Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Proquest Summons
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Euro Pub
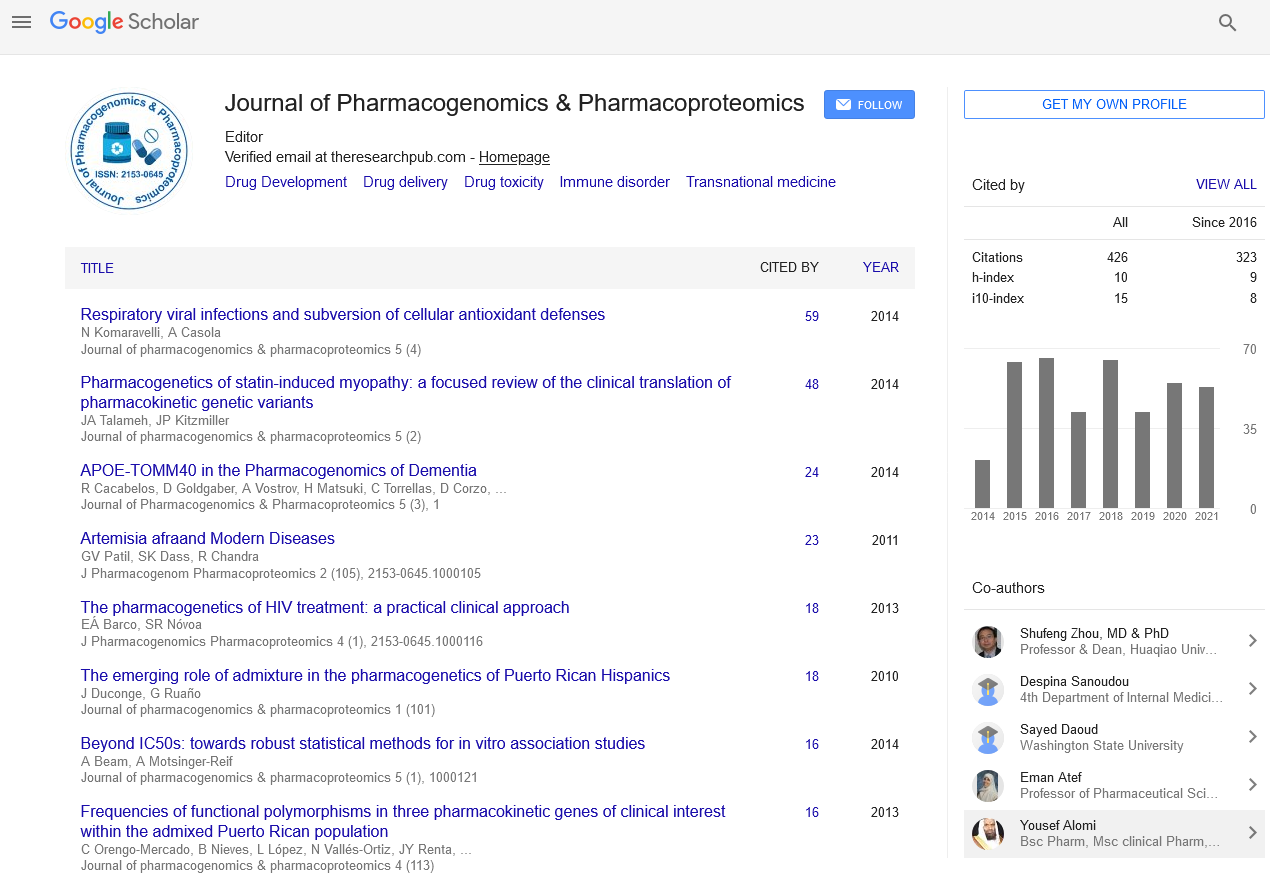
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Personalized Medicine for Severe Asthma: How Far Have We Achieved?
Ting F Leung, FAAAAI, Man F Tang and Gary WK Wong
There is increasing pharmacogenetic literature on the heterogeneity in the treatment responses to different anti-asthma drugs including inhaled corticosteroid (ICS), which are indicated for patients with moderate-to-severe asthma. A number of genetic targets including STIP1, CRHR1, CYP3A4, GLCCI1, T gene and FBXL7 are potential pharmacogenetic biomarkers for predicting patients’ response to ICS. Knowledge on predictive variants in these genes allows for the genotyping and selection of patients with severe asthma for personalized treatment with high-dose ICS treatment. There is an emerging trend to unravel genetic variants that predict treatment responses among patients with different asthma endotypes. Some patients with severe asthma are refractory to maintenance corticosteroids, and several biological agents targeting type 2 helper T lymphocyte pathway offer hope of optimizing their disease control. The efficacy of subcutaneous pitrakinra is dependent on patients’ IL4R status. Nonetheless, such pharmacogenetic effect has not been investigated for other biological agents such as mepolizumab. The adoption of a personalized pharmacogenetic approach to health care delivery facilitates the optimal use of novel, expensive and potentially toxic therapies in patients with severe asthma.
Asthma is characterized by airway inflammation, and is caused by complex interactions between many genetic and environmental factors. Anti-inflammatory therapies such as inhaled corticosteroid (ICS) are therefore an integral component of asthma pharmacotherapy under different international guidelines. There is substantial inter-individual variability in patients’ response to anti-asthma treatments. According to Global Initiative for Asthma guideline, patients with severe controlled asthma require maintenance oral corticosteroid or anti-immunoglobulin E treatments. A number of biologic agents have recently been shown to be treatment alternatives for these patients. Pharmacogenetic approach facilitates personalized medicine by differentiating treatment responders from nonresponders, whereby substantially reducing the economic burden of asthma. Candidate gene and pathway-based pharmacogenetic methods have identified a number of candidate genes and their functional variants, but largerscale pharmacogenomics has drawn more and more attention over the past decade. Our group has previously discussed the genetic targets for bronchodilator responses to β2-agonists and leukotriene modifiers. This editorial focused on recent advances in the pharmacogenetics of ICS and the novel biological agents as treatment modalities for patients with severe asthma.