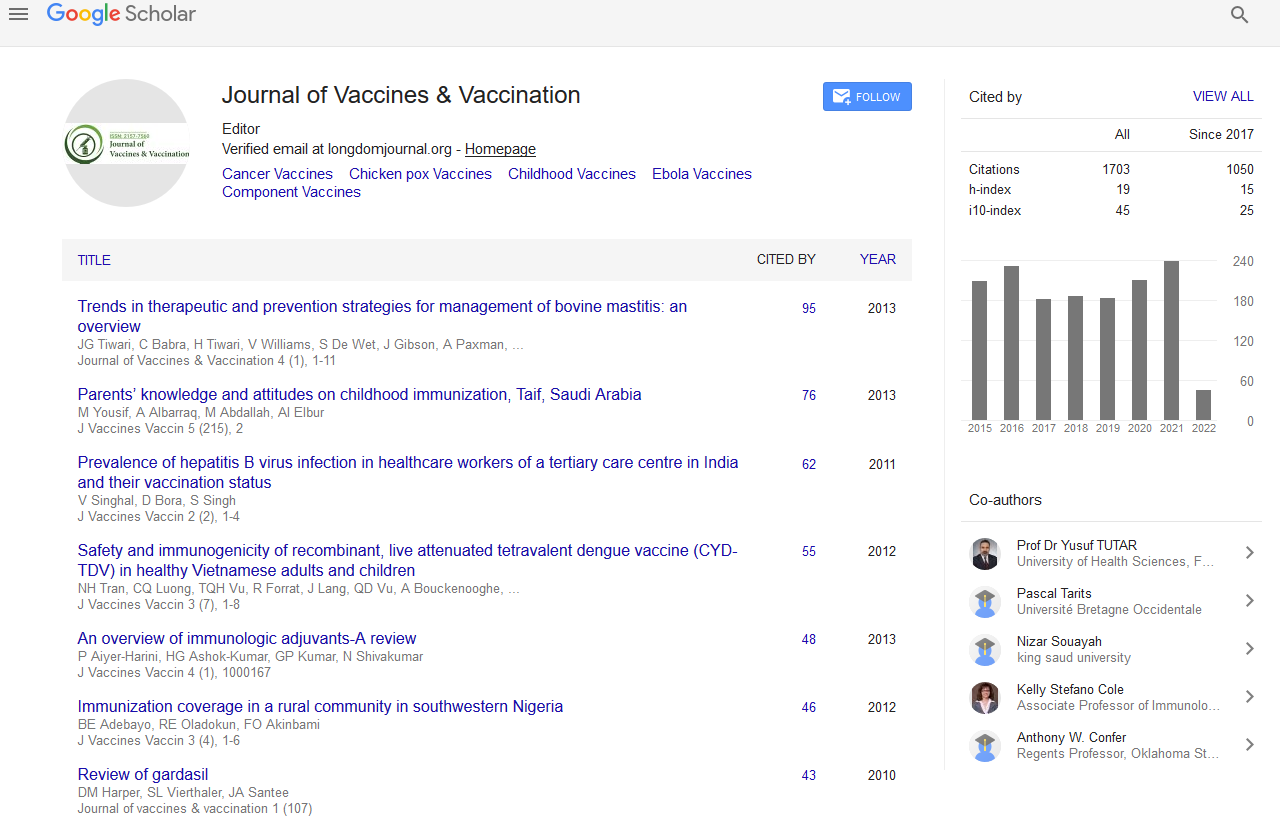
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Retinoic Acid Promotes Mucosal and Systemic Immune Responses after Mucosal Priming and Systemic Boosting in Mice
Elisa Cirelli, Antonella Riccomi, Filippo Veglia, Valentina Gesa, Maria Teresa De Magistris and Silvia Vendetti
Objective: Few mucosal vaccines are available for human use, none of which are recombinant proteins or subunits of pathogens, owing to the lack of potent and safe mucosal adjuvants. Given the crucial role of retinoic acid (RA) in favouring dendritic cell differentiation, imprinting a mucosal homing capacity on T and B cells, as well as its potential to promote the differentiation of IgA-producing plasma cells, we evaluated the capacity of RA to improve mucosal vaccinations.
Study design: BALB/c mice were treated for eight days with RA or its vehicle and then intranasally immunized with tetanus toxoid (TT) with or without CT and boosted three times. Alternatively, mice treated with RA or its vehicle, were exposed to intranasal delivery of TT alone and boosted systemically with TT and Alum. Serum and mucosal Ag-specific antibody responses were examined 2 weeks and 8 months after the priming.
Results: Treatment with RA synergises with the adjuvant capacity of CT to enhance both systemic and mucosal TT-specific antibody responses. The combination of mucosal priming with Ag alone, followed by a boost with systemic adjuvant was also evaluated. Mice treated with RA showed a higher titer of mucosal IgA compared to untreated mice, after intranasal priming with TT followed by a systemic boost with TT plus Alum. After eight months, higher IgG TT-specific antibodies in the serum and a higher frequency of TT-specific IgG and IgA secreting cells were detected in the bone marrow of mice treated with RA as compared to untreated mice. Higher percentages of proliferating CD4 and CD8 T cells upon TT stimulation were found in the spleens, in the mesenteric lymph nodes and in the colonic lamina propria of mice treated with RA.
Conclusion: This approach induces mucosal immunity in the absence of mucosal adjuvants and improves the effectiveness of mucosally-delivered vaccine.