Indexed In
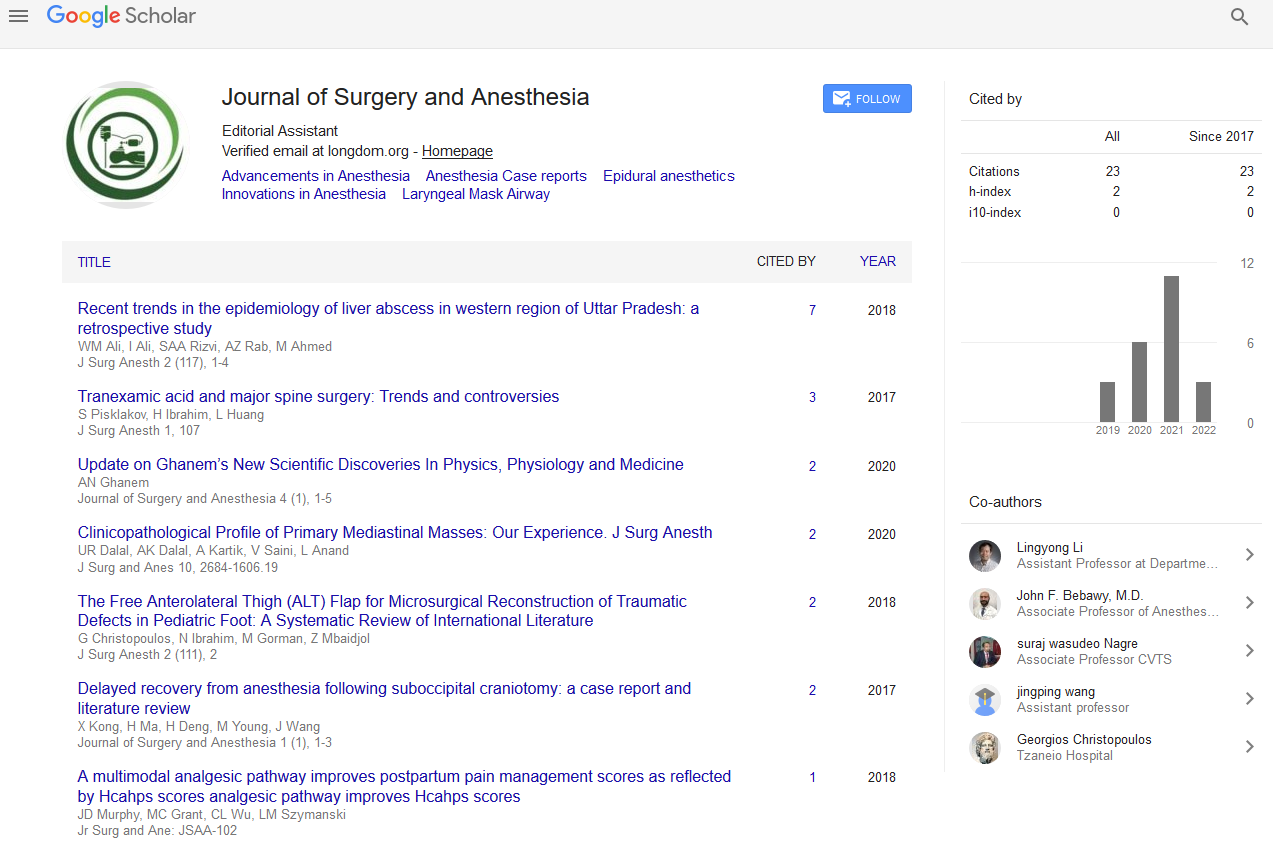
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Improved Post-Resuscitation Survival Time with Adjuvant Cytosolic Energy Replenishment in a Murine Model of Hemorrhagic Refractory Shock
El Rasheid Zakaria, Bellal Joseph, Faisal S Jehan, Muhammad Khan, Abdelrahman Algamal, Faheem Sartaj, Muhammad Jaffar Khan and Rajvir Singh
Objective: A refractory haemorrhagic hypovolemic shock (HS) resuscitation is challenging. HS is associated with profound depletions of cellular energy nucleotides that can cause death from a cardio-circulatory arrest. To prevent an imminent cardio-circulatory arrest, vasopressors, commonly norepinephrine is usually temporarily administered to manage a persistent hypotension that is not corrected by aggressive resuscitation efforts. The objective of this study is to determine the post-resuscitation survival time after adjuvant resuscitations of a refractory HS with norepinephrine, vasopressin or direct cytosolic energy (adenosine-5`-triphosphate, ATP) replenishment using lipid vesicles encapsulating ATP (ATPv).
Methods: 50 male Sprague-Dawley rats were randomized to 5 groups of 10 each: HS/conventional resuscitation (CR), HS/CR+Norepinephrine, HS/CR+Vasopressin, HS/CR+Vesicles, and HS/CR+ATPv. (HS=initial removal of 30% of the calculated blood volume, a 60 min hypotensive phase, and a subsequent transection of the spleen for uncontrolled haemorrhage until persistent shock index (SI)>5 and mean arterial pressure (MAP)<35 mmHg were achieved; CR=shed blood returned+double the shed blood volume as lactated Ringer’s solution). Direct cytosolic ATP replenishment was accomplished with ATPv, which are highly fusogenic lipid vesicles encapsulating ATP. Fusion of the ATPv with the cell membrane on contact, allows for direct cytosolic ATP delivery. We determined the post-resuscitation survival time as the end-point of the study.
Results: All animals displayed the same class of shock as demonstrated by the SI and MAP. Median postresuscitation survival times (computed by the Kaplan-Meier survival curves and the long-rank Mantel-Cox test) were as follows: HS/CR=35.5 min; HS/CR+Norepinephrine=38.5 min; HS/CR+Vasopressin=20 min; HS/CR+Lipid Vesicles control=88.5 min; and HS/CR+ATPv=158.5 min (p<0.001).
Conclusion: The replenishment of the depleted cellular cytosolic energy stores in a refractory haemorrhagic hypotensive shock prolongs post-resuscitation survival time and delays cardio-circulatory arrest. This buys time for the initiation of definitive resuscitation protocols. Cellular energy failure appears to contribute to the pathogenesis of shock refractoriness to resuscitation efforts. The temporary administration of vasopressors for pressure-support resuscitation of a refractory haemorrhagic hypovolemic shock exerts no survival benefits.