Indexed In
- Open J Gate
- JournalTOCs
- The Global Impact Factor (GIF)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
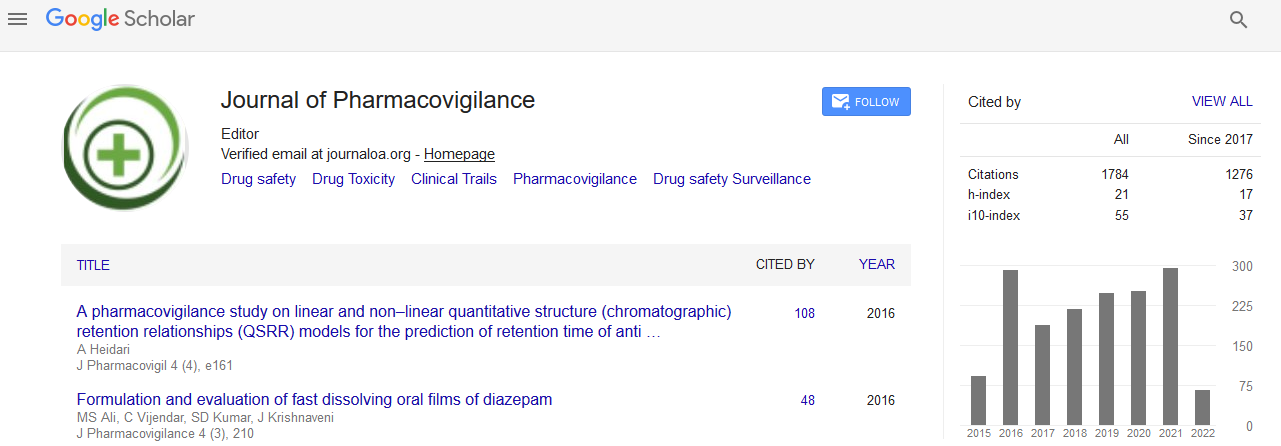
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Non-Ergot Dopamine Agonists don't Increase the Risk of Heart Failure in Parkinson's disease Patients. A Meta-Analysis of Randomized Controlled Trials
Renato De Vecchis, Claudio Cantatrione, Damiana Mazzei and Cesare Baldi
Background: In recent years, some observational studies suggested that pramipexole, a non-ergot dopamine agonist (DA) used for the treatment of Parkinson’s disease (PD), may increase the risk of heart failure (HF). However, the limitations inherent in observational studies made it difficult to determine whether the excess of incident HF was related to the drug or to other determinants. Thus, some concerns remained regarding the increased putative HF risk associated with non-ergot DAs as a class or individually.
Method: In our meta-analysis, primary endpoint was the risk of incident HF in patients with PD treated with non-ergot DAs compared to those treated with monotherapy with levodopa. Secondary outcome measures were all-cause mortality and cardiovascular events. For these purposes, only randomized controlled trials (RCTs) were considered, provided that they offered complete outcome data pertaining to the incident HF, all-cause mortality and risk of cardiovascular events. Systematic searches were performed in the databases of PubMed, Embase and ClinicalTrial.gov up to May 2015. The effect size was estimated using the pooled relative risk (RR) of non-ergot DAs versus placebo on incident HF as well as on all-cause mortality or cardiovascular events.
Results: Six out of 27 RCTs reported at least one case of incident HF; therefore, we included them in the RR estimate, whereas 13 RCTS were included in the meta-analysis for mortality rates and 22 RCTs were included to evaluate cardiovascular events. Treatment with non-ergot DAs did not reveal an increase in the risk of incident HF as compared with the placebo group (pooled RR: 0.95, 95% CI: 0.30–2.90; p = 0.893). Similarly, patients treated with non-ergot DAs didn’t show any significant differences compared to controls with regard to all-cause mortality (pooled RR: 0.617, 95% CI: 0.330–1.153; p = 0.13) as well as with regard to cardiovascular events (pooled RR: 1.067, 95% CI: 0.663–1.717; p = 0.789).
Conclusion: The use of non-ergot DAs in PD patients was not associated with an increased risk of incident HF, nor was it shown to increase the overall mortality or the risk of cardiovascular events compared to the PD patients taking monotherapy with levodopa alone. However, larger studies are warranted to confirm the cardiovascular safety of non-ergot DAs for PD management.