Indexed In
- Open J Gate
- Genamics JournalSeek
- CiteFactor
- Cosmos IF
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Proquest Summons
- Scholarsteer
- ROAD
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
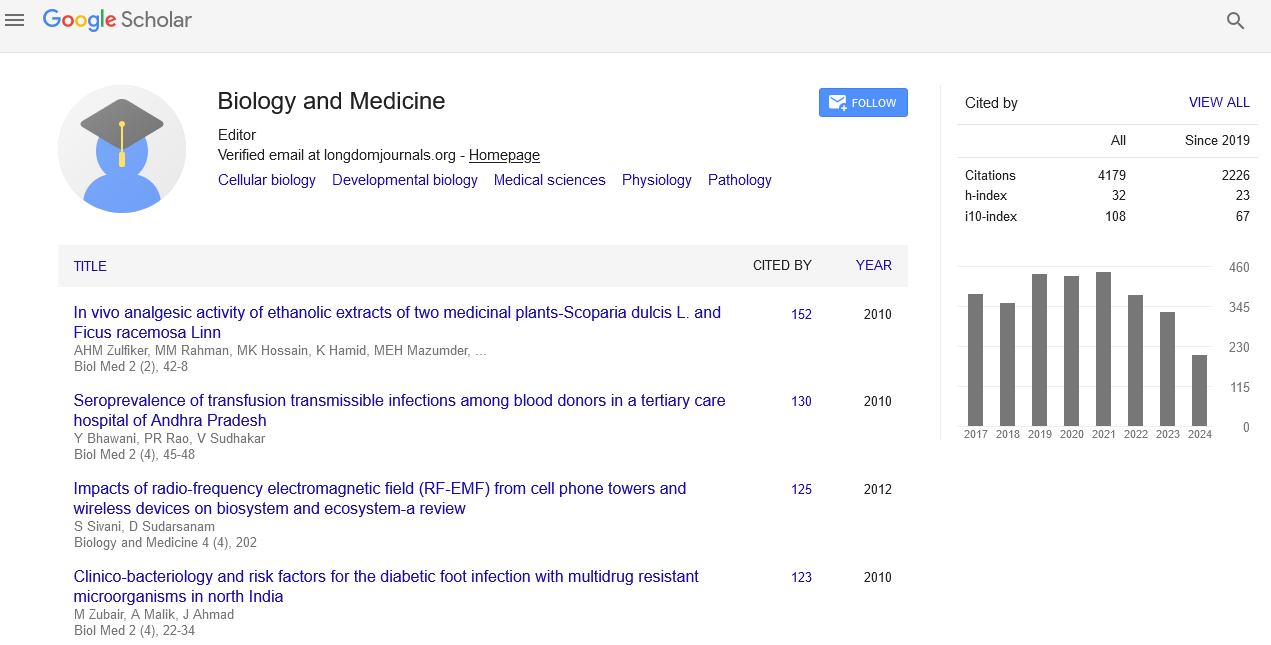
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Restoration of Innate Immune Responses may be a Novel Therapeutic Strategy for Treatment of Chronic Hepatitis C Virus Infection
Yutaka Kishida, NaohikoImaizumi, Hirohisa Tanimura, YoshimichiHaruna, Masahumi Naitoh, Shinichiro Kashiwamura and Toru Kashiwagi
HCV persistence results from inefficient innate and adaptive immune responses. We investigated whether an induction approach (IA) with natural (n) IFN-beta followed by Peg IFN-alpha and ribavirin (Standard of Care; SOC) (novel combination treatment; NCT) increased the virologic response and restored innate and adaptive immune responses in chronic hepatitis C (CHC) patients with HCV genotype 1b and a high viral load. Seven CHC patients were treated with NCT. NCT overcame viral escape and breakthrough, resulting in persistent viral clearance. Early virologic responders (EAVR, n=5) with undetectable HCVRNA before the end of IA showed a sustained virologic response (SVR). Late VR (LAVR, n=2) with undetectable HCVRNA after the end of IA showed a transient VR. IL-15 was increased at the end of IA in both EAVR and LAVR. CXCL-8, CXCL-10, CCL-4, and CCL-11 levels were significantly decreased (p<0.05) in EAVR, but were not in LAVR during NCT. IL-12 increased significantly (p<0.05) and CXCL-8 decreased significantly (p<0.05) after the end of NCT in EAVR, but did not in LAVR. The present study suggested that the initial early virologic clearance induced by CPIT before the use of SOC induced the restoration of DC function and improvements in the activation of NK cells, as indicated by the up-regulation of IL-12 and IL-15 and down-regulation of CXCL-8, CXCL-10, CCL-4, CCL-11. Early virologic clearance by IA with nIFN-beta induced the restoration of innate immune responses linked to adaptive immune responses, which resulted in SVR. NCT (n=8) achieved a higher SVR rate than that of SOC (n=8) in difficultto-treat CHC patients. The results showed the safety of the nIFN-beta treatment and supported the use of nIFN-beta as a safe and alternative option. NCT is more effective and have less adverse effects than SOC in difficult-to-treat CHC patients with genotype 1b and a high viral load